Design Elements for Building for Dementia Care
Info: 8901 words (36 pages) Dissertation
Published: 10th Dec 2019
Tagged: Health and Social CareHealthcare

Table of Contents
Introduction
This document will consider the design features which have a great deal of importance to those living with Dementia. It will display how to incorporate these into a building to allow a safe and comfortable living environment. Many of those living with dementia either still live in their own home or care homes, both however need to be carefully examined for this matter. During the design stages of a new project there are many elements of design to be considered and with existing buildings there can be alterations made to create a more relaxed home for the person with Dementia. Technical features such as lighting and air quality are only some of the problems and concerns which have to be carefully considered when working with dementia.
The summary to key points of dementia design:
- Small size
- Familiar, domestic, homely in style
- Plenty of scope for ordinary activities
- Unobtrusive concern for safety
- Different rooms for different functions
- Age appropriate furniture and fittings
- Safe outside space
- Single rooms big enough for personal belongings
- Good signage and multiple cues
- Use of objects rather than colour for orientation
- Enhancement of visual access
- Controlled stimuli, especially noise
Background
Dementia is a progressive brain disorder with effects the brains ability to think, remember, communicate, focus, and perform every day actives. As Dementia is a progressive disease the symptoms start out slowly and over time will worsen. According to Dementia services development centre, 65% of people with dementia are aged over 65, and it can also effect few number of vulnerable younger adults who are likely to develop the condition at a younger age. According to Alzheimer’s Society, dementia is increasing throughout the world and within the UK there are more than 815,000 people living with dementia today.
Dementia is the overall term for a number of disorders that effect the brain, Alzheimer’s disease, Lewy body dementia and Vascular Dementia. Are only some. Each condition different, Alzheimer’s disease is the most common with approximately 60-80% of dementia cases. Unfortunately there is currently no cure for dementia, however there is medication and methods to help treat some symptoms and there are ways in which designers can help create a safer and more comfortable environment to help with those day to day problems.
The impairments of dementia which design has to recompense are:
- Impaired learning
- Impaired reasoning
- Perceptual problems
- High stress levels
- Impaired ability to understand other impairments.
Common difficulties of old age such as visual and hearing loss, balance and mobility problems can all have a worse effect on a person with dementia, as they will not understand these impairments and not understand how to live with them.
Vulnerabilities of older people (Moulton & Yang, 2012)





Age-related neurodegeneration
Individual features- age, gender etc.
Brain
Air Pollution
Alzheimer’s disease
Health Issues with older People
Ageing and the respiratory system
Diabetes
Dehydration
Ageing of the eye
Impaired homeostasis
Ageing and the olfactory system
Justification
Throughout this project, the research that will be used will be sourced from dementia charities and development centres, which will be investigated further to widened the knowledge and see how it adapts when in practice. The research put into this project it will be carried out by observing the person living with dementia to give a greater insight to how they deal with day to day obstacles and how practical design solutions can help them live independently longer or live more comfortably. Throughout the world people are living with dementia and in each place the standards and design solutions to help those are the same, differing in climate conditions. Currently having no sure for this brain disorder and the number of dementia cases rising, it is necessary to get the design right for this increasing problem. It is important to many of us that there is a control on this illness and that there are things we can do to help those with dementia.
Aims and Objectives
The main aim of this dissertation is to have an understanding of the diagnosis of dementia, how design can have a great influence and to know how to create the best environment for a person living with dementia. Within this aim, there is a lot of work, research and investigating required to achieve what is hoped.
The objectives of this dissertation are as follows:
- To come out at the end of it all and can pass on knowledge of this topic to others and be fit to integrate this knowledge to projects I work with in the future.
- To fully understand the difficulties a person with dementia has to face on a day to day bases.
- To be fit to have solutions that could help with the living discomfort of dementia
- To understand the effect that design has on a person with dementia.
- To have a good understanding of the design guidance and regulations.
- To have an knowledge on a range of different kinds of solutions that could help improve an environment
- To review any relevant literature.
- To analyse and audit current buildings for the occupants needs.
- Comment on how the design could be improved after research is carried out.
Research Questions
How does design impact those with dementia?
What are the main health issues associated to design?
What design features have influence?
How can be Design Dementia friendly buildings?
How can we ensure the environment is safe and comfortable?
How can technology help those with dementia?
How does sound, light and colour effect people living with the condition?
Methodology
Background
Dementia occurs by damage and steady changes in the brain. The most common causes of dementia contains disorders which the brain cells degenerate and die sooner than they would during the normal ageing process of life.
