Anaphylactic Reaction to Penicillin: Physiological Responses, Causes and Treatment
Info: 3704 words (15 pages) Dissertation
Published: 11th Dec 2019
Tagged: Medicine
A patient is attending you for surgery. The patient is given a dose of penicillin and develops an anaphylactic reaction. Explain using the normal physiological principles the aetio – pathological reasons for the clinical signs and symptoms and how treatment should be affected.
(breathing difficulties, tachycardia, hypotension, confusion, urticaria, vasodilatation, peripheral warmers, bowel symptoms)
Anaphylaxis is defined as ‘a serious, generalised or systemic, allergic or hypersensitivity reaction that can be life-threatening or fatal’. This definition was proposed recently by the International Consensus on Anaphylaxis and is intentionally generic in order to encompass both immunologic and non-immunologic anaphylaxis.(1)
Shock is the clinical expression of an abnormality of the circulatory system that results in inadequate organ perfusion, tissue oxygenation and/or cellular oxygen utilization.(2)
Four types of shock are recognised(3):
- Distributive shock
- Cardiogenic shock
- Hypovolaemic shock
- Obstructive shock
Patients may experience more than one type of shock simultaneously.
Anaphylactic shock is considered a form of distributive shock, characterised by decreased peripheral vascular resistance and hypotension. However, anaphylactic shock also shares features of hypovolaemic shock due to loss of intravascular fluid, and cardiogenic shock from reduced venous return and myocardial depression.(4)
‘Anaphylactoid reaction’ is a term that was previously used to describe a non-immunologic (i.e. IgE-independent) event which was clinically indistinguishable from a classic, immunologic (i.e. IgE-dependent) anaphylactic reaction. However, the World Allergy Organisation discourages the use of this term and encourages the use of ‘anaphylaxis’ as an umbrella term for all anaphylactic reactions, regardless of whether the underlying aetiology is immunologic or non-immunologic.(5)
Cardiovascular Physiology and the Physiology of Shock
The major physiologic determinants of tissue perfusion and systemic blood pressure (BP) are cardiac output (CO) and total peripheral resistance (TPR), given by the formula:
BP = CO x TPR
Cardiac output (CO), in turn, is a product of heart rate (HR) and stroke volume (SV), given by the formula:
CO = HR x SV
SV = End Diastolic Volume – End Systolic Volume
Total peripheral resistance (TPR) is determined by vessel length, blood viscosity, and vessel diameter.
Biologic or pathologic processes that alter any one of these parameters can result in hypotension and shock. These formulae make it easy to explain all types of shock and the effects it has on the body.(6)
Hypovolaemic shock, cardiogenic shock, and obstructive shock are characterised by a low CO with compensatory increase in TPR, in order to maintain perfusion to vital organs. This is because they all result in a fall in SV, with a consequent fall in CO and compensatory increase in HR (because CO = HR x SV).
On the other hand, distributive shock (anaphylactic shock) is associated with reduced TPR (due to severe peripheral vasodilatation) and a compensatory increase in CO.
In both scenarios, the formula BP = CO x TPR dictates that hypotension ensues if either CO or TPR are reduced.
Anaphylaxis results in;
- Vasodilation
- Reduced SV
- Reduced TPR
- Reduced BP
- Increased HR
As a result of reduced tissue perfusion, the body reacts with compensatory responses. The main mechanisms involved in this compensatory response are:
- the sympathetic nervous system
- the renin-angiotensin-aldosterone system
Baroreceptors throughout the vascular system detect changes in blood pressure.(6) A reduction in pressure (like in hypotension), activates the baroreceptor reflex and stimulates the sympathetic nervous system. Activation of the sympathetic nervous system results in tachycardia, bronchial smooth muscle relaxation and bronchodilation, and peripheral vasoconstriction, as well as sympathetic activation of the renin-angiotensin-aldosterone system (RAAS).
