Post-discharge Health Outcomes of Aboriginal Patients
Info: 8611 words (34 pages) Dissertation
Published: 4th Feb 2022
Tagged: HealthInformation Systems

Outcome Evaluation of the effect of an Aboriginal Health Linking Information database on remote area discharge planning from metropolitan hospitals for Aboriginal patients living in the Pilbara and Kimberley regions of Western Australia.
Executive Summary
Health outcomes of the Aboriginal population in the Pilbara and Kimberly areas of Western Australia are much poorer than non-Aboriginal populations and when looking at hospitalisations and emergency department presentations for these two regions, we see not only a large disparity between populations, but also a significant number of hospital patients have had to be treated in Perth. A web based Aboriginal health linking information tool in the form of a database was developed with the aim of improving the patient discharge process and the post-discharge patient journey for Aboriginal patients from Perth hospitals back to their remote homes. It will be trialed in the remotes Western Australian regions of Pilbara and Kimberley initially. Dependent on an outcome evaluation and understanding of the unintended consequences, it has the potential to be rolled out across Australia.
Table of Contents
Introduction and Background
Program Summary
Case Example
The Evaluand
Program Logic
Purpose of the Evaluation
Intended Audience and Stakeholders
Key Evaluation Questions
Outcome Evaluation Design, Methodology and Analysis
Limitations
Ethical Issues
Timeline
Budget
Dissemination of Outcome Evaluation
References
Introduction and Background
A focus for Australian state and federal governments is to close the 10-year life expectancy gap between Aboriginal and non-Aboriginal Australians.1 Australia’s Aboriginal population have a higher burden of disease,2 reflective of both the social determinants of health, like their environment, social and economic disadvantage, in addition to deficient access to health services.3 Nearly two thirds of Western Australia’s Aboriginal people live in remote or very remote locations with limited health care and access to services.4 Both the Pilbara and Kimberly regions of Western Australia are considered very remote.
The Pilbara has a population of 66,298 of which, 15% are Aboriginal and there are twenty-six different spoken dialects.5 The Pilbara region represents approximately 20% of Western Australia’s land mass, covering over 500,000 km2 and is the second most northern region after the Kimberley. To put the size into perspective, it is almost twice the size of the Victorian state and nearly three times the size of the United Kingdom.5 The main industry of Pilbara is mining with most of the population living in Karratha, Pert Hedland and Newman.5 It has a very transient population of fly in/fly out workers, estimated to be 28,000 people in 2012.5 When comparing the non-Aboriginal population to the Aboriginal population, the Pilbara region has a higher proportion of females and a younger age structure, 80% are aged 45 and under.6 However, as an overall population, it has a 5% higher proportion of male residents than the state average of 51%.6
The Kimberley in 2013 had a population of 39,890 of which, 44% are Aboriginal and spread over one hundred communities with fifteen different dialects spoken.7 It is the state’s most northern region with an area of 424,517km2. Broome, Kununurra, Derby, Wyndham, Fitzroy Crossing and Halls Creek is home to most of the population.7 It also has a large transient population due to mining being its largest industry. The Kimberly, similarly to the Pilbara, has a younger age structure of Aboriginal population compared to non-Aboriginal and has a higher level of disadvantage compared to other regions.8
Along with poorer health outcomes and high levels of social and economic disadvantage compared to non-Aboriginal populations in these two regions2 a disparity also exists when looking at hospitalisations and emergency department presentations for these two regions. A significant percent of patients are treated in Perth hospitals, which can be financially costly on the health systems and an imposition on Aboriginal patients and their families.