Dementia can be caused by a head injury, a stroke, or a brain tumour. The first signs of dementia might not be noticed by family or friends until over time it gets worse and the signs become more evident. This usually means that preparing for dementia can be challenging, the house that the person with dementia lives in can be problematic for their day to day living. However dementia practical design solutions are not much different from the solutions within the home of growing older, the design and technical needs of the elderly are much different than a child, and usually a home is modified over time for these requirements.
Good design can help people with dementia optimise functioning, enabling them to adapt and reduce excess disability. The physical and social environment involves not just where the person lives, but also the wider environment, such as parks and gardens, shops, transport, community services, clubs and theatres.
The understanding of what is good design for dementia has developed over time and is constantly being informed by research and expect opinions. It is important that the decisions about the design for spaces used by people with the condition is thought-out and carefully considered with the help of this knowledge to create a safer environment.
Throughout the world dementia is a growing concern in older individuals, and a lot of time has been invested into research to assistance the knowledge and understanding of the cause, treatment and requirements of this mental health illness. There are many different opinions and strategies in different countries throughout the world, however all working well with the requirements.
Evidence shows what delivers dementia-friendly design:
- Specialist knowledge and advice is key at all stages of any redesign or development
- Addressing physical issues such lighting, colour contrast, signage, textures and sensory stimulation is not enough on its own
- Tackling service and physical change together delivers better results
- Technology and adaptations – many of them inexpensive – can have a positive impact
- Using the arts as an integral part of design can offer lasting benefits for people with dementia
- Improving the care environment has a direct link to improved care standards and enhanced reputation.
Library Reading
Library reading will be essential through this project as it requires reading hard copies of books, which may be more beneficial than searching for documents on the internet.
Completion of aims
- To carry out background reading and research in this field.
- Search UUJ library for publications in this subject
- Search on internet for publications and information on this subject
- Use Dementia research centres for information on this subject
- Understand the needs and obstacles a person with dementia has to face.
- Research what is dementia
- Observe a person with dementia
- Understand the Health and wellbeing medical issues and impairments concerned with Dementia
- Obtain information from Health Organisations
- Speak to professional Dementia nurses and carers
- Investigate what issues are more related to design
- To be aware of the existing design guidance and solutions.
- Research what guidance is given by experts
- Obtain copies of the relevant design guidance
- Read and make notes from research
- Use the knowledge to assess dementia friendly places
- Examine care homes
- Examine non dementia friendly spaces
- Understand the importance of different design features
Visual Impairment
What is Visual Impairment?
As people get older, there are a number of changes in normal vision which are simply due to ageing. These include:
- the need for additional light
- increased sensitivity to glare
- reduced peripheral vision
- reduced sensitivity to contrasts
- reduced speed of adapting to change in light level
- reduced visual acuity
- reduced depth perception
- altered perception of colour i.e. being less able to discriminate between unsaturated (less intense) colours such as pastels
With older age, there is a greater likelihood of additional eyesight conditions, being on medication for other conditions, having a form of dementia, and perhaps some or all of these things. What the eye sees, the brain must interpret, and this can vary given different circumstances, type and progression of dementia, and abilities.
Understanding that an older person with or without dementia will probably perceive their surroundings differently is a good starting point for the design of living environments. Good design can help enormously in making it easier to interpret and navigate a building in safety, and the use of colour and contrast can be used in different ways to assist in this.
High contrast
When we want to draw attention to something important, greater contrast helps to highlight it. For example, the toilets are more easily found if the doors are made obvious; a coloured and contrasting toilet seat helps with positioning; stairs can be made safer with a contrasting strip along the front edge; grab rails can be located; the outlines of furniture can be seen more clearly
Low contrast
The opposite effect can be achieved by lowering the contrast. A feature which you may not want residents to be attracted to, such as staff rooms or storage cupboards, can be somewhat disguised by choosing colours which match the background e.g. a white door on a white wall. This is also a useful way of making floorings safer, by keeping to a single colour over different floor finishes, or making changes in the floor colour gradually rather than suddenly. It is the sudden contrast which can make the floor levels look uneven, like a step, and this can cause hesitation and unsteadiness which can lead to falls.
In the context of floors, patterns are best avoided where people are walking. A large or busy pattern can confuse the eye, and again cause hesitation if it looks like an obstacle or a hole. Shiny finishes can look unsafe, so a matte flooring is preferable and people can walk more quickly and safely.
Contrast is the key to vision. If there is no contrast, objects cannot easily be seen and differentiated. Contrast is vital in being able to comprehend the environment and understand the features and elements of a building that we need to use in our ordinary daily lives. As we age we lose the ability to differentiate colours clearly, our perception of depth diminishes, there is a loss of visual acuity, we have less spatial awareness and our sensitivity to contrast lowers. Without good contrasts, the world becomes hazier, we struggle more and more to make sense of it and we function in life with less confidence.