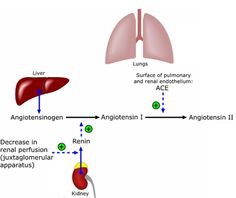
Figure 1. Renin-angiotensin-aldosterone system. (7)
When the kidney detects decreased renal perfusion, it releases the enzyme renin. Renin cleaves angiotensinogen to release angiotensin I; angiotensin I is then converted to angiotensin II by angiotensin-converting enzyme (ACE) in the pulmonary vasculature. Angiotensin II is a potent vasoconstrictor, acting to increase blood pressure and intravascular volume. Angiotensin II also stimulates activation of the sympathetic nervous system.
Shock and end-organ dysfunction occur when these normal physiological mechanisms are overwhelmed.
Reduced tissue perfusion and oxygenation causes hypoxia. Hypoxia can have many consequences, including intracellular oedema, leakage of intracellular contents into the extracellular space, myocardial depression, and further stimulation of inflammatory cascades. These abnormalities manifest as the signs and symptoms of end-organ dysfunction, including tachycardia, breathing difficulties (dyspnoea), increased sweating (diaphoresis), hypotension, restlessness, reduced mental proficiency and abdominal pain. These can all be seen in anaphylaxis.(8, 9)
Pathophysiology of Anaphylaxis
Anaphylaxis may be immunologic (i.e. IgE-dependent) or non-immunologic (i.e. IgE-independent).(9)
IgE-dependent anaphylaxis is the predominant cause of anaphylaxis. In people with an allergic tendency, there is an increase in the amount of circulating IgE antibodies, called reagins. IgE antibodies have a strong tendency to bind to mast cells and basophils. When an allergen then enters the body, it reacts with these basophils and mast cells which have been sensitised by IgE reagins, and an allergen-reagin reaction occurs. This results in activation of intracellular signalling cascades and the release of preformed mediators from mast cells and basophils. (9)
It is these mediators, like histamine and tryptase, and the production of inflammatory mediators, which are responsible for causing the signs and symptoms we see in an anaphylactic reaction. (10)
IgE-independent anaphylaxis results from activation of mast cells and basophils without evidence of involvement of IgE. (11)
The major biochemical mediators of anaphylaxis are:
- histamine
- tryptase
- nitric oxide
- platelet-activating factor
- arachidonic metabolites
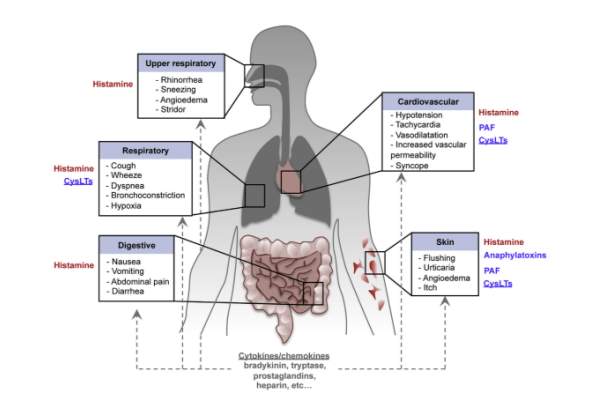
Figure 2. Pathophysiological changes in anaphylaxis and mediators that have been implicated in these processes. (10)
Cardiovascular Pathophysiology in Anaphylaxis
The major cardiovascular sequelae of anaphylaxis include:
- hypovolaemia
- hypotension
- cardiac arrhythmia
- myocardial depression
Hypovolaemia and Hypotension
The release of histamine results in many of the cardiovascular complications seen in anaphylaxis. The effects of histamine are mediated via activation of H1 and H2 receptors.(12)
Histamine acts on H1 receptors to increase vascular permeability. This increased permeability results in big fluid shifts. During anaphylaxis, it is possible for up to 35% of intravascular fluid volume to shift to the extracellular space in the first 10 minutes of an attack.(13) The binding of histamine to H1 receptors also results in production of nitric oxide, a potent vasodilator. The combination of peripheral vasodilatation and loss of fluid account for the sudden and profound hypotension seen in anaphylaxis, constituting a mixed hypovolaemic-distributive shock as previously discussed.