2003- 2013 Hospitalisations for 15-64 years
The Pilbara had 71,806 (120,785 per 100,000) hospitalisations. This is six times higher than the non-Aboriginal population in Pilbara and 10% higher than the Aboriginal state rate.6
The Kimberly had 155,544 (142,413 per 100,000) hospitalisations, which is six times higher than the non-Aboriginal population in Kimberly and 28% higher than the Aboriginal state rate.8
2013/2014 Emergency Department Attendances
The Aboriginal population made up 30% of the overall Pilbara hospital emergency department attendances with 59,233 in total. Of that 30%, 25% of Aboriginal patients were transported to attend emergency departments of Perth hospitals.6
While in the Kimberley, Aboriginal emergency department attendances was 59,233, representing 57% of all attendances with 17% of Aboriginal attendances needing to be seen at Perth hospital’s emergency departments.8
With both the Pilbara and Kimberley regions comprise a large area with a relatively low population within, it creates a challenge for the delivery and accessibility of health services. Evidence supporting increasing disparities in post-discharge health outcomes 9-11 is suggestive of a tool needed for better discharge planning that considers the cultural needs of the Aboriginal people as well as understanding of the logistical complexities.12 The overall implications of suboptimal discharge processes impact on patients and health workers. Negative impacts can include but are not limited to, more staff time spent making patient arrangements, delayed discharge for the patient, inconsistent and poorly coordinated transport schedules leading to long delays, reduced provision of care in the community, additional and often unnecessary trips and hospital admissions that could be avoided.13,14
To address some of these problems, a web based Aboriginal health linking information tool in the form of a database was developed with the aim of improving the patient discharge process and the post-discharge patient journey for Aboriginal patients from Perth hospitals back to their remote homes. It will initially be trialed in the remote Western Australian regions of Pilbara and Kimberley. Dependent on an outcome evaluation and understanding of the unintended consequences, it has the potential to be rolled out across Australia.

Figure 1. Geographical representation of the Pilbara and Kimberly regions of Western Australia and the distance from Perth. 15
Program Summary
The current discharge processes for Aboriginal patients returning to remote areas in the North of Western Australia, specifically the Pilbara and Kimberley regions, are impacted by a lack of readily accessible local information to metropolitan-based health workers. Without an understanding of the resources, geography, services and other factors relevant to post-discharge support and management, metropolitan-based health workers are not able to make effective and efficient discharge plans which may result in either poor care and follow up, or patients having to staying in Perth longer than necessary, away from their families and at additional costs.
Figure 2 shows a schematic representation of the current situation which utilisation of the database aims to improve. A secondary outcome of the evaluation may identify areas of improvement that can enhance the success of the program. If this evaluation demonstrates that the program is successful, the scope of the program could be expanded to include other regional and remote locations across Australia.
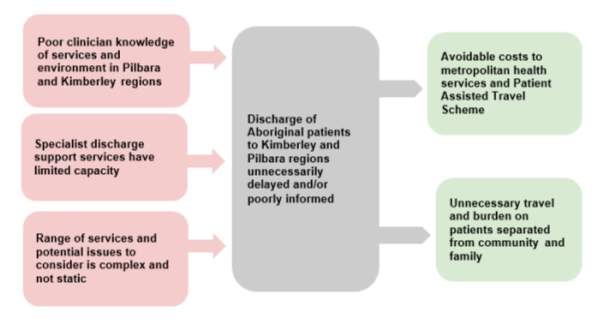
Figure 2. Schematic representation of the problem to be addressed in this evaluation
The following case example highlights the need for better information at the time of discharge and demonstrates the impacts on the patients and their families.
Case Example
Joe* is a 47-year-old Aboriginal male who resides in Swift Bay, 120 kilometers west of the Kalumburu Aboriginal Community in the Kimberley area of Western Australia. He underwent vascular surgery at the Fiona Stanley hospital in Perth and was ready for discharge. His surgeon requested a follow review in 2 weeks and suggested he should remain in Perth until his follow up appointment time. Joe and his wife were staying in a Perth hotel near the hospital, when they received word that one of their relatives had passed away. Aboriginal people place great importance on the cultural practice of ‘sorry business’, where a whole community comes together to share the sorrow.16 Joe and his wife left Perth the day before the review appointment. Another follow up appointment was made in 3 weeks’ time, requiring Joe and his wife to make the 24-hour journey back to Perth and accommodation was required for 4 days pending return travel arrangements. They could have had follow up with a visiting cardiologist from Perth via telehealth conferencing at their local hospital, which would have been a 4-hour same day return trip using local transport.
* name changed for privacy reasons
The Evaluand
The evaluand is a database portal that is accessible to metropolitan-based health workers 24/7 containing information regarding the availability of funded medical and support services within the Pilbara and Kimberley regions. It will provide information on location and operating hours of community pharmacies, local hospitals with telehealth facilities, visiting specialists schedules, nursing availability and skills, along with relevant and practical information such as seasonal weather, road conditions during seasons, travel times and distances between communities and services. The inclusion of aspects of cultural aspects is collaborative and aims to include information on sacred sites, significant exclusion times and areas where applicable and available. It is understood from conversations with Aboriginal Health Liaison Officers (AHLO) that some information may not be included due to cultural sensitivity, thus this could be considered a limitation of the database information.