Why is lighting important?
The living environment for a person with dementia can help with the impairments they are living with. People with dementia do not have the ability to do things they used to be capable of, impairments through old age increase and elements of their environment can have an effect. It is important that the light around them is throughout and designed for their needs, to ensure their safety and so they can experience more independence. People with dementia need more attention to detail at the design stage as they need help to see what is around them and where they are, using light and objects such a furniture. It is vital that the person can find their way around the environment such as a nursing as they will be unsure of the environment and may feel isolated that they are not in their own home, it is important that they see the different spaces and area like the living room, toilets around them so they don’t feel lost or unsure. They should have the chance to see and enjoy the changing of the seasons, helping them stimulate memories and aid enjoyment and pleasure of nature. The lighting should help them see other people faces, gestures and their location, and to have the chance to join in on day to day, ordinary routines such as washing up, getting dressed, sorting clothes and laying the table for dinner. Without good lighting all these normal activities and routines would be impossible and a lot harder to do for a person living with dementia. Poor lighting can result in anxiety and also accidents, which should be avoided due to the vulnerability of the resident and their body.
People with dementia can also mistake aspects of their environment, for example:
- Reflections on polished floors, making them look like wet floors
- Reflections on mirrors, the person with dementia will not understand that it’s their own reflection but maybe someone else in the room.
- They will see shadows as objects and likewise objects as shadows
Aging of the eye
Our sight is one of the most important senses and without it we would find our day to day routines and activities much different and lot harder to assume. When designing a residence for older people and people living with dementia it is important that we be aware of this impairment as it can significantly impact a person’s interpretation of surroundings which can lend to further confusion, reading of visual cues such as signage and memory prompts, effective participation in activities and stimulation and their safety which can increase their chances of falling. As we get older our eyes start to change, and our performance starts to deteriorate. The eye loses its capacity to focus at close and distance ranges, this can also occur in young life. According to RNIB 2006 approximately four million older people not have go for regular sight check-ups, which means that the majority of older people surer from impaired vision but do not have it seen to or anything prescribed to help. Around 270, 000 people over the age of 75 experience avoidable sight loss due to wearing out dated glasses or no glasses at all.







Recreation of age-related lens changes
Recreation of age-related lens changes
Normal vision
Normal vision
Recreation of Cataract
Recreation of Cataract
Recreation of macular degeneration
Recreation of macular degeneration
Recreation of Glaucoma
Recreation of Glaucoma
Recreation of hemianopia
Recreation of hemianopia
Visual deficiency is strongly related to falls and hip fractures with older people, this can be a serious issue but can be reduced by good design and lighting. Must falls that occur usually start come from the person not having great vision, in 1999 some 189,000 falls that required hospital treatment occurred in individuals with visual impairment, 89,000 of those were accredited to the visual impairment, with an estimated cost of £269 million from the NHS according to Scuffham et la 2002.
Older people in nursing homes are at a higher risk of falls and this is due to age, physiological factors, vision, and medication. Other risks include environmental issues such as poor light and flooring being too slippery and uneven. Impaired vision and sight problems will also effect the persons balance, coordination and mobility.
Improvements that can be incorporated into the environment to help prevent falls and improve the space in with a person with dementia lives in are simple factors such as:
- Training staff to communicate better to understand the person needs
- Reduce physical hazards
- Improve colour perception
- Increase the size of signage
- Improve lighting by minimising glare, increasing light levels, balancing light levels and increasing contrast.
Light can also have an influence on a person’s health by regulating our bodies to a sleeping pattern and improve the quality of sleep, its helps maintain bone density and strength through vitamin D which the body produces from the UV in sun light. It is important that it is dark in order to sleep during the night, however in an area that has people with dementia it is also vitally significant that safety lighting is in place. In the event of someone deciding to get out of their bed in the middle of the night confused, the environment is illumined so that they can make their way safety and see where they are going.
Design Challenges
The main elements of a dementia friendly lighting are to use domestic styled fittings to help promote a recognition of place, increased levels of light to twice the normal lighting level, use daylight wherever possible in the building, and to expose people to the 24 hour cycle of light and dark.
Using domestic styled light fittings should enable a sense of home to the residents in a care home, using this style of fitting will give the feeling there are in a familiar environment that they are most comfortable in, and such like their own home. Although care home and hospitals are workplaces it is most important that the facilities is accommodating to suit the residents and patients’ best. It should portray a sense of home and this can be achieved by using more traditional and domestic style light furnishing as well as the fittings.
Increasing the level of light will help assist the person with dementia understand its surroundings better by being fit to see well. Increasing the light level by two times the normal light, will give a more effective measure for those with dementia, when the light is increased the reflection on materials and other surfaces must be considered to reduce the reflect glare.
Daylight should be used in as many appropriate places as possible where is delivers good rendition. It can be delivered in through elements such as windows, skylights, doors with glazing, and light pips, however where these elements exist there must be measures installed to cut light out such as, curtains, blinds, special glass, and external shading devices. These are essential to a dementia friendly design to enable the management of light entering the building as light from the sun is beneficial to improve our health, it can also be too strong. This can occur a problem when the building has been designed to have bigger area windows, rooms on higher levels where there is less external obstructions, the light transmission through the window is enhanced, the rooms surfaces reflects more light and where the room is smaller in proportion to the window.
Exposing people to bright light in the morning and during the day will create a better and more normal circadian rhythm and they will sleep more effectively at night. Care home all should have safe outdoor spaces, and having these areas will help with receiving more natural day light.
Even and consistent Try to keep light at a similar level throughout the room as uneven brightness patterns can produce frightening shadows causing agitation and confusion. Where transitions are necessary – for example, between outside daylight areas and indoor spaces – changes should be gradual as older eyes adapt much more slowly to changes in light levels.
Night-time illumination Careful attention to night-time lighting can help reduce the risk of falls – ADRD sufferers are three times more likely to fall than healthy older adults and they take much longer to heal. Strips of LEDs around doorways and along pathways (e.g. to the bathroom) were found to work better than leaving a dim nightlight on in these areas.
Guidance for particular areas
Through the observance of a dementia based nursing home, the characteristics found most beneficial for residents and caregivers for different rooms were:
Living Room
- For general lighting use lighting like chandeliers or ceiling mounted lights with curved opal visors so that light is shed on the ceiling and walls, and lamps cannot be seen.
- For areas that are used for reading or games, table lamps and floor lights increase the level of light and can be moved to areas where appropriate
- Avoid the use of dark carpets , curtains and furniture and ensure the walls are decorated with light colours
- Light coloured diffusing blinds should be used to offer relief from direct sunlight.
Kitchens
- for general lighting use long light sources like fluorescent tubes and avoid spot lights
- On the wall mounted cupboards, low profile fluorescent tubes can be fixed to the bottom to achieve light are areas where cooking tasks will be applied. These lights should be covered and out of vision
- Use light coloured vinyl flooring
- Avoid very dark and speckled work surfaces.
Dining Room
- Multiple lamp fittings should be located above dining tables
- Wall mounted lamps will help with light reaching the dining table and will also help with appearance
- Use compact fluorescent lights in table lights and any other light that could be accidently touched
- Use white dishes with a contrasting coloured dark rim.
Toilets
Bedrooms
Corridors
| Lamp Type | Energy Use | Light Quality | Useful Life (hours) | Light depreciation | Re-strike Time | Colour Rendition | Lamp Cost |
| Fluorescent (electronic gear) | Very low | Very good | 16,000 | 10% loss at 16,000 hours | Instant | Good | Medium |
| Fluorescent (conventional gear) | low | Good | 8,000 | 17.5% loss at 8,000 hours | A few seconds | Suitable | Medium |
| Compact fluorescent (separate gear) | low | Good | 12,000 | Poor output after 12,000 hours | Instant | Good | High |
| Compact fluorescent (gear within lamp base) | low | Suitable | 8,000 | Poor output after 8,000 hours | Instant | Good | High |
| Tungsten- halogen | High | Excellent | 2,000 | Lamp fails before critical reduction | Instant | Excellent | Medium |
| Light emitting diodes (LEDs) (domestic style ) | low | Very good | 25,000- 30,000 | Typically 10% loss at 15,000 hours | Instant | Excellent | Very high |
Lamp Characteristics
Bright light therapy Lots of studies have shown that bright light therapy (at least 1,000lux) for two hours each morning had a variety of benefits: improved night-time sleep, increased daytime wakefulness, reduced evening agitation and better rest/activity patterns overall. Bright light therapy doesn’t involve extra effort or time; for example, patients can have a light box switched on whilst they’re watching TV or having breakfast
Indirect bright light improves circadian rest-activity rhythm disturbances in demented patients
Biol Psychiatry. 1997 May 1;41(9):955-963
Light is known to be an important modulator of circadian rhythms. We tested the hypothesis than an enduring increase in the daytime environmental illumination level improves rest-activity rhythm disturbances in demented patients. Actigraphy was performed before, during, and after 4 weeks of increased illumination in the living rooms of 22 patients with dementia clinically diagnosed as probable Alzheimer’s disease, multi-infarct dementia, dementia associated with alcoholism, or normal pressure hydrocephalus. The results indicated that during increased illumination, the stability of the rest-activity rhythm increased in patients with intact vision,but not in visually impaired patients.