Activation of the sympathetic nervous system (such as activation of the RAAS) initially tries to counter the peripheral vasodilatation and fluid loss of anaphylaxis, promoting peripheral vasoconstriction and fluid retention. These compensatory mechanisms can be overwhelmed in some people, resulting in hypotension and shock.
Clinically, peripheral vasodilatation and fluid loss manifests as hypotension (systolic blood pressure < 90 mmHg), and tachycardia (heart rate >100 bpm). Hypotension and shock can cause a reduction in organ perfusion, resulting in confusion, anxiety or agitation (due to cerebral hypoperfusion), decreased urine output (due to renal hypoperfusion), and warm peripheries (reflecting peripheral vasodilatation).
Cardiac Arrhythmia and Myocardial Depression
In the heart, histamine activation of H1 receptors results in coronary artery vasoconstriction. This can result in myocardial ischaemia and arrhythmias. Tachycardia is the most common arrhythmia seen in anaphylaxis. Once intravascular fluid volume starts to fall, baroreceptors detect decreased vascular pressure and activate the sympathetic nervous system to increase heart rate and myocardial contractility, and thus cardiac output (CO = HR x SV). (6)
Activation of H2 receptors results in coronary artery vasodilation, increased atrial and ventricular contractility, and positive chronotropy (increased heart rate).(12)
Myocardial depression is also a feature of anaphylaxis.(14) This is likely due to the direct mediator effect on the myocardium.
As a result of myocardial ischaemia, clinically patients may complain of chest pain. A 12-lead electrocardiogram may show changes consistent with coronary artery vasospasm, ischaemia or infarction, or evidence of cardiac arrhythmia (e.g. Tachycardia).
Respiratory Pathophysiology in Anaphylaxis
The major upper respiratory tract sequelae of anaphylaxis include:
- rhinorrhoea
- oropharyngeal oedema
- laryngeal oedema
The major lower respiratory tract sequelae of anaphylaxis include:
- bronchial smooth muscle constriction
- bronchospasm
Oropharyngeal oedema and laryngeal oedema result from peripheral vasodilatation, increased vascular permeability and loss of fluid. Stridor is a high-pitched inspiratory sound that results from turbulent airflow through a partially obstructed upper airway, due to laryngeal oedema. This is different to Stertor, which is a snoring sound on inspiration, caused by partially obstructed airflow in the oropharynx. (15) Oropharyngeal and laryngeal oedema can lead to total occlusion of the upper respiratory tract, respiratory arrest and death.
Bronchial smooth muscle constriction results from the release of inflammatory mediators, with activation of H1 receptors. Once arachidonic acid is metabolised from cells like mast cells and basophils, it leads to the production of proinflammatory mediators including leukotrienes, prostaglandins, and platelet-activating factor. (9, 16) Previously known as slow-reacting substance of anaphylaxis, these mediators can cause spasm of the smooth muscle of bronchioles.(9) Leukotrienes D4 and E4, and prostaglandin E2, are potent bronchoconstrictors and increase vascular permeability.(17)
Activation of H1 and H2 receptors stimulate increased mucous secretion, which can result in airflow obstruction, respiratory arrest, and death.
Clinically, bronchial smooth muscle constriction and increased mucous secretion combine to result in difficulty breathing (dyspnoea), cough, wheeze (an expiratory air sound that results from airflow obstruction), hypoxaemia and respiratory failure, respiratory arrest and death.(18)
Cutaneous Pathophysiology in Anaphylaxis
During anaphylaxis, the allergen can travel to areas of the skin and cause localised reactions. Histamine and other proinflammatory mediators are released from mast cells and basophils, resulting in local vasodilation and increased capillary permeability, resulting in urticaria.(9)
The local vasodilation causes a red rash and flushing, and the increased capillary permeability causes local skin swellings called hives.