Training of hospital clinicians and AHLO staff would be undertaken so that discharge planning is synergistic and utilises the intimate local area knowledge of the AHLO’s to maximise efficiencies and patient experience. Access to this database at the point of discharge planning aims to facilitate more informed and streamlined plans which can support discharge decisions to return patients to remote areas or to accommodate them in Perth until they are well enough to return to their home.
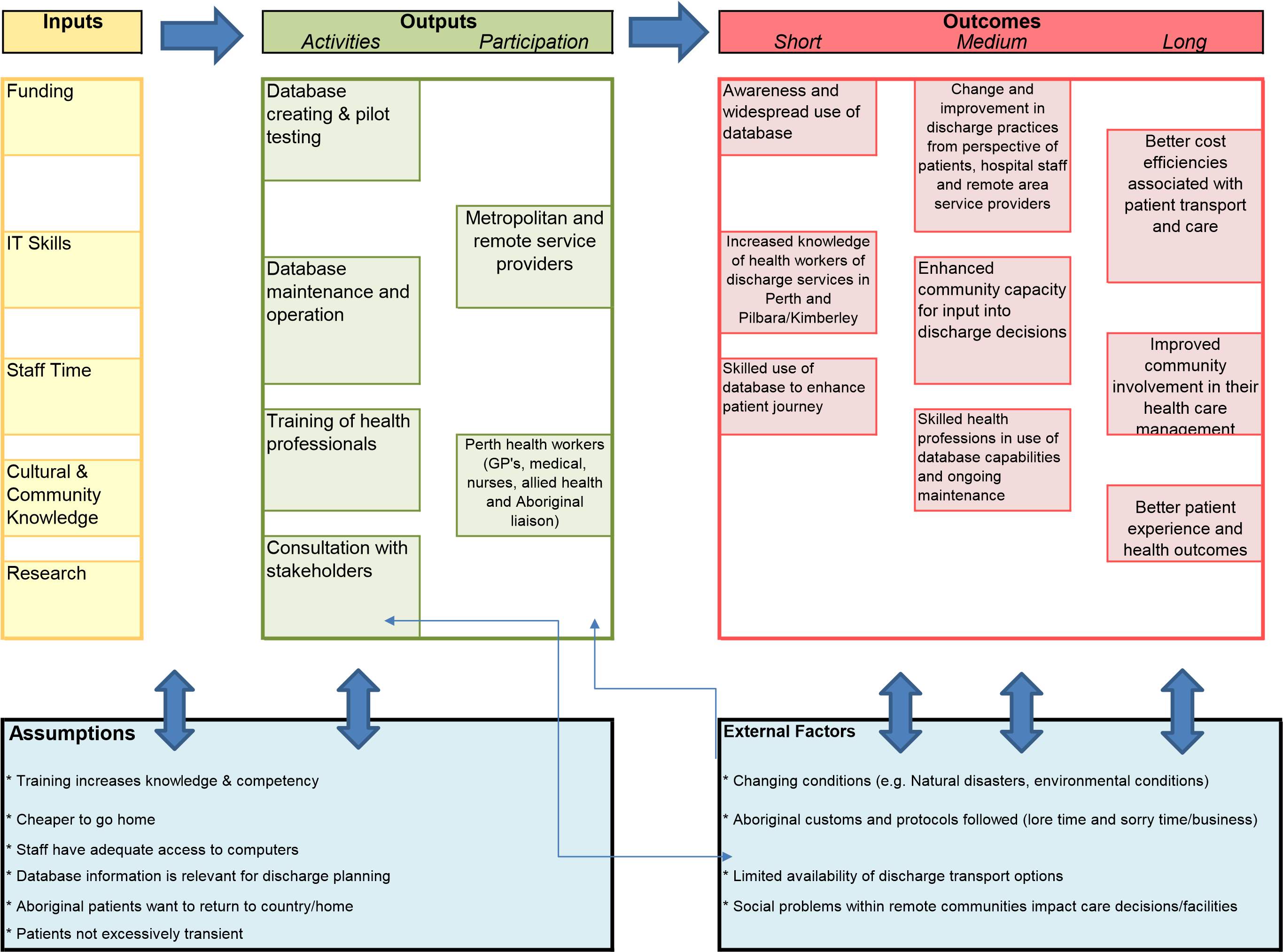
Program Logic
The program logic model below demonstrates the logical linkages among the program resources, the outputs (activities and audience) and short, medium and long-term outcomes17, in consultation with the stakeholders about the strategies and chain of events that need to occur to accomplish the goals and objectives of the database implementation. During the evaluation process, it will be used as guide to define what is done and how success of the outcomes will be measured in addition to providing an opportunity to identify areas of improvement.
It is read from left to right and starts with the inputs defined as the resources needed for the project. It then moves to outputs which show the activities, processes, tools and events to bring about the intended changes and results of the database usage. The participation column shows the people who will use the database and participate in the activities. The outputs are the product of the program activities. Outcomes are the expected changes that result from the program’s activities and range from short to long term results. Short term outcomes are the most immediate changes, evidenced in learning and knowledge of the database use and practicalities. Medium term outcomes are the changes in the behaviours and practices because of the increased knowledge and awareness of the database and used in the discharge planning process. Long term outcomes are the conditions that change as a result of the actions of the users and in this case effect the end user. 18,19
Purpose of the Evaluation
It is the intention of this evaluation to determine whether the database program meets the aim of improving hospital discharge for Aboriginal patients returning to the Pilbara and Kimberley after receiving treatment in Perth metropolitan hospitals. An improvement would be identified as a reduction in treatment and transport and better patient experiences. The outcome evaluation will be a mixed method design, using qualitative and quantitative data as the most appropriate methods given the timeframes and budget constraints.
A secondary outcome of the evaluation may identify areas of improvement that can enhance the success of the program. The significance of the evaluation is instrumental in that if the program demonstrates tangible improvements to the patient experience, streamlines the services and consequently delivers cost efficiencies, then the scope of the program could be expanded to include other regional and remote locations within Australia with further interstate transferability.
Intended Audience and Stakeholders
This mixed methods outcome evaluation is commissioned by the Government of Western Australia Health Department who will be the recipient of the full evaluation report. Other stakeholders and their interests are:
- Aboriginal Health Council of Western Australia – a peak body that represents 21 Aboriginal Community Controlled Health Services across Western Australia.
- St John Ambulance Australia – provider of high quality ambulance and first aid services.
- Lions Eye Institute – non-for-profit organisation using scientific research and clinical practice in the prevention of blindness and eye diseases
- Australian Medical Association – The Australian Medical Association is the professional association for Australian doctors and medical students.
- Royal Flying Doctor Service – extensive primary health care and 24-hour emergency service to those who live, work and travel throughout Australia.
- Primary Health Works (Country WA) – support organisation for primary health providers – GPs, allied health professionals and community services to provide efficient and effective medical services to patients, particularly those at risk of poor health outcomes.
- Aboriginal Medical Service – health service for Aboriginal people in Perth metropolitan area.
- Aboriginal Health Liaison Workers – provide support services including travel, transport and interpreters to assist Aboriginal patients through the care and discharge process in a culturally informed and respectful manner.
- Aboriginal Health Workers – Play a vital role in the primary health care workforce, providing clinical and primary care for individuals, families and community groups.
- Western Australian Country Health Service – provides accessible health services to the regional population and a quality health care workforce.
Key Evaluation Questions
- Have discharges of Aboriginal patients returning to remote locations (Kimberley and Pilbara) improved following the commencement of the database system?
- Have there been any unintended consequences of the program?
- To what extent have discharge planning processes changed?
- What is the patient experience?
Outcome Evaluation Design, Methodology and Analysis
Table 1 below represents the design and methodology of the outcome evaluation. It details what and how the outcomes are being evaluated and the types and process of gathering information data for analysis.
This type of study is descriptive with a mixed method design to assess the service utilisation of the database and to gather the views of both direct user and recipient of the services the database was designed to assist in the patient discharge process for Aboriginal people living in the Pilbara and Kimberly regions of Western Australia.
The methodology used will be both quantitative and qualitative by way of self-report surveys, quizzes with users and focus groups with groups involved in the discharge process and by yarning with Aboriginal patients. Due to time and budget restraints, each group will be a representative sample of the wider group of users and recipients.
Purposive sampling will be done in that with some key outcomes, certain people will be selected representative of the wider users and selected patients who have experienced the discharge process using the database to arrange their post health care will be interviewed.
Quantitative measures will be the analysis of key database usage statistics broken down into type of health person, number of use, length of time of use and other key broad metrics. These will be statically analysed using t-tests and correlations comparing information gathered at baseline (assumption of no knowledge), one month after database introduction and use and again at 3 months after inception and use. Quantitative data results will be presented as tables, graphs or charts.
Qualitative data will be presented as descriptive themes in the final report of the outcomes evaluation and presented to key stakeholders.
Table 1: Outcome Evaluation Design: Mixed Methods (Quantitative and Qualitative)
|
OutcomeFactor |
Measure&Analysis |
Indicator |
Method |
Sampling |
MethodType |
|
Awareness and widespread use of database |
Survey issued to all intended users asking about awareness and use of database | % of users surveyed self-reporting use and awareness of database |
On-line survey sent to all known users |
Purposive sampling: All users who have access to the database |
Quantitative |
|
Increased knowledge of health workers of discharge services in Perth and Pilbara/Kimberley |
Knowledge and competency quiz scores taken pre-training and post 3 months |
% of health professions who increased knowledge after database training and use in a discharge plan |
On-line self-quiz development with ProJet team and delivered immediately before staff training. Staff repeat quiz after 3 months | Purposive sampling: All staff undertaking training who used the system at least once in relation to patient discharge |
Quantitative |
|
Skilled use of database to enhance patient journey as experienced by the Aboriginal patients Links into Better patient experience and health outcomes |
Qualitative themes and issues raised |
Both positive and negative experiences shared |
Yarning on patient experiences by community based health workers. Template recording after the yarning to record key issues discussed |
Purposive sampling: First 2 adult patients being discharged to target communities in each region during the evaluation period |
Qualitative |
| Summary of issues by themes and assessment of ‘positive’, ‘negative’ and ‘neutral’ comments | |||||
|
Change & Improvement in discharge practices experienced by patients, hospital staff and remote area service providers |
Qualitative feedback on discharge following implementation of database. |
Feedback on use of database utility in the discharge process |
Focus Groups |
3 x Focus groups help across 2 locations. Groups will be by discipline. Convenience sampling by invitation |
Qualitative |
|
Number of staff logging in and accessing information |
Increase in number of staff logging in to system and increase in time spent in database to a statistically significant degree comparing 1st month use with 3rd month use |
Data report generated for database system, broken down to hospital, designation, dates, times and sections accessed |
Purposive sampling: Data available from all users |
Quantitative |
|
| Enhanced community capacity for input into discharge decisions Linking into
Improved community involvement in their own health care management |
Qualitative themes and issues raised |
Both positive and negative experiences shared about how they felt included into the discharge process and if they feel they have their health better managed |
Yarning on patient experiences by Aboriginal patients living in remote Pilbara/Kimberley region. Template recording after the yarning to record key issues discussed |
Purposive sampling: First 2 adult patients being discharged to target communities in each region each fortnight during the evaluation period |
Qualitative |
| Summary of issues by themes and assessment of ‘positive’, ‘negative’ and ‘neutral’ comments | |||||
|
Skilled health professions in use of database capabilities and ongoing maintenance |
Number of staff logging in and accessing information |
% of users within each group |
Data report generated for database system, broken down to hospital, designation, dates, times and sections accessed |
Purposive sampling: Data available from all users |
Quantitative |
| Number of request for updating information within the database and number of medical specialist’s remote visiting schedules added to database |
% of changes and added specialist schedules comparing start of database and at 3 months |
Quantitative |
|||
|
Better cost efficiencies associated with patient transport and care |
$ per patient per activity episode linked from data |
% decrease in costs between matched and evaluation periods |
Unobtrusive data collection: ABF, Medicare, PBS and Patient Assisted Travel Scheme data accessed |
Purposive sampling: All adult patients admitted for at least 1 day to RPH or FSH between a specified date range and discharged home to remote location between certain specified dates with discharge involving AHLO’s |
Quantitative |
|
Average of cost per patient pre-and post-period – t -test |
Quantitative |
||||
Limitations
It is important to consider some limitations to the outcome evaluation, particularly of a cultural nature that may impact on outcomes. Whilst many are included in the external factors and assumptions of the program logic model, there are some others worth noting. Currently the health system has a ‘miss an appointment and you lose your place’ which is not conducive or flexible in meeting the needs of the Aboriginal people, where adhering to traditional customs are considered a priority to the individual. This can lead to many missed appointments, poorer health care management and outcomes for the individual and disengagement with medical/health services.12 In addition, transport scheduling and availability can impact on discharge decisions. Another factor worth noting is that there can be within cultural ostracisation/disapproval towards those chosen to receive treatment and those not.
There are also database limitations in that the timely and ongoing maintenance of the database can be compromised by missing or late information. It is only as accurate as the information provided and may not contain some culturally sensitive information, omitted purposefully for confidentiality. This is where the relationship and inclusion of the community members and AHLO is invaluable as they have intimate knowledge about the community, traditions and circumstances that can impact on best treatment outcomes and discharge planning and decisions. They are also likely to understand which patients are more likely to receive medical treatment and follow medical advice and future appointments, and the reasons associated with these behaviours.
This outcome evaluation will not factor in all individual circumstances when evaluating the outcomes, however they need to be considered synergistically with the results found. Key recommendations will be provided; however, these will also need to be viewed synergistically with the community and the medical profession.
Ethical Issues
This outcome evaluation is undertaken with respect to the principles and values of the Aboriginal people in accordance with the guidelines set out in the National Health and Medical Research Council of Australia20 and with the view that this research will do no harm and benefit the patient care and experience of the Aboriginal people within the Pilbara and Kimberley regions of Western Australia. The six core values set out in the guideline and how they will be considered within this outcome evaluation are addressed below.
- Spirit and Integrity – the understanding that the present and the future are bound up in the past and are not separate from each other. The liaising with AHLO’s will assist us this aspect and ensure we are always mindful of this in our interpretations.
- Reciprocity – inclusion and recognition of the contributions from the Aboriginal people to their yarning and focus group participation. The outcome evaluation may provide benefit by way of better patient care and patient journeys with respect to their families and time away from home, which are consistent with what the Aboriginal people and AHLO’s voiced in previous consultations.
- Respect – acknowledging the induvial and collective contribution of the Aboriginal people and seeking agreement at the outset of this evaluation as to when, how and who will be engaged in the research process to ensure transparencies and all parties are equally respectful. The effects of difference blindness will be minimized through a consultative process with identified key Aboriginal members and AHLO’s to acknowledge and affirm the different values, norms and aspirations, so that the purpose, methods, demands, risks, inconveniences, discomforts and possible outcomes of the research are understood and agreed to by all stakeholders involved. In addition, all relevant issues such as management of data, publication arrangements, protection of individual and community identity and their right to either voluntarily participate, refuse or withdraw, will be addressed and at their level of comprehension.
- Equality – the collective memory and shared experience of the Aboriginal people in the telling of their personal patient journeys is highly valued and appreciated. All communities involved will be included and consulted on the proposed research so that understanding of the research, it’s benefits and the distribution of the evaluation outcomes is transparent and equitable to the satisfaction of the Aboriginal people. No one stakeholder will have advantage over another.
- Survival and Protection – this outcome evaluation aims to contribute to the social and cultural bonds by assessing the utility of the database to enhance patient experience with medical interactions and appointments. Any concerns expressed which may be contrary to this will be rectified to ensure culture is not compromised. Confidentiality is ensured with our handling and storing of data under the University of Western Australia policy and guidelines.
- Responsibility – This evaluation is conducted mindful of doing no harm to individuals, communities or the things the Aboriginal people value and to establish processes which ensure our accountability to Aboriginal people and their social and cultural dimensions.
Further to adherence to the guidelines, we will engage with an Aboriginal reference group and ask for two letters of recommendation and make submissions to four ethics committees listed below:
- WA Human Research Ethics Committee (DoH HREC)
- WA Aboriginal Human Ethics Committee (WAAHEC)
- UWA Human Research Ethics Committee (HREC)
- Kimberley Aboriginal Health Planning Forum (KAHPF)
The collection of evaluation data handling and storage will involve the de-identifying of participants data and stories and all records will be stored indefinitely due to there being patient records created within the Pilbara and Kimberley regions. Questionnaire data and participant responses will be securely coded, and stored separately from identifying information on the protected University of Western Australia Institutional Research Data Store (IRDS). Participants will be assigned non-identifying codes and no names will be disclosed to any third parties unless legally required to do so. Any hard copy identifiable data will be maintained in a ‘restricted-access’ lockable cabinet, in a lockable office when not in direct use. Only the research personnel identified in the approved ethics application or who have signed confidentiality agreements related to the project will be permitted access to the data. On completion of the project, all electronic and hard copy records will be retained indefinitely after date of publication or project completion, whichever is the latter, archived (in an encrypted/password protected file or archive box marked confidential) and forwarded to the School of Population Health Manager at the University of Western Australia. Any research results published will not have any participant’s identifying information included as per the University of Western Australia guidelines.21
Timeline
Table 2 contains a project and evaluation timeline which highlights the different evaluation activities and deadlines. It has been negotiated with key stakeholder groups to ensure outcomes are agreed upon, are relevant to the project and deliverable. After initial creation of database there will be pilot testing to address any potential ‘bugs’ followed by a live launch scheduled for Feb 2017. Baseline testing of knowledge with key users will commence one month prior to live launch. This will be followed by two more knowledge assessments conducting one month after live launch and again at conclusion of three months of use to determine if there are any measurable improvements in knowledge, skills and attitudes of users. Focus groups with key medical personnel users and yarning with Aboriginal patients will also commence after three months of use. Final reports and summaries will be presented to all key stakeholders by the deadline in April with a visual presentation at the WADoH conference in May 2018.
Budget
The budget in Table 3 is indicative of the associated costs of implementing, conducting analysis and presenting the outcome evaluation within the stated timeframe. The actual planning and implementing of the database are beyond the scope of works of this outcome evaluation and are completed by a non-affiliated, information technology specialist third party.
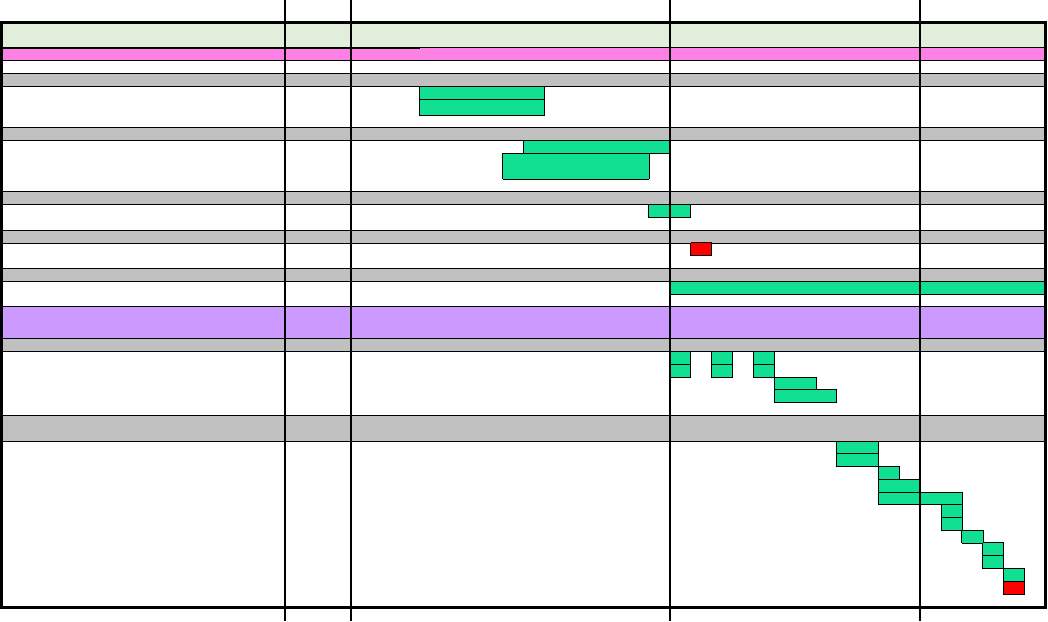
Table 3. Outcome Evaluation Budget
Dissemination of Outcome Evaluation
Two outcome evaluation reports will be generated. First will be an in-depth report on all findings and key recommendations, presented to the key audience, The Western Australian Department of Health (WADoH). The second will be a summary report and summary poster presented to each of the stakeholders and each of the Pilbara and Kimberley Aboriginal communities who contributed to the project.
A visual presentation and summary poster of the outcome evaluation findings will be presented by the leading evaluator and assistant evaluator at the WADoH conference in Broome in May 2018.
References
1. Statistics ABo. In: Life Tables for Aboriginal and Torres Strait Islander Australians, 2010-2012. 2013. Canberra: Australian Burea of Statistics.
2. Vos T, Barker B, Stanley L, Lopez AD. The burden of disease and injury in Aboriginal and Torres Strait Islander peoples 2003. Brisbane; 2007.
3. A B. Acute coronary syndromes in indigenous Australians: opportunities for improving outcomes across the continuum of care. Heart Lung Circ. 2010;19(5-6):325-336.
4. Statistics. ABo. The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. 2010 [cited 2017 19 July]. Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/lookup/4704.0Chapter210Oct+2010
5. Services WCH. Pilbara Regional Profile. The Government of Western Australia; 2015 [cited 2017 20 July]. Available from: http://www.wacountry.health.wa.gov.au/index.php?id=494
6. Serafina S, Anderson C, Waenerberg N. In: Pilbara Health Profile. 2015 WA Department of Health.
7. WA Country Health Services. Kimberley Regional Profile. The Government of Western Australia; 2015 [cited 2017 20 July]. Available from: http://www.wacountry.health.wa.gov.au/index.php?id=492
8. Serafina S, Anderson C. In: The Kimberley Health Profile. 2015. Perth: The Department of Health, WA Country Health Services.
9. Katzenellenbogen J, Teng T, Lopez D, Hung J, Knuiman M, Sanfilippo F, et al. Initial hospitalisation for atrial fibrillation in Aboriginal and non-Aboriginal populations in Western Australia. Heart Advis. 2015 [cited 11 July, 2017];101(9).
10. Teng H, Katzenellenbogen J, Thompson S, Sanfilippo F, Knuiman M, Geelhoed E, et al. Incidence of first heart failure hospitalisation and mortality in Aboriginal and non-Aboriginal patients in Western Australia, 2000–2009. International Journal of Cardiology,. 2014 [cited 11 July 2017, ];173(1).
11. Hall S, Bulsara C, Bulsara M, Hendrie D, Holman C, Leahy T, et al. Treatment patterns for cancer in Western Australia: Does being indigenous make a difference? Medical Journal of Australia. 2004 [cited 10 July, 2017];181(4):191-194.
12. Katzenellenbogen J. Round 9 [Application Form]. In: State Health Research Advisory Council Research Translation Projects. 2015. Perth: State Health Research Advisory Council.
13. Malyon R, Zhao Y, Oates B. Differences in the cost of admitted patient care for Indigenous people and people from remote locations. Aust Health Rev. 2012 [cited 10 July, 2017];37(1):26-31.
14. Dwyer J, Kelly J, Willis E, Glover J, Mackean T, Pekarsky B, et al. In: Managing two worlds together : City hospital care for country Aboriginal people. 2011. Bedford Park, South Australia: Lowitja Institute.
15. Horton DR. Aboriginal Australia Wall Map of Western Australia [Map]. Canberra: Aboriginal Press Studies; 1996 [15 July, 2017]. Australian Institute of Aboriginal and Torres Strait Islander Studies. Available from: https://aiatsis.gov.au/
16. Korff J. Mourning an Aboriginal Death. 2017 [cited 2017 24 August]. Available from: https://www.creativespirits.info/aboriginalculture/people/mourning-an-aboriginal-death#axzz4niw0taFZ
17. Julian DA. The utilization of the logic model as a system level planning and evaluation device. Eval Program Plann. 1997 [cited 14 July 2017];20(3):251-257.
18. Hannum K. Handbook of Leadership Development Evaluation. 1st ed. ed. Hoboken: Wiley; 2006.
19. Boulet S, Mai C, O’Leary LA, Silverman B. Logic models for planning and evaluation; a resource guide for the CDC State Birth Defects Surveillance Program cooperative agreement. 2007.
20. National Health and Medical Research Council. In: Value and Ethics: Guidelines for Ethical Conduct in Aboriginal and Torres Strait Islander Research. 2017. Canberra:
21. Policies and procedures : Governance : The University of Western Australia [Policy Guideline Document]. Perth: The University of Western Australia; 2012 [updated 2016; cited 2017 31 July,]. Available from: http://www.governance.uwa.edu.au/procedures/policies/policies-and-procedures?method=document&id=UP12/25
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Information Systems"
Information Systems relates to systems that allow people and businesses to handle and use data in a multitude of ways. Information Systems can assist you in processing and filtering data, and can be used in many different environments.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