Indoor air quality is vital to our experience of a space it is affected by high and low temperatures, air that is too dry or too moist, contaminants and pollutions. All of these directly affect our respiratory and cardiovascular systems. The degree to which we will be affected by poor indoor air quality will vary depending on the intensity and duration of our exposure to it. Older people, who are often less mobile and spend a lot of their time indoors, can be particularly susceptible to poor indoor air quality. People with dementia may face the additional challenges of not being able to communicate their concerns or discomfort.
The air inside our buildings are either sourced into the building naturally or mechanically ventilated, however way, the air that is held inside our homes can be poor quality than the local outdoor air. This is due to the contribution of emissions from people, materials, finishes and heating systems. All these factors that pollute the air around us can affect us significantly affect our health, and those who’s health is susceptible, it can create a lot more concerns in their well-being. The occupants of a building with poor air quality can be referred to as ‘Sick Building Syndrome’, this condition can result in the occupants experiencing acute health and comfort effects, though there are no specific illness or cause can be identified. Long term exposure to these contaminations from the indoor environment can have consequences of life threating illnesses.
‘Clean air is a basic requirement of life. The quality of air inside homes, offices, schools, day centres, public buildings, health care facilities or other private and public buildings where people spend a large part of their life is an essential determinant of healthy life and people’s well-being’ (WHO, 2010)
Pollutants
Cupboards/shelves: formaldehyde, dust mites

Kitchen unit & tops: dust mites, formaldehyde
Windows: pollen, mould




Damp: Mould Spores







Curtains/lampshades: dust mites
Gas cooker: Nitrogen Dioxide
Floor boards: formaldehyde
ards: formaldehyde
Wall finishes: paint toxins, wallpaper toxins, adhesives
Damp: mould
Carpet: formaldehyde, dust mites, mould
Insulation: formaldehyde
What is Ventilation?
Ventilation is airflow resulting from a design intention
Air infiltration is unintentional and uncontrollable leakage of air because of imperfections in detailing and construction. Air infiltration can have a significant adverse impact on the amount of heating or cooling required and may be pathway for noise and pollution. Air infiltration should therefore always be eliminated in favour of ventilation that is well controlled when, where and in the quantity required- giving rise to the maxim ‘Built tight – ventilate right’.
Improving thermal comfort and indoor air quality through the provision of fresh air is vital to an individual’s perception of a space, their health and well-being, as well as staff sickness rates and productivity. We ventilate in order to:
- control air quality and to remove pollutants that can be hazardous to health and our buildings
- remove heat and smells directly from localised sources and areas such as kitchen and bathrooms
- Deliver mechanical heating, cooling and humidity controls.
- Reduce the impact of cold winter drafts and summer over heating
- Control moisture and condensation and prevent its side effects
- Provide oxygen for breathing
Why is ventilation important?
People living with dementia may be unaware of their environment and may have trouble communicating or taking actions of their discomfort. It is important that carers in health facilities are trained to understand and respond to the people they are caring for. It is significant that good communication is kept between the carer and the people going through the journey of dementia. People living at home with dementia also may be unware of challenges and may need assistance with the control of their environment. Within the home it is important that smoke and carbon dioxide detectors are installed and working correctly, as some elderly people and more cases, people with dementia lose their sense of smell and therefore won’t have the ability to sense danger from the kind of situation. It is important that ventilation is given detailed consideration at the design stage, for the needs of its users.
Relative Humidity Issues
Relative humidity that is too high or too low can affect those in a more vulnerable state and cause various health issues. Relative humidity which is too low is likely to increase the spread of cold and flu viruses and the irritation and inflammation of nose and respiratory passages. High relative humidity can then lend to the spread and growth of airborne allergens such as moulds spores, bacteria and dust mites. Both low and high humidity can lend to more common health matters such as asthma, due to the vulnerability of the occupants health, this can lend to more serious problems and needs to be resolved in the design of the building. The ideal percentage range of relative humidity for a person with dementia is between 40% and 60% according to Arundel et la, 1986.
Thermal Comfort
Thermal comfort is defined as being an individual’s state of mind in relations to whether they feel too hot or too cold. However thermal comfort depends on more than just the temperature of the air, it can be subject to the temperatures of the surrounding surfaces, air velocity and relative humidity. As well as these factors, thermal comfort depends on the individual and influences of the amount of clothes they are wearing, and the physical activities and the degree of impairment of homeostasis.
The building form will also effect thermal comfort within the internal space, considering the orientation of the building and its spaces within, temperature can vary due to solar gain and draughts and
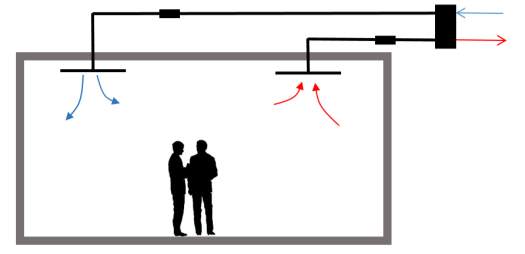
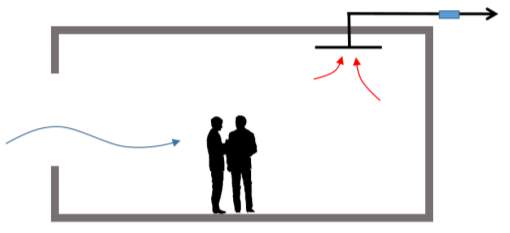
Natural Ventilation
Natural ventilation, uses natural outside air movement and pressure differences to both inactively cool and ventilate a building.
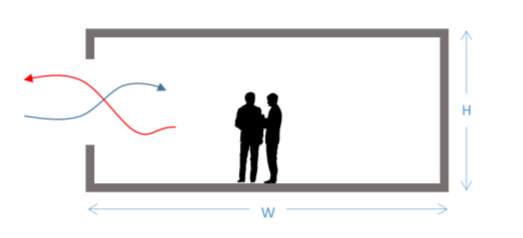 Single sided ventilation, one opening is effective to a depth of about two times the floor to ceiling height. W ≤ 2 X H
Single sided ventilation, one opening is effective to a depth of about two times the floor to ceiling height. W ≤ 2 X H
Warm air out
Fresh air in
Warm air out
Fresh air in
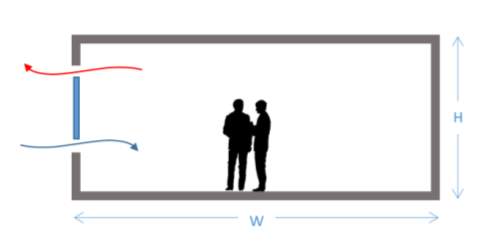 Single sided, double opening ventilation is effective to a depth of about 2.5 times the floor to ceiling height. W ≤ 2.5 X H
Single sided, double opening ventilation is effective to a depth of about 2.5 times the floor to ceiling height. W ≤ 2.5 X H
Warm air out
Fresh air in
Warm air out
Fresh air in
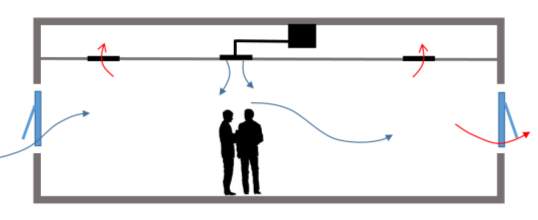
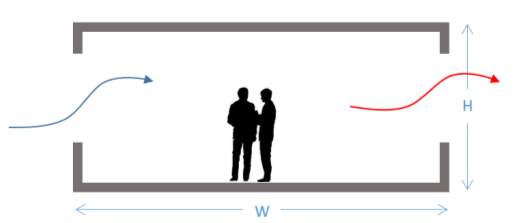 Cross ventilation is effective to a depth up to 5 times the floor to ceiling height. W ≤ 5 X H
Cross ventilation is effective to a depth up to 5 times the floor to ceiling height. W ≤ 5 X H
Warm air out
Warm air out
Fresh air in
Fresh air in
Mechanical Ventilation
What is mechanical ventilation?
Design Notes
Throughout my research for my dissertation I under took a study of observation of a working dementia nursing home and a normal household. The nursing home facilitates those with dementia who no longer can be cared for at home, for many reasons, lack of dementia friendly design could be one. It is essential that there are care facilities available for those with dementia as this condition requires 24 hour care in a safe environment, as a lot of dwellings are not designed to accommodate those with dementia as dementia happens in later life. As explained through this report dementia patients require a lot of consideration due to their impairments and discomfort. In this section I will describe my experience in a nursing home and using an audit tool explain how the nursing home assists people with dementia with its design features. To further my knowledge on this topic, a normal house hold dwelling was observed to compare the two environments and identify Cleary what the mean issues are to achieve a dementia friendly design.
Audit Tool
The Dementia design audit tool that was used for the inspection of a nursing home and house hold was an audit tool published by University of Stirling, Dementia services development centre. This organisation works to improve the understanding and the services given to people living with dementia, they work with university of Stirling as a charity based research and development centre. They aim to improve the standard of living for those with dementia, to enable the best environment possible. Creating an audit tool allows their knowledge of dementia to filter through homes, hospital and care accommodations internationally and provide enhanced Dementia friendly spaces. The audit tool provides an outlined design information generated by professionals and experts. The constants involved in this scheme are experienced designers and health professionals. They have managed to create a very beneficial tool to analyse homes and care accommodations to ensure they achieve the best environment for a person with dementia.
The Audit tool involves a process of moving through different areas and rooms of a building to access the design and layout using different standards. It uses a scoring system to evaluate the overall performance, standards and principles of the building. The Dementia Services Development Centre offers this as a service, to audit and then to formally certify the building in accordance to the score attained
- Gold (90% +) exceptional example of design for people with dementia
- Silver (75-89%) good example of design for people with dementia
- Bronze (60-74%) a satisfactory example of design for people with dementia
As the nursing home is a new environment for many people, it is as well their new home, so it is important that the design feels homely and therapeutic as well as being accessible.
The areas which were examined with the help of the audit tool were:
- Corridors
- Living Room
- Kitchen
- Dining Room
- Bedroom
- Toilet
- Outdoor area
Following the guidance of the audit tool the design and layout of a dementia unit in a nursing home was accessed and reviewed and the following was found.
Corridor/ Entrance
The Entrance of the nursing home lending into the dementia unit was a promising start, it was clean, clear of obstruction, level access and very welcoming. Entering the building there was space between two different sets of doors, first set of automatic doors and the second there locked to ensure safety of the residents inside. The door entry systems was unobtrusive for the occupants inside the building.
The nurse’s station/ reception desk was located close to the front entrance, and adjacent to it was the living room where the majority of residents spent their day. This was found an exceptional layout from the staff, as they you manage their theory work while maintaining a close distance to the residents.
The corridors lending through the unit were an accessible width for passers and furniture, and seating was provided for opportunities of rest. The lighting through the corridors was consistent, ranging in different types, up standing, wall mounted and ceiling chandeliers. Switches were located outside each door lending into additional areas with a contrasting colour from the wall. A continuous patterned red coloured carpet, with dark stained doors and skirting contrasted against the walls along the corridor. However the building would benefit strongly from a plain red carpet as the patterns in flooring, some residents may misinterpreted the patterns for objects on the floor and may result in a fall. The dark contrasting doors and skirting enables the dementia patients to distinguish where the doors are located and so they don’t react to being lost in the corridor. The corridor was broke up by old fashioned furniture and iconic pictures and paintings to stimulate memory and divided into different areas for fire regulations and separated by sets of fire protected doors.
The corridor closer to the bedrooms was isolated from natural light due to the design and layout of the building, however the entrance received a lot of natural light and the artificial lighting through the corridor was ideal and efficient to manage a recommended amount of light.
Signage
Doors
Living Area
As stated before, the main living area is based opposite the nurse’s station which allows easy communication between resident and care giver. The main theme in this room is a relaxed, rich vintage style with is appropriate for the arrange age of the residents, this interior creates a therapeutic environment as it will support the occupants and make them feel like they’re in their own home or somewhere they have been before. The carpet flooring followed through into this space from the corridor, and large, glazed, opened doors creates an open and very comfortable environment for the residents to sit, communicate and watch television. The space includes a set of patio doors which follows out onto a garden area, the doors are dressed with wall colour contrasting curtains for décor and blinds to deny any unwanted light to enter the room when needed. Other from the natural light the room is installed with several domestic style lights including chandeliers and table lamps. The room is a suitable size for its purpose, allowing the residents to sit comfortably together however not to close for any interference. Toilets are closely based to this area of living, with large and clear signage specifying to the resident where they are located.
Kitchen/Dining Room
The Kitchen and Dining area is situated down the corridor and just around the corner from the living and reception area. Both the dining room and kitchen are based in the same location, opposite one another. This allows the residents and staff to use the kitchen and be travel a sort distance to the adjacent room. The kitchen is a small area with a small kitchen table, allowing this facilities to entertain the clients when they feel the need to take care of those day to day activities. The kitchen must be safe from any hazards, such as the cooker. This kitchen is for patient use only, and is not a fully functioning kitchen as the staff of the nursing home do not prepare or cook the resident’s meals in this area, it is simply there for those basic chores of a household. Many residents will find a comfort in cleaning up, and washing up dishes from the kitchen and this save allows that to happen. The lighting in the both areas is delivered by large windows, offering both natural light and views to the external spaces. The traditional domestic styled kitchen continues the vintage interior throughout the building for that sense of homeliness, comfort and recognition for the clients. The kitchen units are all labelled with what they contain for the residents to easily find and easily complete the task, these signs are clearly marked with text and pictures to indicate to the brain effortlessly what each unit encloses. The kitchen also has a patio door lending out onto the same space in which the living area does. The dining room is opposite the kitchen, with basic domestic fashioned furnishings, it holds several large tables and chairs with will permit residents the room to eat and not become distracted by the person next to them and will allow staff to interact with task of eating. The room is suitable for this purpose as the space has no interferences to disturb the people with dementia that find it difficult to complete simple tasks.
Bedroom
The bedrooms are positioned further down each of the corridors, these rooms must be private areas for the clients to have their own space. Each room that the residents use in the building must have a clear focal point to indicate the purpose of the room, in this instance the bed must be the first feature which I seen, and differing furniture around the room for the residents personal clothes and belongings. Windows must be designed and included to submit a sense of day or night in the room and to also permit various views to outside. Each room in the nursing home was large in size, with an ensuite connected to the bedroom, this also allows provision for personal space for toilet facilities and bathing. It will also ensure ease of access to a toilet facility during night-time hours and minimising the travel distance to toilets located near to the living and dining areas. The toilet doors are clearly marked with signage to state what the room, and when the door is left open the toilet is visible from the bed. The majority of the windows surrounding the building have a low sill height to allow residents to sit and view the outside settings rather than stand and cause tiredness and frustration. It is also important that the staff members help keep this space tidy and free from obstruction for the person with dementia.
Toilet
It is vitally important that the doors throughout the building are contrasted to the colour of the walls, and the handles are different from the general material and colour of the door. The door should be easily opened with no pressure against the force to open. In as many places possible the doors should include glazing to allow the person to see into the room and view its purpose. However is it extremely significant that toilet doors have no glazing, and toilets provided by the lounge area have an additional corridor and door to provide privacy from the central area. Lighting provided into these spaces were ideal for the use and enhanced the visibility of the room. Also helping with the clear visual space was the contrast of colour, hand rails and the toilet seats were a dark navy against the white features in the toilet. Mirrors were covered to ensure that the person with dementia didn’t get confused with their own reflection and become distracted and uncomfortable. The flooring in the toilet areas were a non-slip, matte material for the purpose of the room being a wet area and to ensure the ease of cleaning.
Outdoor Area
Case Study
King’s College Hospital NHS Foundation Trust (Older Persons Ward / Environment)
Marjory Warren Ward is a 30-bed ward on the Health and Ageing Unit. The ward treats and cares for older people, many of whom will have dementia, delirium or a combination of the two conditions. The ward was not originally designed to specifically accommodate the needs of patients with dementia.
Hospital admission can be a distressing and overwhelming experience for patients with dementia. Environmental factors can trigger behavioural changes in this patient group, whereby patients often wander due to under-stimulation or because signage is inadequate and they are looking for something. It is recognised that a lack of stimulation and boredom can cause agitation.
The main aim of the project was to improve the general ward environment for people with dementia by enhancing the décor to ensure it complies with current best design practices. The project team identified four main areas for improvement:
- Entrance to the ward
- Day room
- Nurses’ station
The existing dayroom was transformed into a multi-sensory space. The room needed to be flexible enough to be used both for agitated patients who might require a low stimulus environment and as a space where structured and unstructured activity could also take place. Lighting, imagery and sounds can also be adjusted to suit mood in addition to the provision of reminiscence materials and atomisers. Portable sensory equipment is also provided to stimulate activity in patients who are bed-bound or who are confined to a side room for infection control reasons.
 Marjory Warren Ward is now one of the highest scoring wards in the trust’s patient satisfaction survey, which includes the environment. Patients feel more confident when mobilising. Anecdotally, when patients are transferred to Marjory Warren Ward from the Medical Assessment Unit with one-to-one nursing, this is not required 24 hours after admission to the ward. The overall impression from patients, staff and visitors is that the environmental improvements have had a significant positive impact on patient well-being and also on staff motivation levels.
Marjory Warren Ward is now one of the highest scoring wards in the trust’s patient satisfaction survey, which includes the environment. Patients feel more confident when mobilising. Anecdotally, when patients are transferred to Marjory Warren Ward from the Medical Assessment Unit with one-to-one nursing, this is not required 24 hours after admission to the ward. The overall impression from patients, staff and visitors is that the environmental improvements have had a significant positive impact on patient well-being and also on staff motivation levels.

Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Healthcare"
Healthcare is defined as providing medical services in order to maintain or improve health through preventing, diagnosing, or treating diseases, illnesses or injuries.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