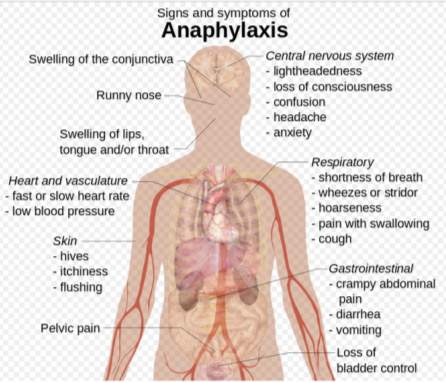
Figure 3. Summary of signs and symptoms of anaphylaxis. (19)
Correlating Pathophysiology with Treatment Options
Given the life-threatening nature of anaphylaxis, all international guidelines agree that rapid recognition of the condition and immediate intervention are critical. Immediate intervention should include a call for help to emergency services.
Intramuscular adrenaline (to the mid upper thigh) is the universally accepted first-line treatment for anaphylaxis. Based on an understanding of the underlying pathophysiology of anaphylaxis, the rationale for its use is clear.
Adrenaline acts on α1-adrenergic receptors to induce vasoconstriction, which can prevent or reduce hypotension and distributive shock, as well as tissue and airway oedema; β1-adrenergic receptors to exert a positive chronotropic (increasing heart rate) and inotropic (increasing cardiac contractility) effect; β2-adrenergic receptors to dilate the airways, potentially inhibit the release of mediators from mast cells and basophils, and relieve urticaria.(18, 20) Early intramuscular adrenaline injection has clearly been proven to significantly reduce anaphylaxis related fatalities.
Second line therapies include lying the patient supine with legs elevated (to promote venous return), giving intravenous fluid resuscitation (to combat hypovolaemia and distributive shock), and oxygen therapy.
Antihistamines and corticosteroids might play a role in reducing respiratory signs and symptoms and delayed anaphylactic reactions, respectively, but do not replace adrenaline as first line therapy.(20)
The patient’s vital signs should be monitored at regular intervals, and if necessary, cardiopulmonary resuscitation should be initiated and continued until the arrival of emergency services.
Anaphylaxis and Sedation/Anaesthesia
The occurrence of anaphylaxis during anaesthesia has been reported in the literature, with an incidence ranging from 1 in 4,000 to 1 in 20,000.(21) During conscious sedation or general anaesthesia, anaphylaxis can present as cardiovascular collapse, respiratory arrest, or skin manifestations. Cutaneous manifestations of anaphylaxis can be difficult to diagnose given the nature of these procedures, as the patient will unlikely be able to verbalise their complaint.
During procedures where the patient is sedated or under general anaesthesia, they can be exposed to multiple allergens which may trigger anaphylaxis. The most common of these include latex and antibiotics, which are commonly used in the dental setting.
There have been reports of anaphylactic reactions to benzodiazepines, although these seem very rare. These reports are largely limited to case reports, and most cases involved multidrug use for general anaesthesia, where it was impossible to identify the causative agent. There does seem to be a consensus that Diazepam is more likely to cause an allergic reaction than Midazolam due to the lack of any active metabolites in Midazolam.(21, 22)
Chlorhexidine is another agent commonly used in the dental setting, and is being reported as an increasingly common allergen that can trigger anaphylaxis. (23)
The management of anaphylaxis that occurs during a procedure involving conscious sedation or general anaesthesia is like that described above. This involves stopping the procedure and discontinuing the administration of any potential allergen, calling for help, maintaining the airway, and administration of intramuscular adrenaline.
References
1. Simons FER, Ardusso LR, Bilò MB, Cardona V, Ebisawa M, El-Gamal YM, et al. International consensus on (ICON) anaphylaxis. World Allergy Organization Journal. 2014;7(1):9.
2. Vincent J-L, De Backer D. Circulatory Shock. New England Journal of Medicine. 2013;369(18):1726-34.
3. Weil MH, Shubin H. Proposed reclassification of shock states with special reference to distributive defects. The Fundamental Mechanisms of Shock: Springer; 1972. p. 13-23.
4. Brown SGA. The Pathophysiology of Shock in Anaphylaxis. Immunology and Allergy Clinics of North America. 2007;27:165-75.
5. Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. Journal of Allergy and Clinical Immunology.113(5):832-6.
6. Stassen L. Cardiovascular Anatomy, Physiology and BP Control. Lecture for Diploma in Conscious Sedation in Dentistry2017.
7. Contributor WC. Renin-Angiotensin-Aldosterone System: Wikimedia Commons, the free media repository; 2015 [Available from: https://commons.wikimedia.org/w/index.php?title=File:Renin-angiotensin-aldosterone_system.png&oldid=169864402.
8. Cafaro RP. Hypoxia: Its Causes and Symptoms. Journal of the American Dental Society of Anesthesiology. 1960;7(4):4-8.
9. Guyton AC HJ. Textbook of Medical Physiology. 12 ed2006.
10. Reber LL, Hernandez JD, Galli SJ. The pathophysiology of anaphylaxis. Journal of Allergy and Clinical Immunology.140(2):335-48.
11. Lagopoulos V, Gigi E. Anaphylactic and anaphylactoid reactions during the perioperative period. Hippokratia. 2011;15(2):138-40.
12. Keet C. Recognition and management of food induced anaphylaxis. Pediatric clinics of North America. 2011;58(2):377-x.
13. Fisher MM. Clinical observations on the pathophysiology and treatment of anaphylactic cardiovascular collapse. Anaesthesia Intensive Care. 1986;14(17).
14. Raper RF, Fisher MM. Profound reversible myocardial depression after anaphylaxis. The Lancet.331(8582):386-8.
15. Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF, Jr., Bock SA, Branum A, et al. Second symposium on the definition and management of anaphylaxis: Summary report Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Journal of Allergy and Clinical Immunology.117(2):391-7.
16. Peters-Golden M, Gleason MM, Togias A. Cysteinyl leukotrienes: multi-functional mediators in allergic rhinitis. Clinical & Experimental Allergy. 2006;36(6):689-703.
17. Cyphert JM, Kovarova M, Allen IC, Hartney JM, Murphy DL, Wess J, et al. Cooperation between Mast Cells and Neurons Is Essential for Antigen-Mediated Bronchoconstriction. The Journal of Immunology. 2009;182(12):7430-9.
18. Simons FE, Ardusso L, Bilo MB, El-Gamal Y, Ledford D, Ring J, et al. World Allergy Organization Guidelines for the Assessment and Management of Anaphylaxis. World Allergy Organization Journal. 2011;4(2):13 – 37.
19. Contributor WC. Signs and Symptoms of Anaphylaxis: Wikimedia Commons, the free media repository; 2015 [updated 25/03/2015. Available from: https://commons.wikimedia.org/w/index.php?title=File:Signs_and_symptoms_of_anaphylaxis.svg&oldid=154681964.
20. Simons FER, Ebisawa M, Sanchez-Borges M, Thong BY, Worm M, Tanno LK, et al. 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organization Journal. 2015;8(1):1-16.
21. Mali S. Anaphylaxis during the perioperative period. Anesthesia: Essays and Researches. 2012;6(2):124-33.
22. Haybarger E, Young AS, Joseph A. Giovannitti J. Benzodiazepine Allergy With Anesthesia Administration: A Review of Current Literature. Anesthesia Progress. 2016;63(3):160-7.
23. Opstrup MS, Malling HJ, Krøigaard M, Mosbech H, Skov PS, Poulsen LK, et al. Standardized testing with chlorhexidine in perioperative allergy – a large single-centre evaluation. Allergy. 2014;69(10):1390-6.
Bibliography
- Guyton AC, Hall JE. Textbook of Medical Physiology 12th Ed. 2006. Saunders
- Sproat C, Burke G, McGurk M. Essential Human Disease for Dentists. 2006.
- Stassen L. Respiratory anatomy, physiology and control of respiration. Lecture for Diploma in Conscious Sedation in Dentistry. Dublin Dental University Hospital. 2017.
- Stassen L. Cardiovascular anatomy, physiology and BP control. Lecture for Diploma in Conscious Sedation in Dentistry. Dublin Dental University Hospital. 2017.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medicine"
The area of Medicine focuses on the healing of patients, including diagnosing and treating them, as well as the prevention of disease. Medicine is an essential science, looking to combat health issues and improve overall well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please: