Flight Anxiety Modality Questionnaire (FAM): How Do I Express My Fear?
Info: 9455 words (38 pages) Dissertation
Published: 25th Feb 2022
Tagged: Psychology
Contents
Click to expand Contents
1. Introduction
1.1 Biographic data
2. Presenting problems
2.1 Coping strategies
2.2 Treatment goal
2.3 Diagnostic criteria
2.4 Standardised measures
2.5 Suitability
3. Case conceptualisation
3.1 Vulnerability and precipitating factors
3.2 Formulations
4. Treatment Plan
5. Course of therapy
5.1 Assessment session
5.2 Session one
5.3 Session two
5.4 Sessions three and four
5.5 Session five
5.6 Sessions six, seven and eight
5.7 Session nine
5.8 Sessions ten and eleven
5.9 Sessions twelve and thirteen
6. Outcomes
7. Future Treatment Plan
8. Discussion
9. Appendices
9.1 DSM-V Diagnostic Criteria for Specific Phobia
9.2 Kirk and Rouf (2004) model of Specific Phobia
9.3 Flight Anxiety Situations Questionnaire (FAS)
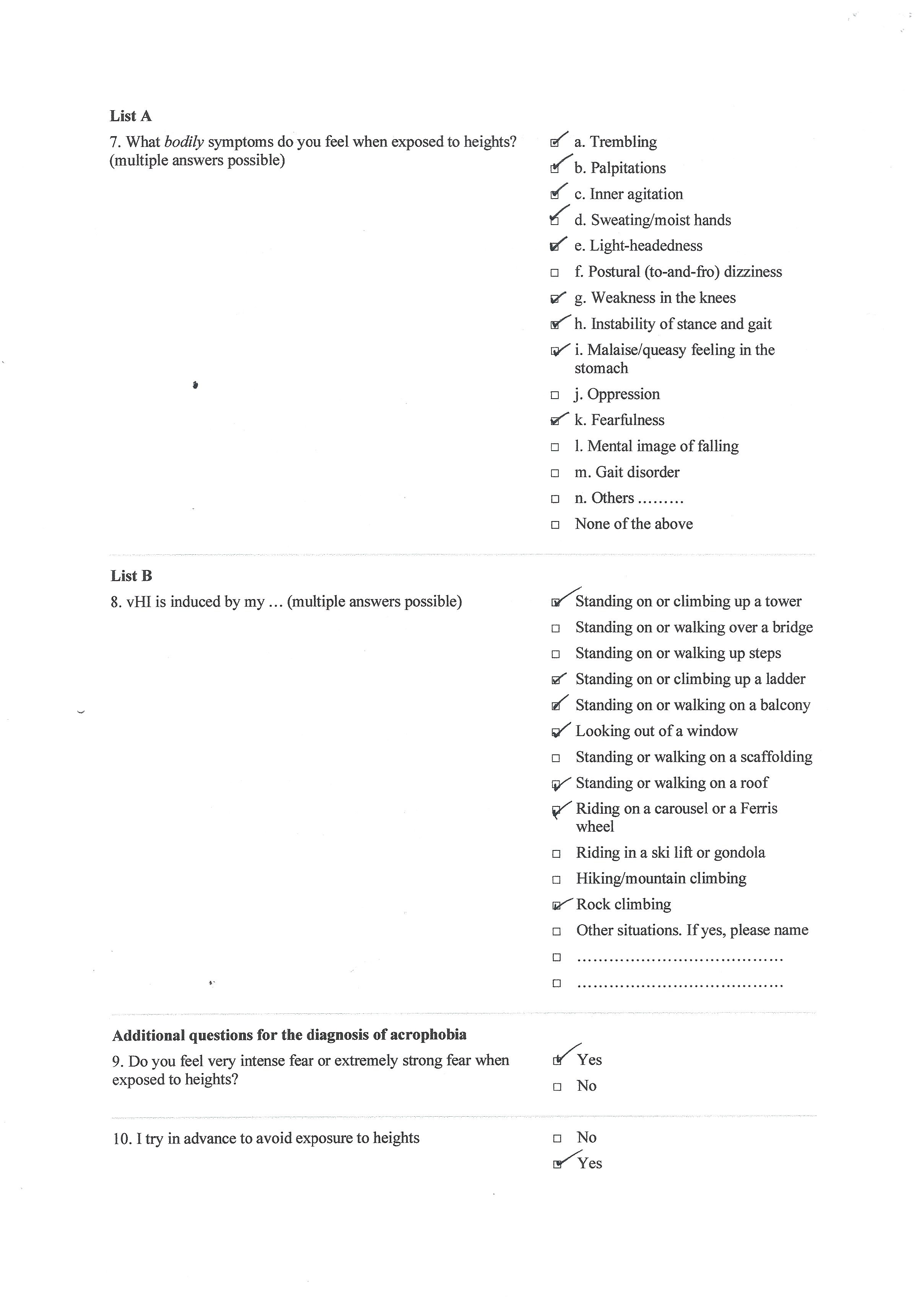
9.4 Flight Anxiety Modality Questionnaire (FAM)
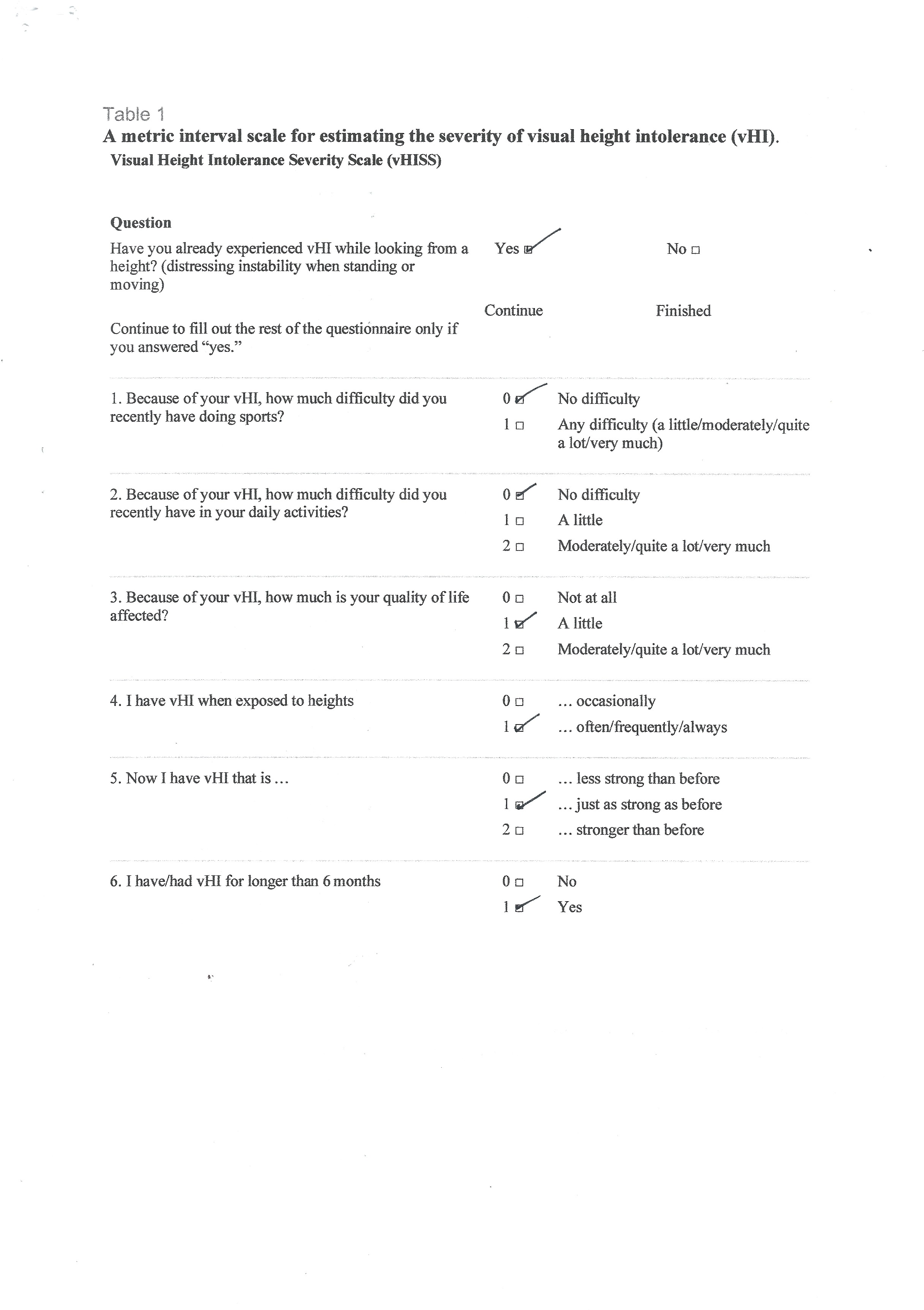
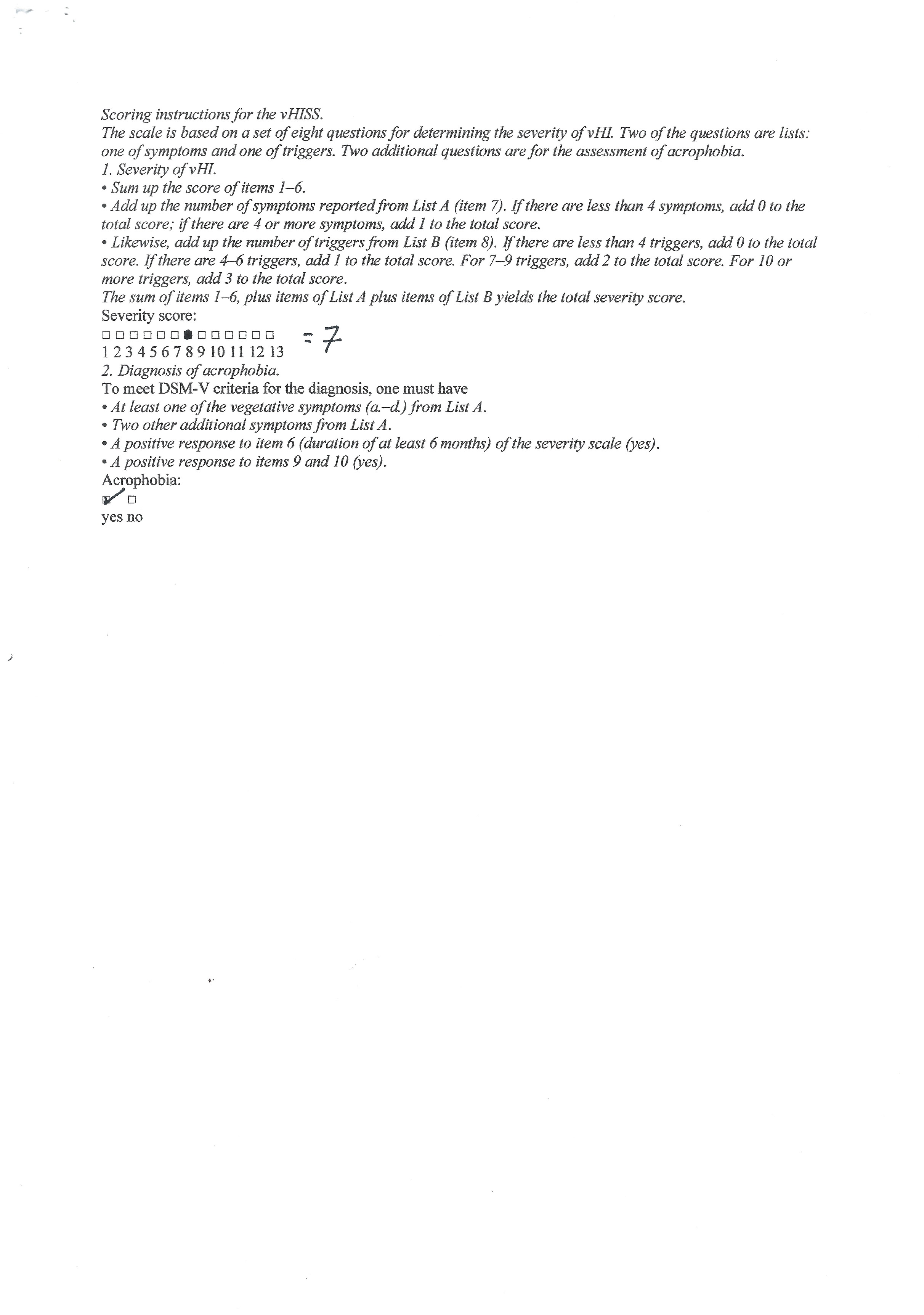
9.5 Visual Height Intolerance Severity Scale Huppert, Grill, and Brandt, (2017)
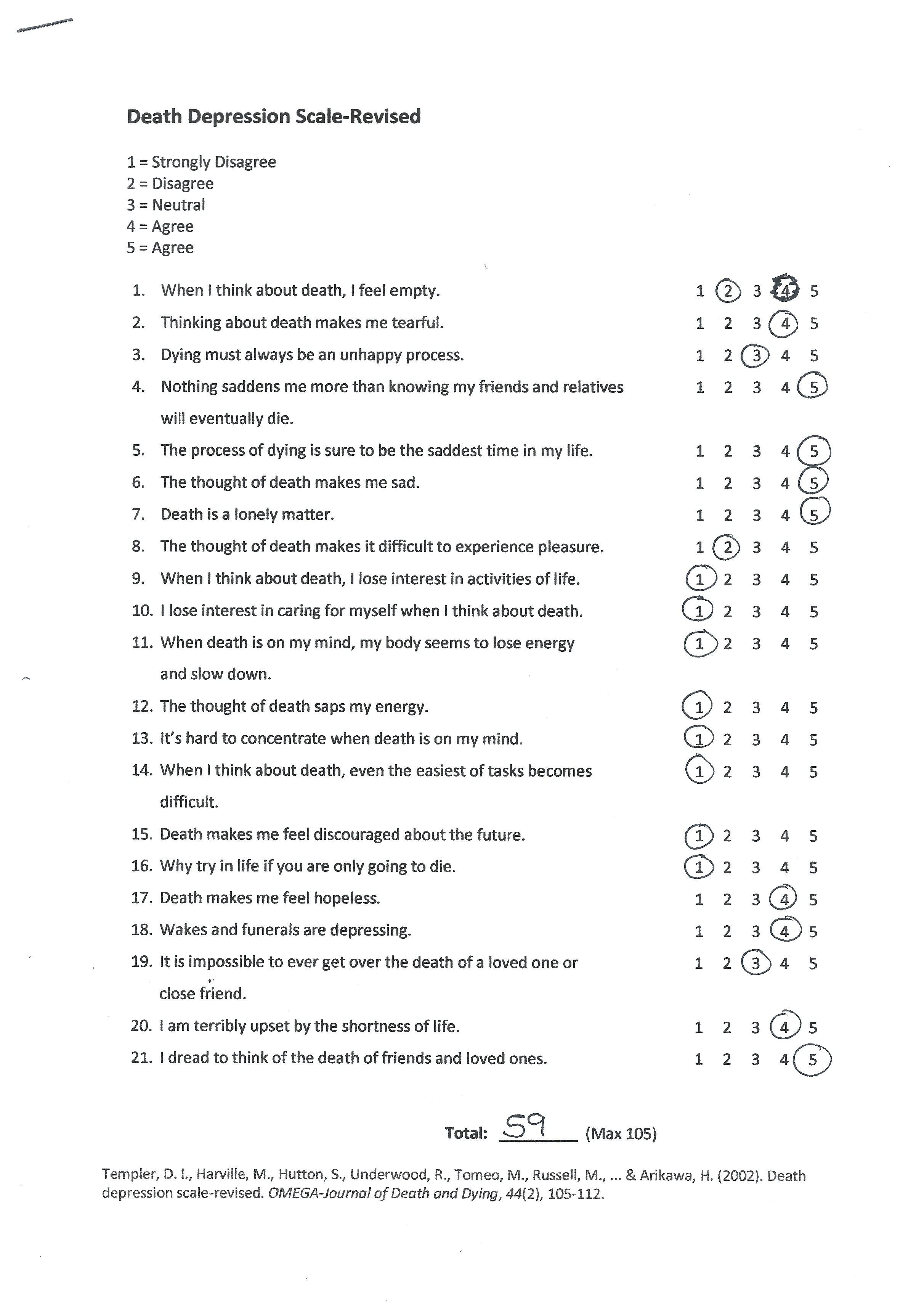
9.6 Death Depression Scale, Templer, Lavoie, Chalgujian, and Thomas‐Dobson, (1990)
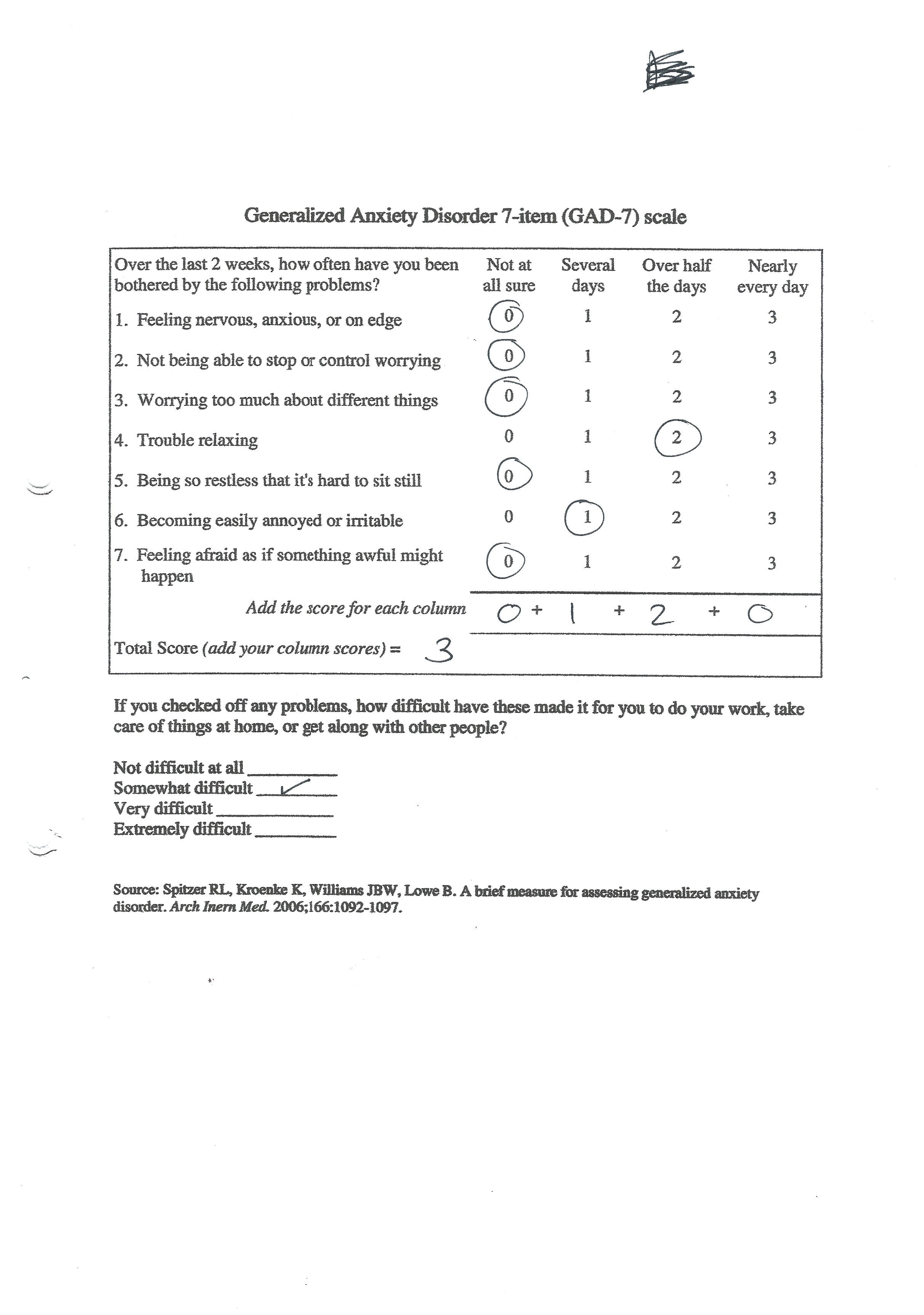
9.7 General Anxiety Disorder 7 (GAD-7)
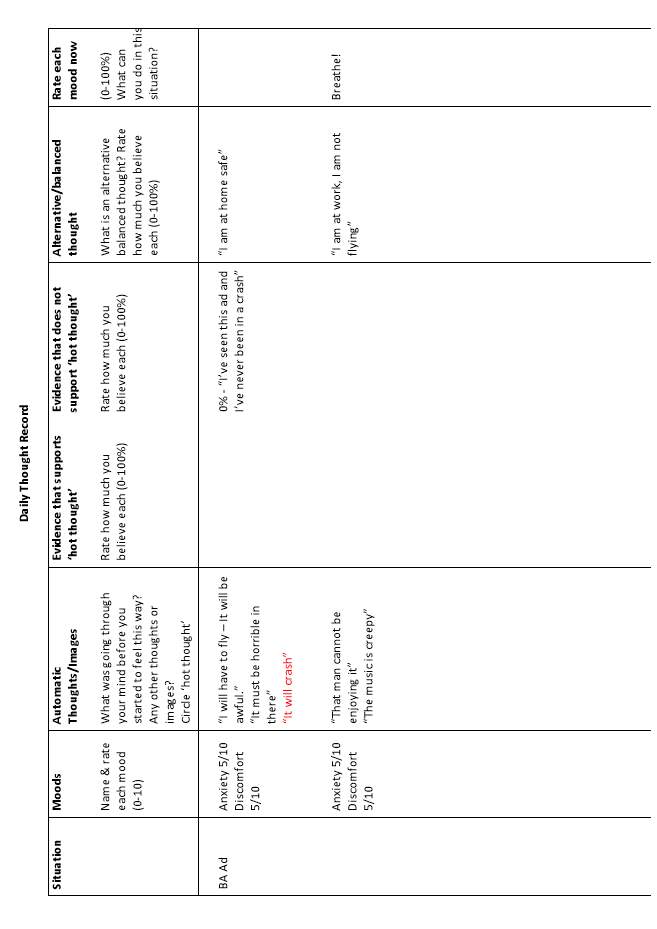
9.8 Thought Record 1. Watching a flight advertisement
9.9 Transcription of downward arrowing
9.10 Aircraft Safety Handouts
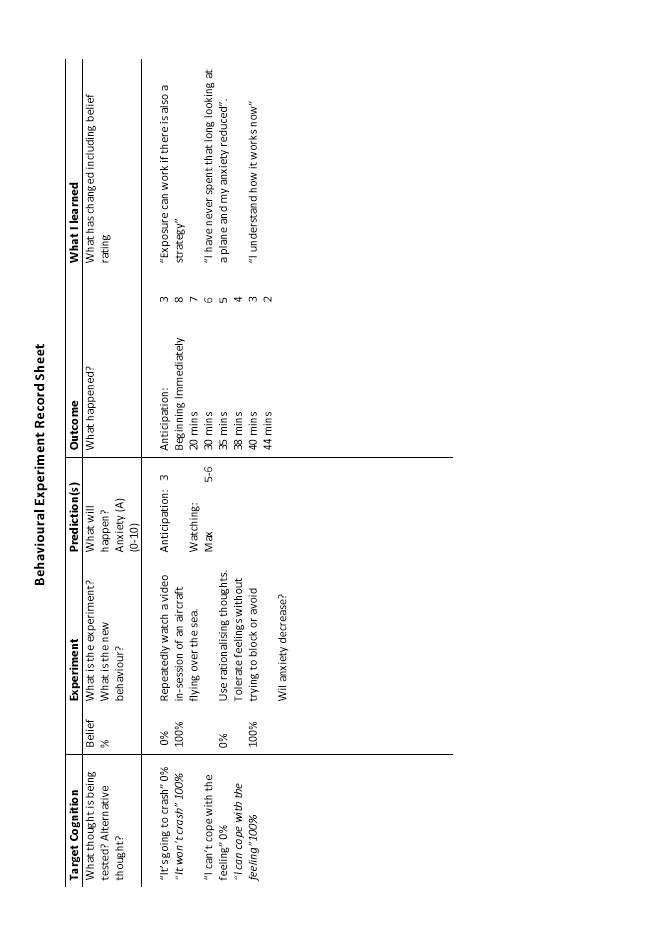
9.11 Behaviour experiment, watching an airline advertisement
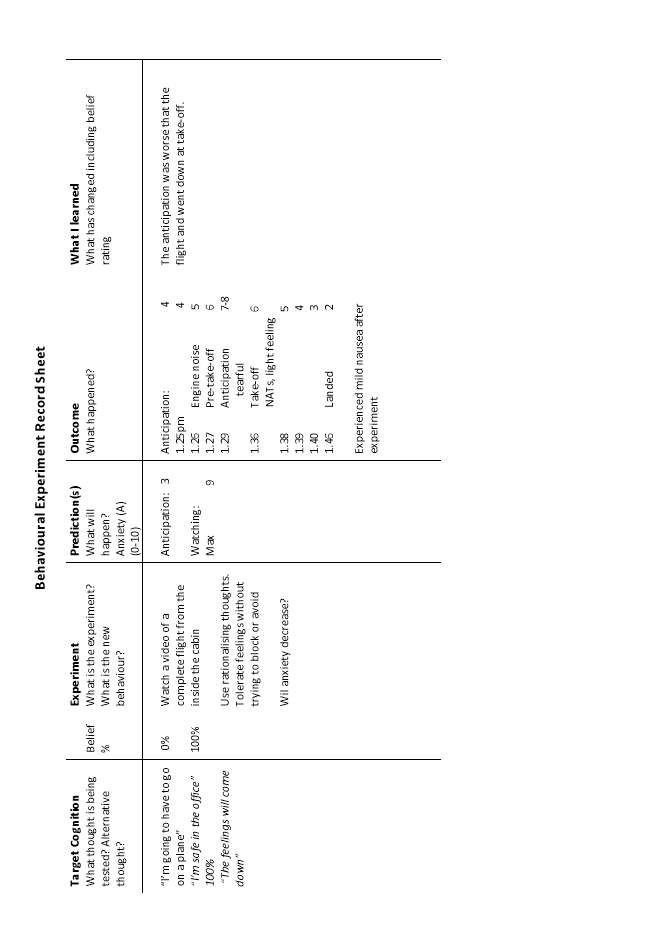
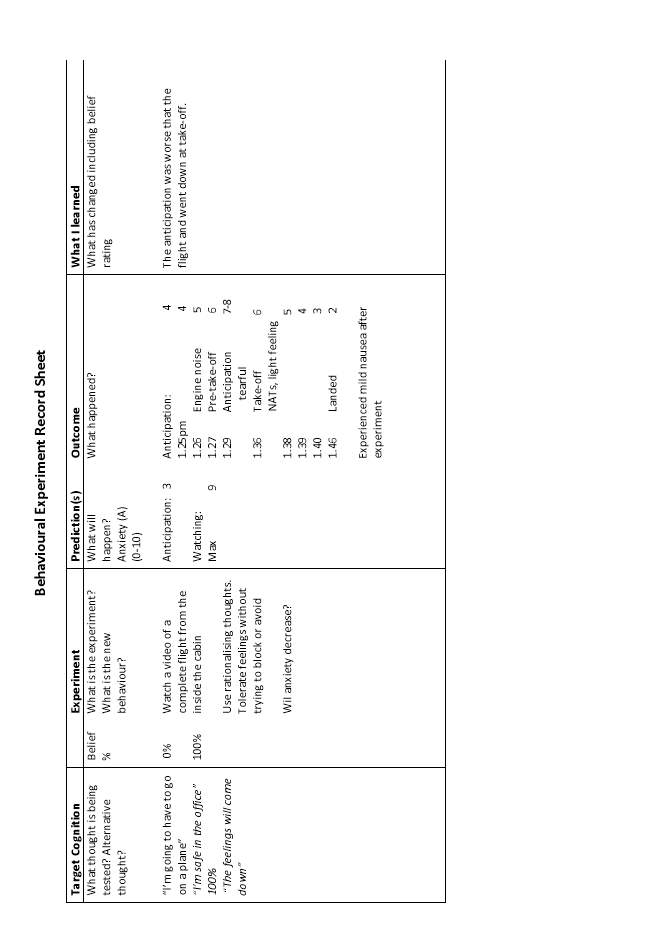
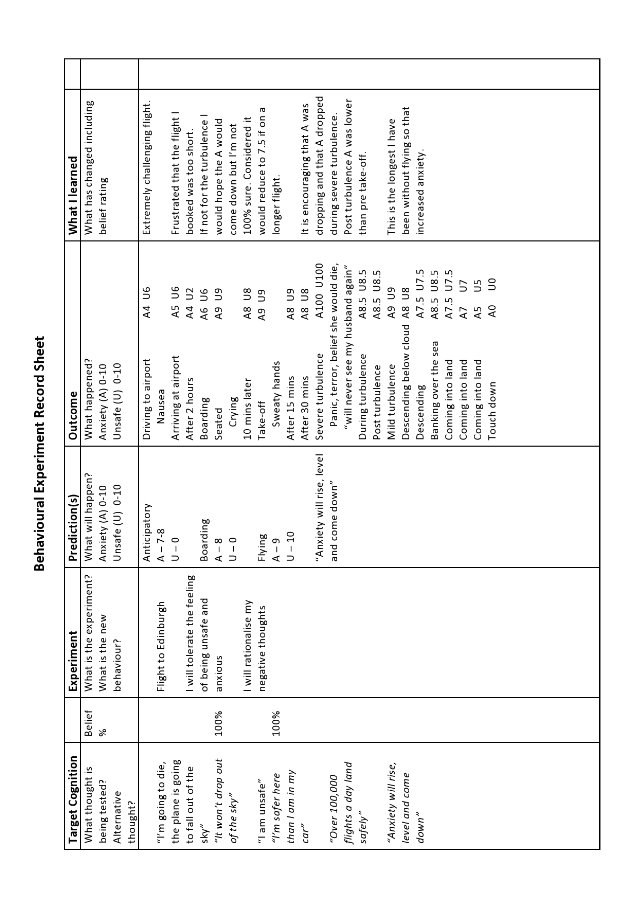
9.12 Behaviour experiment, complete flight
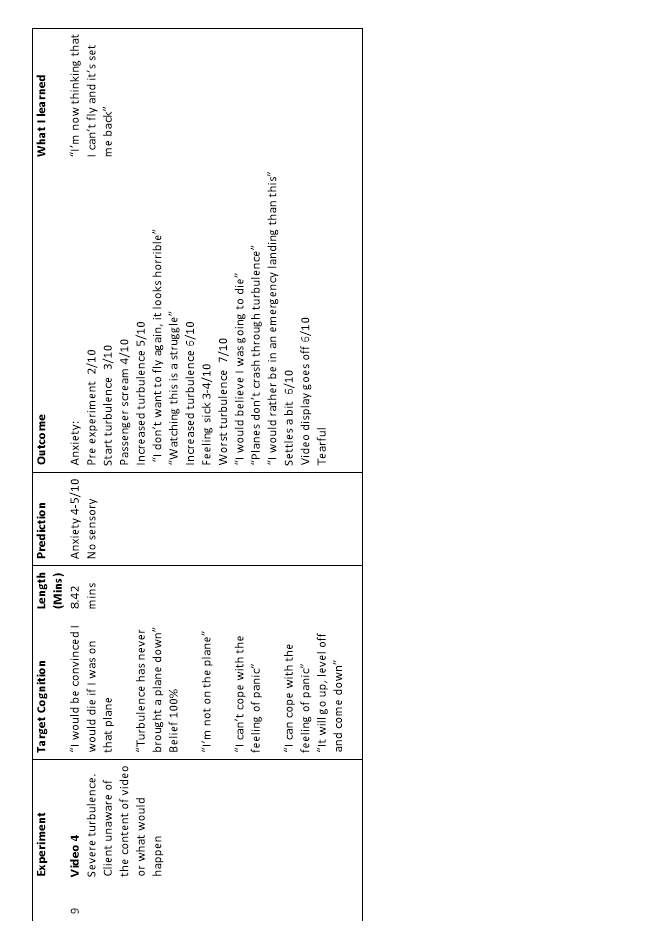
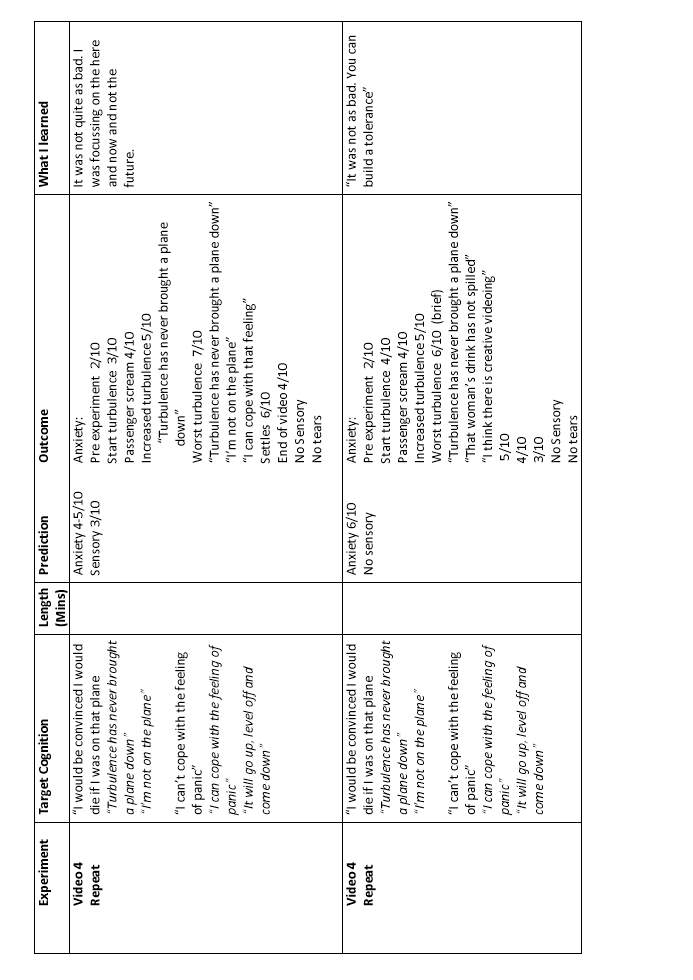
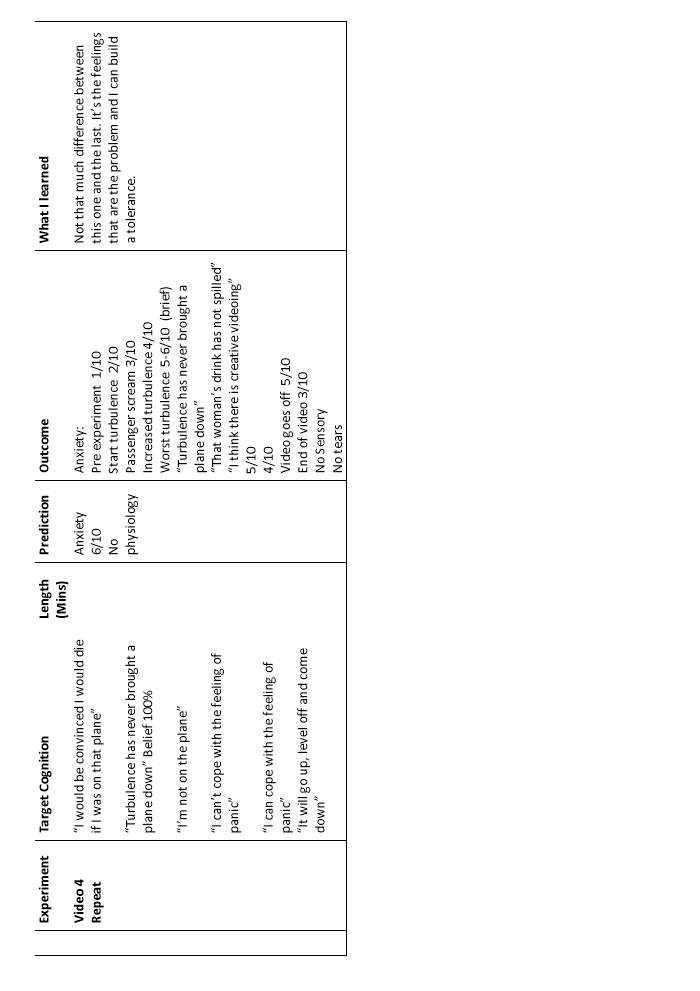
9.13 Behaviour experiment, unknown flight video
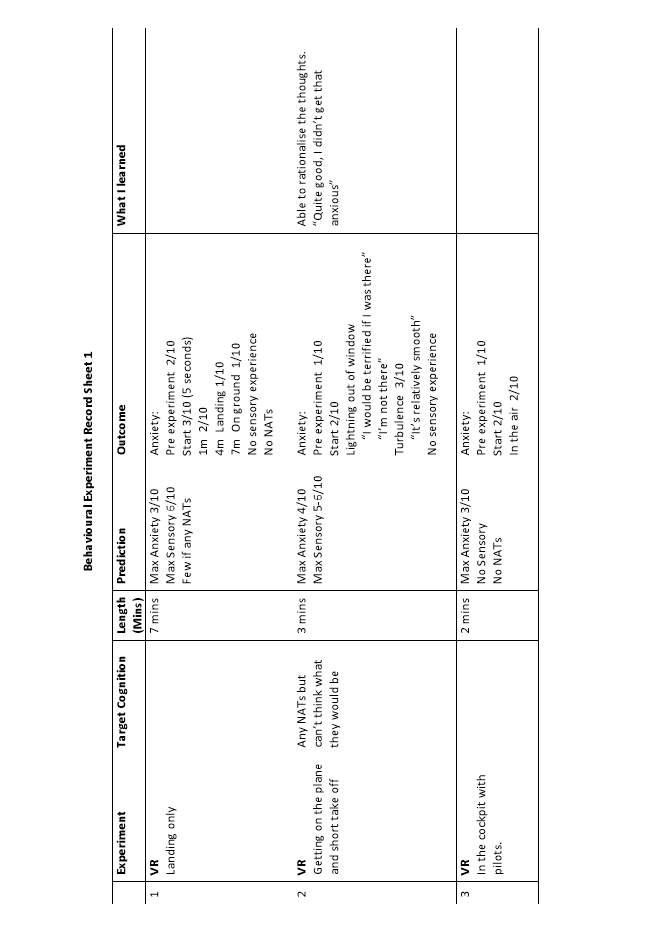
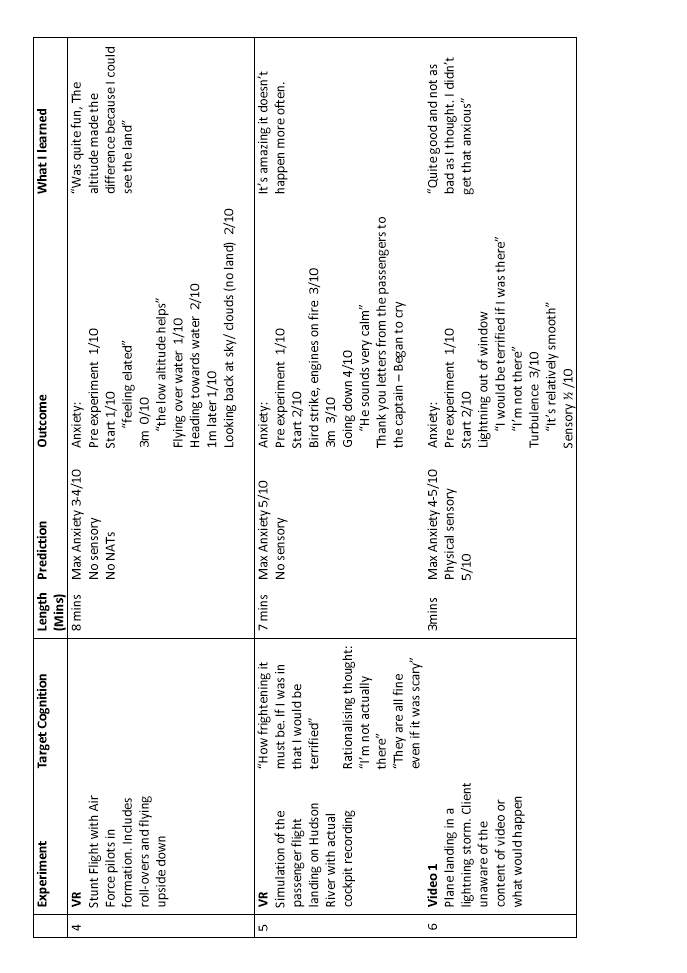
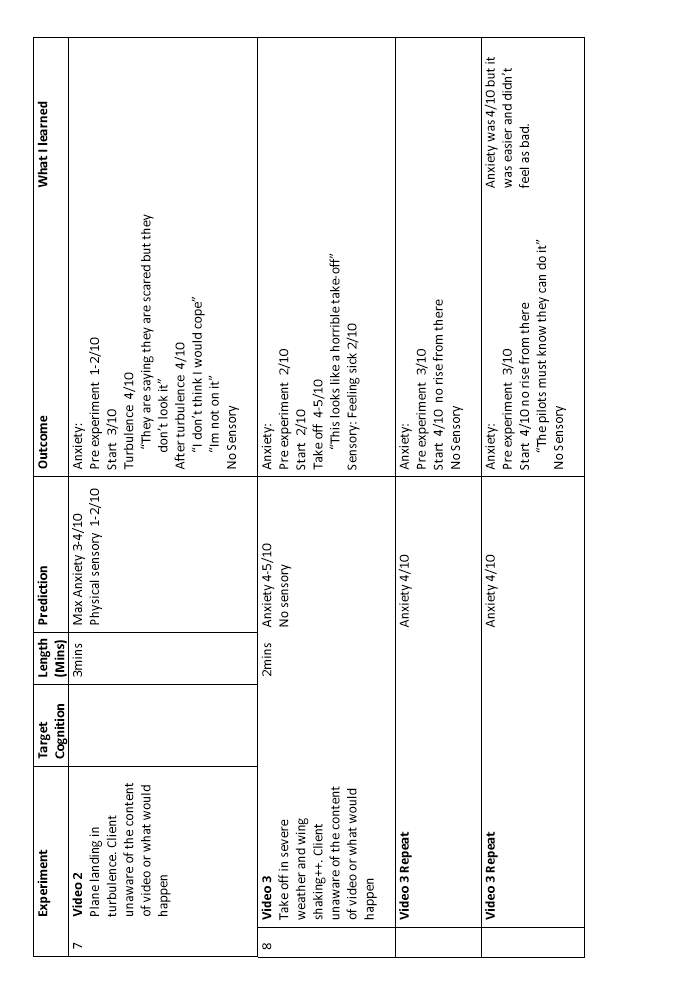
9.14 VR Behaviour experiments
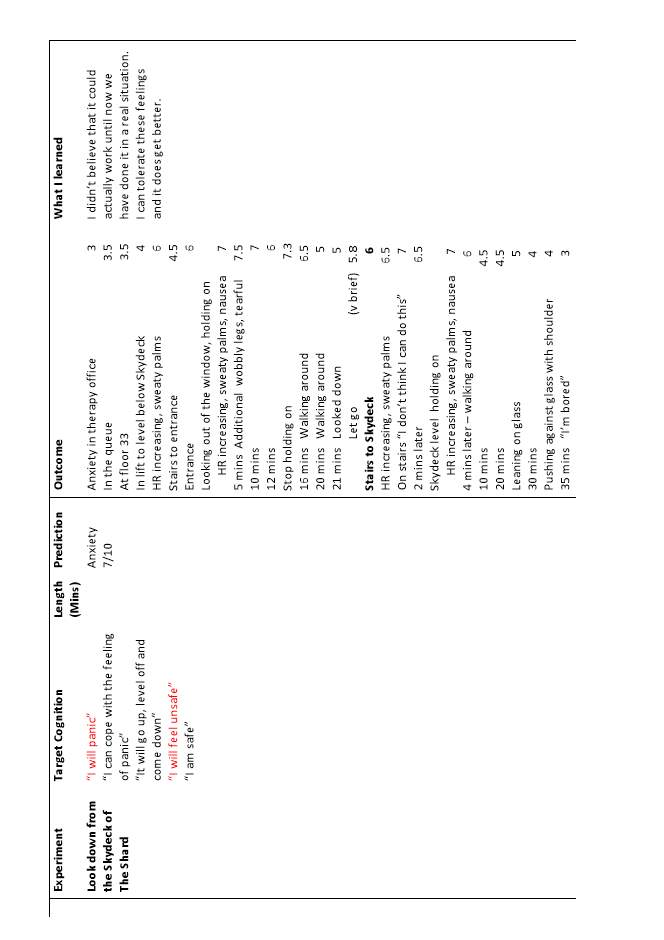
9.15 Behaviour experiment, The Shard
9.16 Behaviour experiment, flight to Edinburgh
10. References
1. Introduction
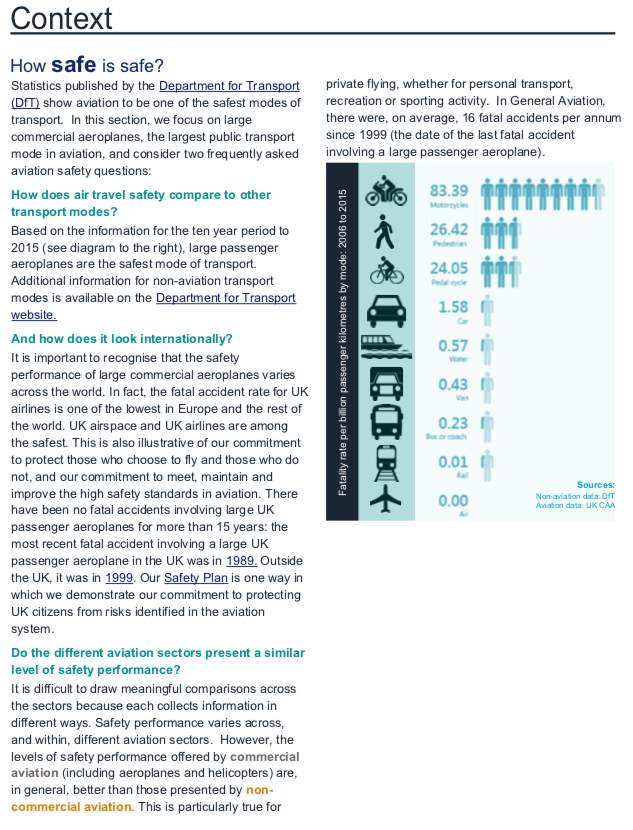
Within the DSM-V diagnostic criteria, Specific Phobia (SP) is a ‘marked fear or anxiety about a specific object or situation’, with fear of flying (FF) and acrophobia specified under the ‘situational’ subcategory and fear of death (FD) within ‘other’. The stimuli create immediate fear or anxiety and will be avoided or endured with intense anxiety (American Psychiatric Association, 2013) (Appendix 9.1). Kessler, Petukhova, Sampson, Zaslavsky & Wittchen, (2012) estimate the prevalence of SP in the United States as 7-9%, with 75.8% of those presenting with more than one phobia (Curtis, Magee, Eaton, Wittchen & Kessler,1998). FF in Northern and Western Europe and North America is estimated at 2.5% of the adult population. Although FF is relatively common, the Civil Aviation Authority, (2013) report the global fatal accident rate from 2002 to 2011 was 0.4 per million hours flown, and decreasing. Beck, Emery and Greenberg, (1985), suggest ‘that if a person could only die as the result of the plane crash, he would live to be a million years old’. SP affects twice as many women as men. (Barlow, Allen and Basden, 2007). Curtis et. al., (1998) report people with SP have parents, especially mothers, with history of mental disorders.
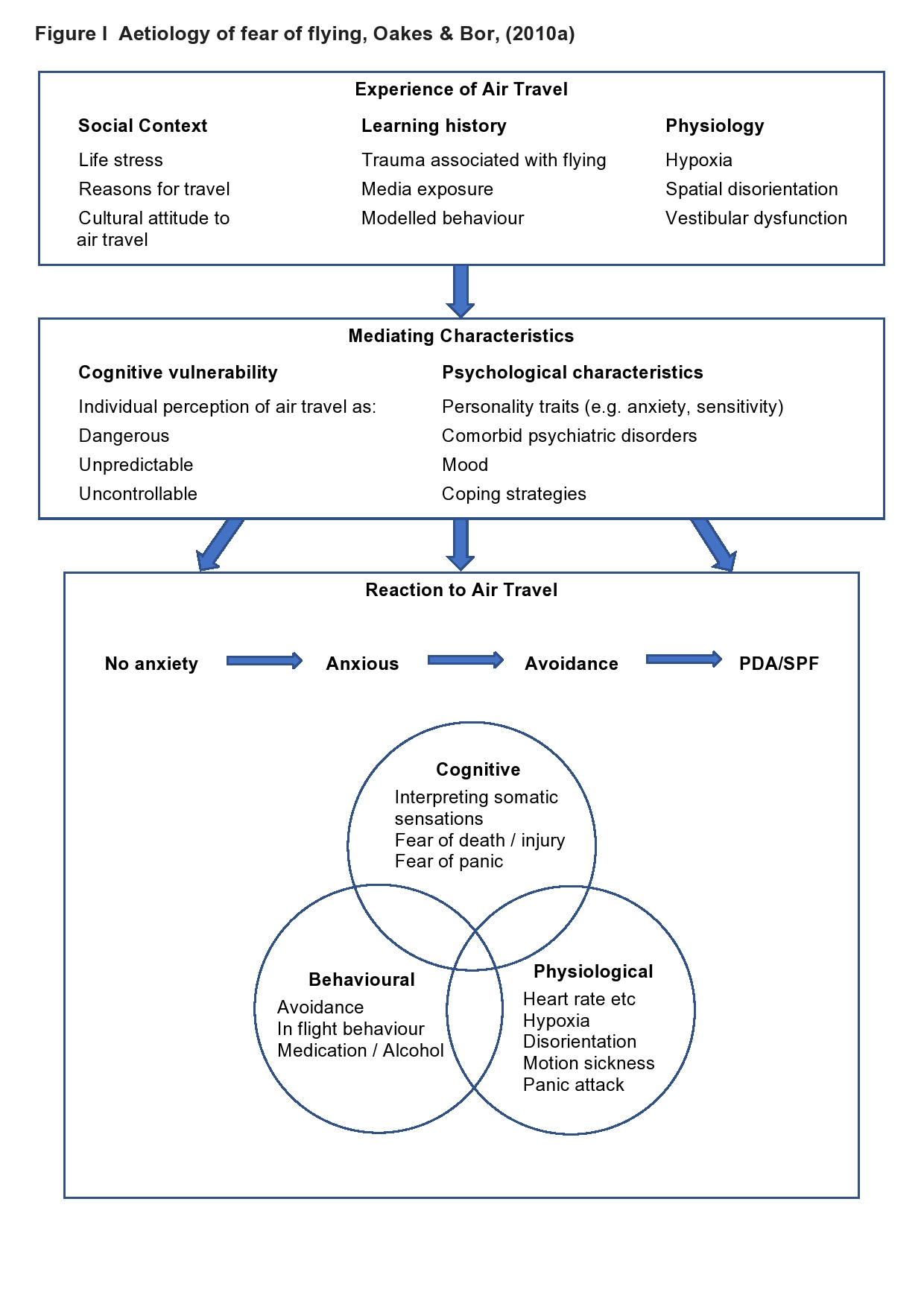
Rachman, (1977) suggests that fear can be acquired by three pathways: conditioning, vicarious exposures and information and instruction. Oakes and Bor, (2010a) evaluated ten studies examining the aetiology of FF. They found FF is acquired by ‘complex psychological, social and physiological factors unique to each affected individual’ (Figure I). They found limited evidence to support vicarious exposure.
In SP, fear is out of proportion to the perceived threat creating symptoms of anxiety or panic (sweating, shaking, increased heart rate (HR) and hyperventilation), even though the person may recognise their reaction is irrational (Beck et. al.,1985). When fear is activated, seeking avoidance or escape provides temporary relief, but with no disconfirmation of the threat, maintains the problem (Barlow, 2004; Clark & Beck, 2010; Salkovskis & Clark & Gelder, 1996).
Ekeberg, Seeberg and Elleertsen, (1989) describe three subgroups of people with FF.
Those who:
- do not fly at all
- restrict flying to a minimum experiencing intense anxiety
- continue to fly with continuous mild/moderate anxiety.
FF can be divided into two subcategories: loss of internal control and loss of external control. Only a few will fear both. Fear of losing internal control relates to social anxiety, panic disorder, claustrophobia and agoraphobia. The stimuli in fear of loss of external control include mechanical failure, pilot error, bad weather or turbulence causing a crash. This is related to flying phobia, fear of heights and death (McNally & Louro, 1992 & Wilhelm & Roth, 1997). Safety behaviours include sitting near emergency exits or seeking reassurance by questioning cabin crew about delays or weather (Oakes, & Bor, 2010a). Avoidance strategies include numbing anxiety with alcohol and medication (Barlow, 2004).
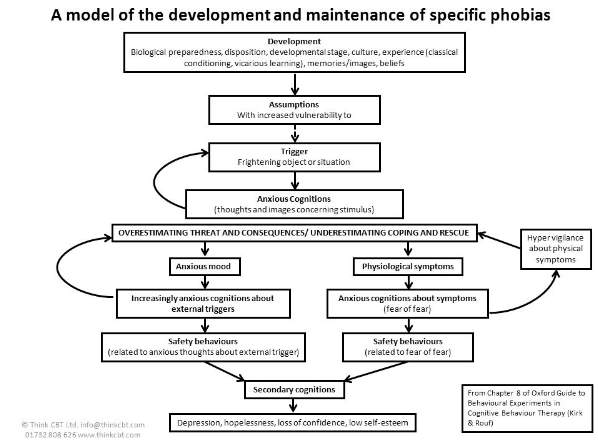
Substantial evidence supports the use of cognitive behavioural therapy (CBT) in treating anxiety disorders. In the Butler, Chapman, Forman and Beck, (2006) review of meta-analyses, large effect sizes were found for CBT in panic and anxiety disorders. CBT showed superior mental state improvements over all other treatments up to 18 months post treatment (Epp and Dobson, 2010). In SP, exposure to stimuli improves tolerance and weakens associations. Cognitive approaches test negative assumptions and beliefs to allow more realistic appraisals (Craske & Rowe 1997). Oakes and Bor, (2010b), conducted a critical evaluation to identify best practice for FF. They noted that interventions lacked comprehensive assessment, and treatments were not embedded within a consistent CBT framework. The closest model for FF is Kirk and Rouf (2004) SP model, identifying two maintaining cycles of ‘overestimating threat and consequences’ and ‘underestimating coping and rescue’ (Appendix 9.2).
Besides the SP model, Virtual Reality Exposure Therapy (VRET), a developing technology requiring further investigation, looks promising (Botella, Osma, Garcia‐Palacios, Quero, & Baños, 2004; Cardoş, David, & David, 2017; and Freeman, et. al., 2017 consider VRET superior in treating FF but poor quality of research results from the term ’VR’ being misapplied to non-interactive, non-immersive technologies. The Oculus Rift HMD VR system for research and clinical applications is a powerful tool giving an immersive and realistic experience causing vertigo in height phobics (Chessa, Maiello, Borsari & Bex, 2016).
1.1 Biographic data
Lucy, 33, is a happily married, self-employed psychotherapist with no children.
2. Presenting problems
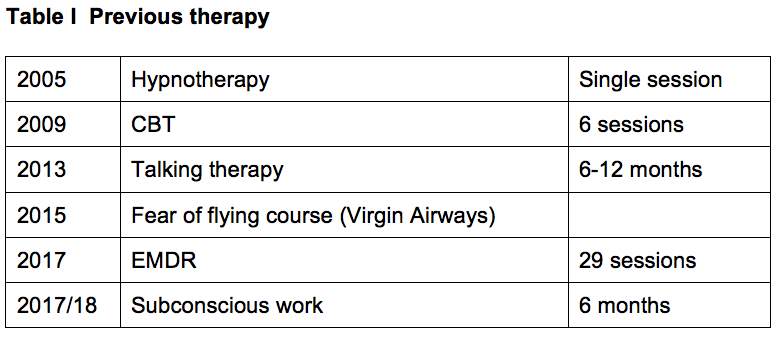
Lucy self-referred with a thirteen year history of persistent FF, and a twenty six year history of acrophobia. She was unsure why she had developed a FF, having no recollection of experiencing a difficult flight, previously considering flying “boring”. Having unsuccessfully undertaken several therapies her fear had increased (Table I).
Lucy reported little anxiety in other areas of her life, although during therapy a FD emerged. Lucy had avoided for a year and described her fear as “sheer terror”. She was becoming increasingly fearful of friends or family flying, thinking “the plane will come crashing out of the sky” and “inevitable death”. “Loving travel” she “would do anything” to overcome her fear and expressed little hope that anything could help her and fearing further disappointment.
2.1 Coping strategies
Lucy’s coping strategies included safety seeking behaviours of avoidance and reassurance seeking. She had used sedatives, alcohol and distraction like films and books to try to numb her panic and block distressing thoughts and images. Hypervigilant to signs of danger, she sought reassurance by concentrating on captain’s announcements, questioning flight attendants, gauging their mood and attentiveness. If the crew or captain were not as friendly or attentive enough, her anxiety and need to seek reassurance increased. Lucy avoided all reminders of flying, even photographs which would trigger anxiety. She also avoided tall buildings where possible or stayed away from windows or closed her eyes.
2.2 Treatment goal
Goal:
Tolerate anxiety, manage negative automatic thoughts (NATs) enough for a flight without alcohol, sedatives or reassurance.
Anxiety 10/10 Target 5/10
2.3 Diagnostic criteria
Lucy met the DSM-V diagnostic criteria for SP for FF, acrophobia and FD. Panic Disorder was discounted as she had no catastrophic misinterpretation of physiological symptoms of panic (American Psychiatric Association, 2013).
2.4 Standardised measures
Standardised measures for FF are few. The Fear of Flying Scale (FFS), developed by Haug, et. al., (1987), rated anxiety in twenty one flight related situations. Van Gerwen, Spinhoven, Van Dyck, and Diekstra, (1999), developed the Flight Anxiety Situations Questionnaire (FAS), and the Flight Anxiety Modality Questionnaire (FAM), (Appendix 9.3 & 9.4). Used together they examine two aspects of a FF. The FAS assesses anxiety stimuli in three flying situations: planning the trip, boarding and the actual flight. The FAM assesses anxiety related to thoughts of danger and physiological sensations. A copy of the FFS was unavailable so the FAS/FAM was selected for Lucy. The Visual Height Intolerance Severity Scale (vHISS) developed by Huppert, Grill and Brandt, (2017), (Appendix 9.5) was used to assess the severity of visual height intolerance (vHI) and whether she would meet the DSM-V diagnostic criteria for acrophobia within SP. The revised Death Depression Scale (DDS), (Appendix 9.6) was completed to assess her FD. The DDS measures four factors: ‘death sadness’, ‘anergia’, ‘existential vacuum’ and ‘anhedonia’, (Templer, Lavoie, Chalgujian, and Thomas‐Dobson, (1990). The scale does not identify general depression as death depression is more closely linked to general anxiety (Templer, et. al., 1990). Although Lucy reported not experiencing general anxiety, the General Anxiety Disorder 7 (GAD-7), (Appendix 9.7) was completed as confirmation (Table II).
2.5 Suitability
No specific SP treatments are included by National Institute for Health and Care Excellence (NICE). It recommends 7-14 hours of CBT, in 1-2 hour sessions, within 4 months for PD. Lucy had undertaken CBT previously and as a therapist understood therapeutic processes. Her motivation for change was overshadowed by doubt that her fear could reduce. She had never experienced suicidal ideation, so CBT was considered appropriate.
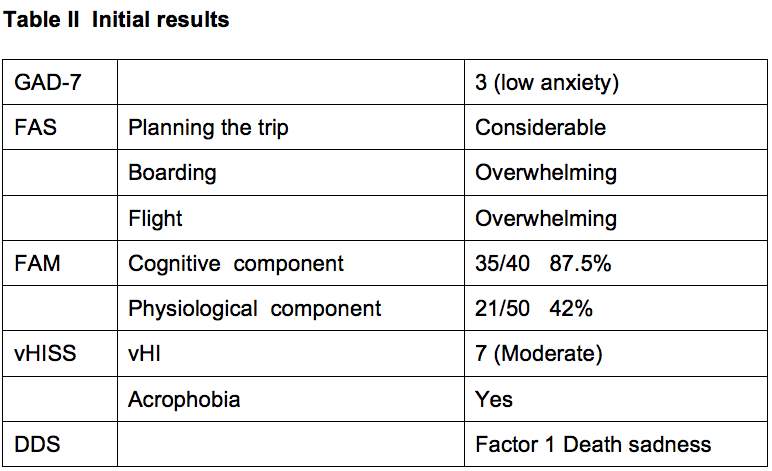
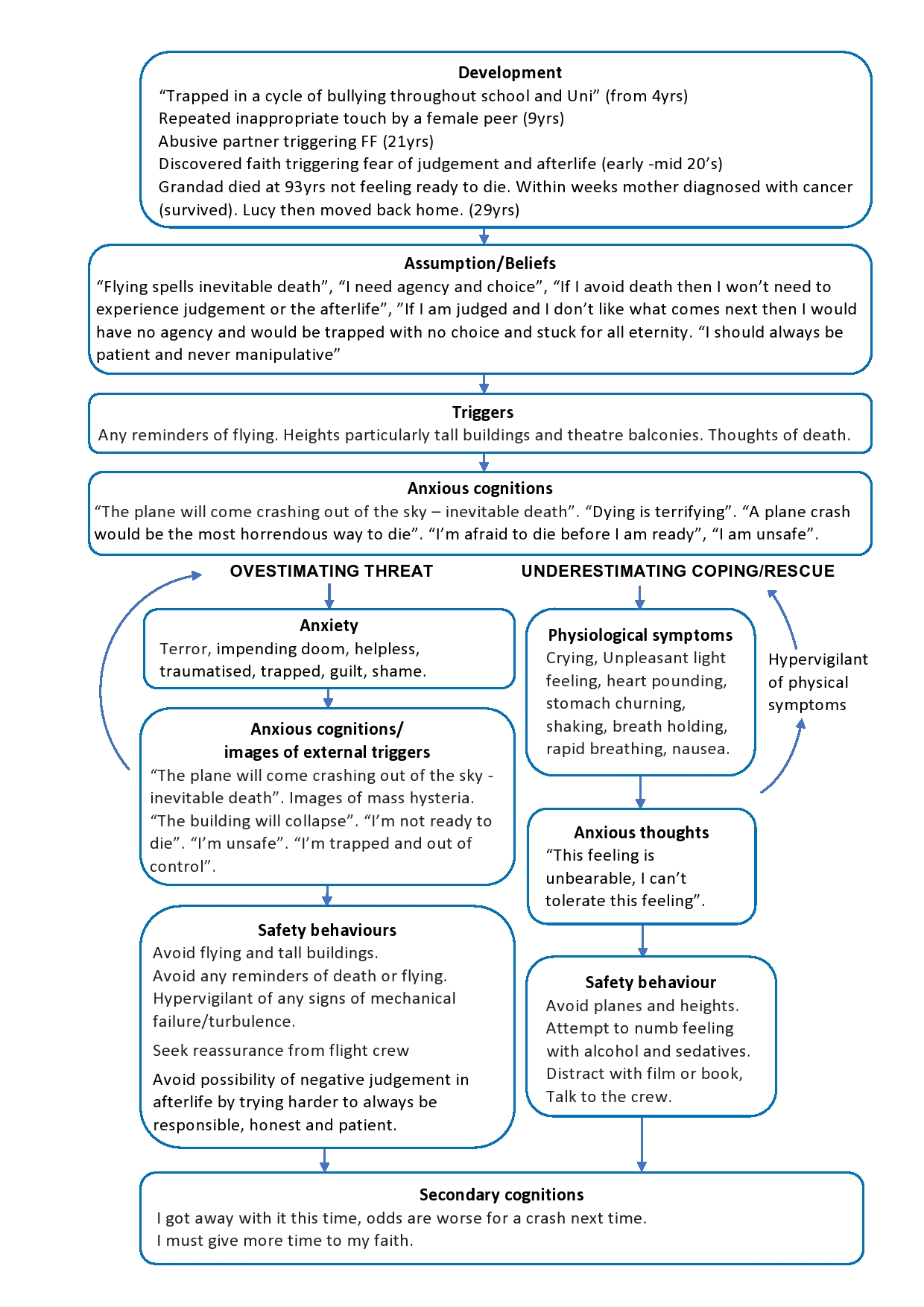
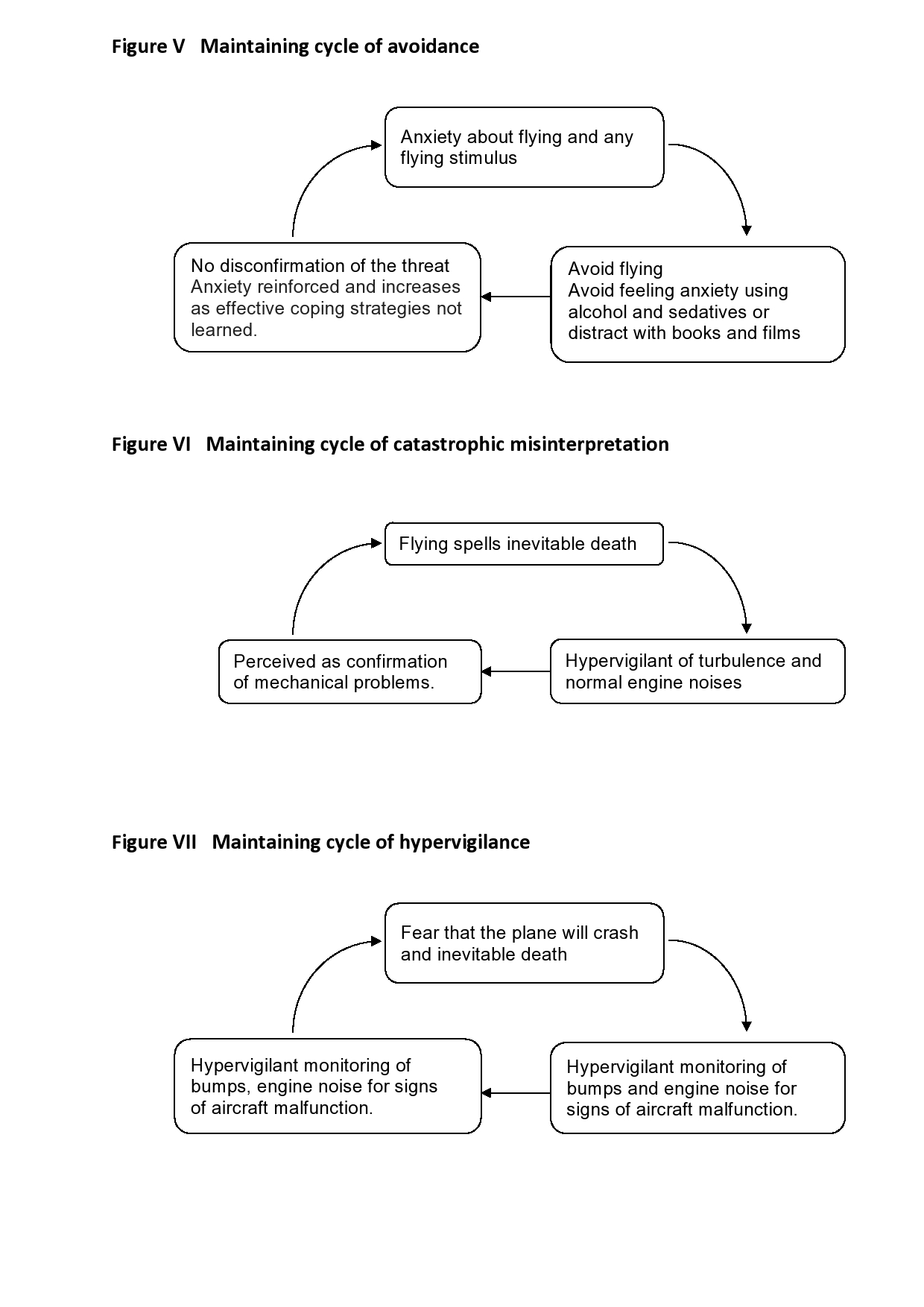
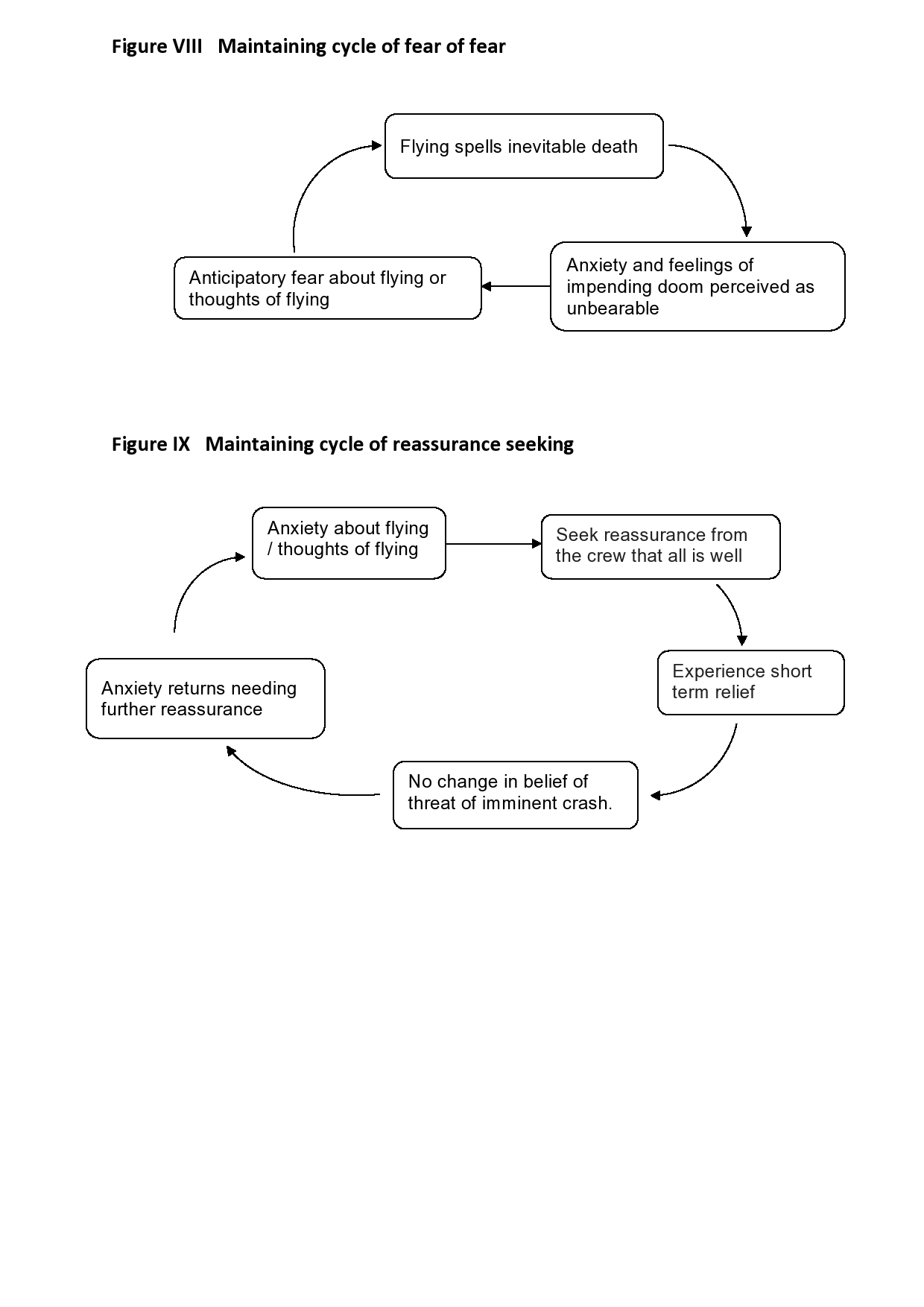
3. Case conceptualisation
Lucy had a FF, acrophobia and FD. Her FF, formulated using Padesky’s (1990) ‘hot cross bun’ (Figure II) identified maintaining cycles of avoidance, hypervigilance, catastrophic misinterpretation, fear of fear and reassurance seeking (Figures V-IX). Lucy had negative thoughts and images, and a ‘hot thought’ of “the plane will come crashing out of the sky and inevitable death”, triggering feelings of “sheer terror” and physiological symptoms of panic. She was hypervigilant of turbulence, engine noises and wing movements, interpreting these catastrophically. Rather than learning to tolerate panic, she tried to numb it or distract herself, further increasing her belief that her feelings were intolerable, eroding her resilience and increasing anticipatory anxiety (Beck, et. al., 1985). Avoiding flying and any reminders in her daily life reduced her anxiety temporarily. However, without opportunities to disconfirm the perceived threat, her fear increased to include friends and family flying (Salkovskis, Clark & Gelder, 1996). Her coping strategies maintained and exacerbated the problem until she could no longer fly. Lucy applied similar strategies to her acrophobia and FD by avoiding tall buildings and thoughts related to death. As thirteen years of different therapies were unsuccessful, we explored possible links with past experiences. Through comprehensive assessment as suggested by Oakes and Bor, (2010b) and formulating using a vicious flower (Figure III) Lucy connected “feeling trapped” and “lack of agency”. We formulated this using the Kirk and Rouf, (2004) SP model and she recognised how her difficulties were maintained. I hypothesised that with greater understanding and realistic appraisals, exposure may prove more effective.
3.1 Vulnerability and precipitating factors
Lucy, an only child, has a close, loving relationship with her parents. Her mother also suffers a FF and shared details of eventful flights, exacerbating Lucy’s FF and FD.
Lucy described being “trapped in a cycle of bullying throughout school” and University. At age nine she suffered repeated, unwanted, inappropriate sexual touch at home by an older female child. At twenty one, Lucy was in an abusive relationship. Her anxiety about him joining her family holiday abroad precipitated the FF. This correlates with life stressors as a cause of FF (Oakes & Bor, 2010a). Lucy’s fear of death, judgement and the afterlife came with her discovery of faith in her early twenties, exacerbated by her grandfather’s death at ninety three “he didn’t want to die and didn’t feel ready”, and her mother’s diagnosis of cancer in 2014 (now recovered).
3.2 Formulations
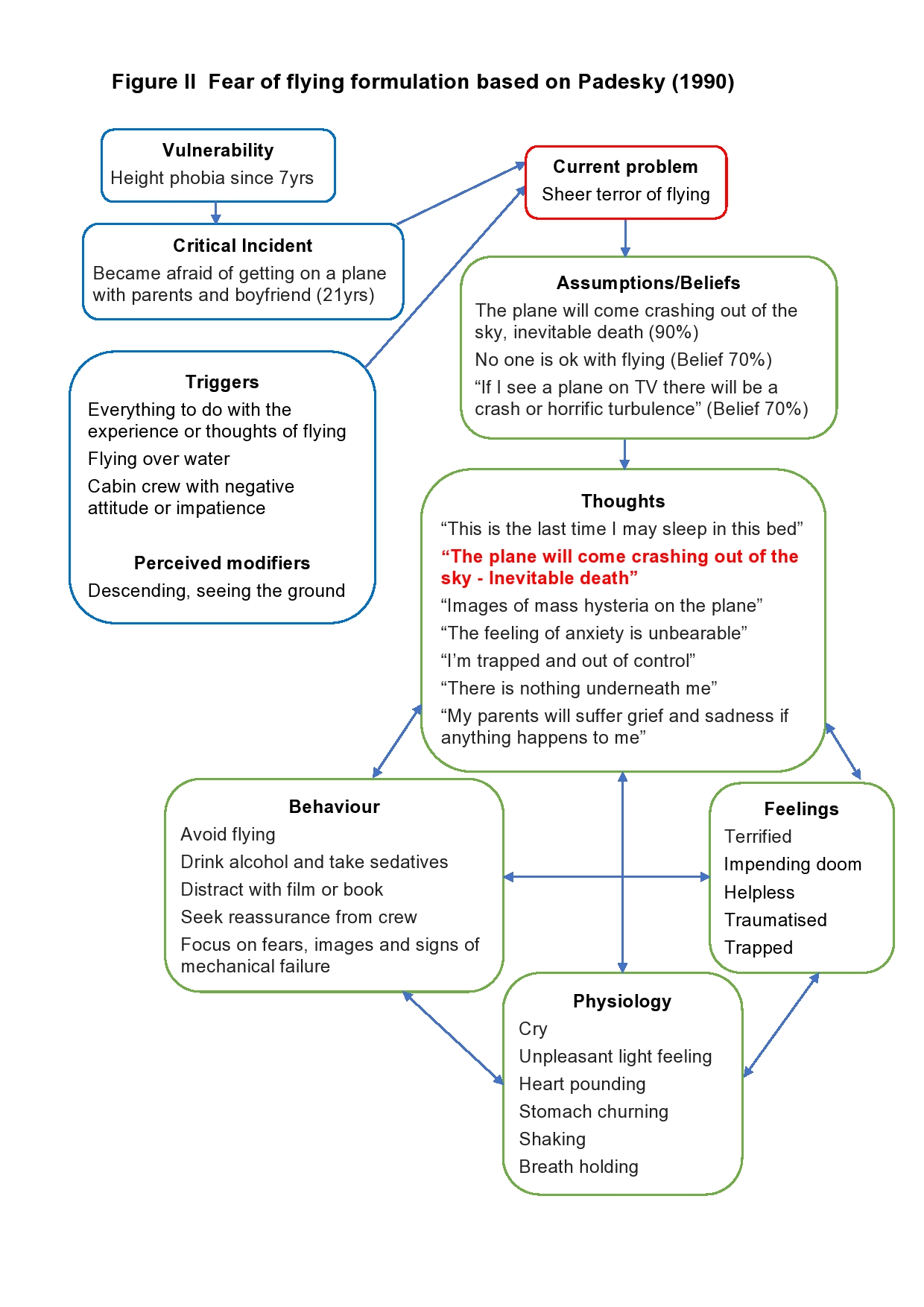
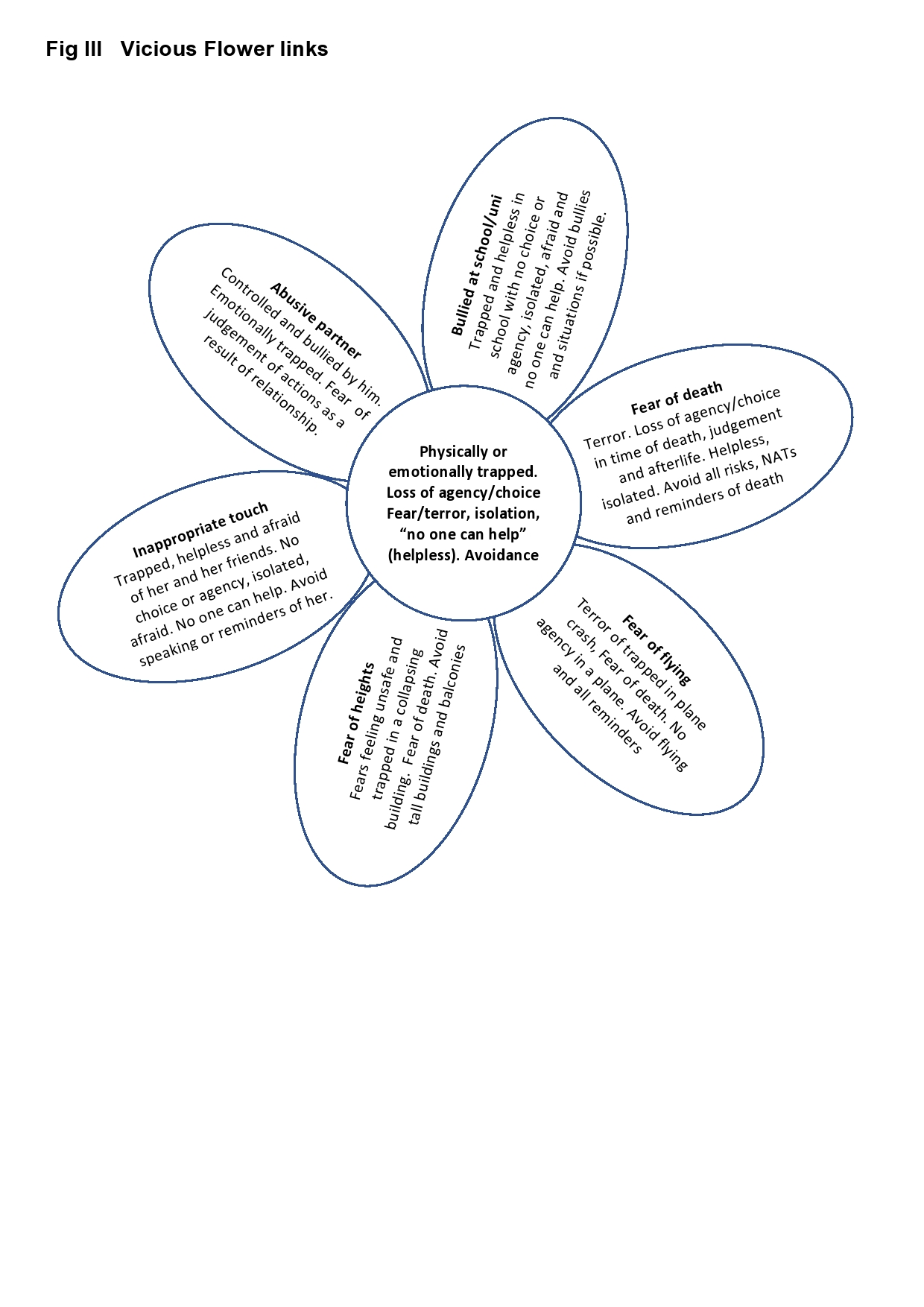
Figure IV Formulation based on Kirk and Rouf, (2004) model of SP
4. Treatment Plan
- Assessment of difficulties
- Statistical information about the safety of passenger airlines
- Psychoeducation of cognitive processes
- Identification and testing of negative beliefs/assumptions and development of rationalising thoughts
- Exposure through graded behaviour experiments with video, VR and an actual flight
- Relapse management throughout
- Blueprint
5. Course of therapy
Over five months, Lucy has received 10 x one hour sessions and 3 x extended sessions: VR, The Shard and a Luton to Edinburgh flight.
5.1 Assessment session
We explored Lucy’s difficulties using a Socratic style and a positive therapeutic alliance quickly developed. Lucy commented that unlike other therapists, as I made no guarantees of success or progress, she felt she could trust me. Lucy cried describing her FF including a panic attack in flight, triggering an argument with her husband. She described the unpleasant light feeling which she also experiences with heights. We agreed an agenda, completed and discussed the FAS, FAM and GAD-7 and developed a formulation of her FF (Figure II).
Homework: complete a thought record of NATs to evaluate the proportion of flying NATs compared to other life NATs.
5.2 Session one
Lucy found the assessment helpful, recognising that extreme anxiety is reasonable if flying meant 90% certainty of death. Lucy recorded no NATs on the thought record suggesting that her anxiety was phobia specific and she was proficient at avoiding flying stimulus.
Lucy’s ultimate goal was flying again so we developed an initial SMART goal:
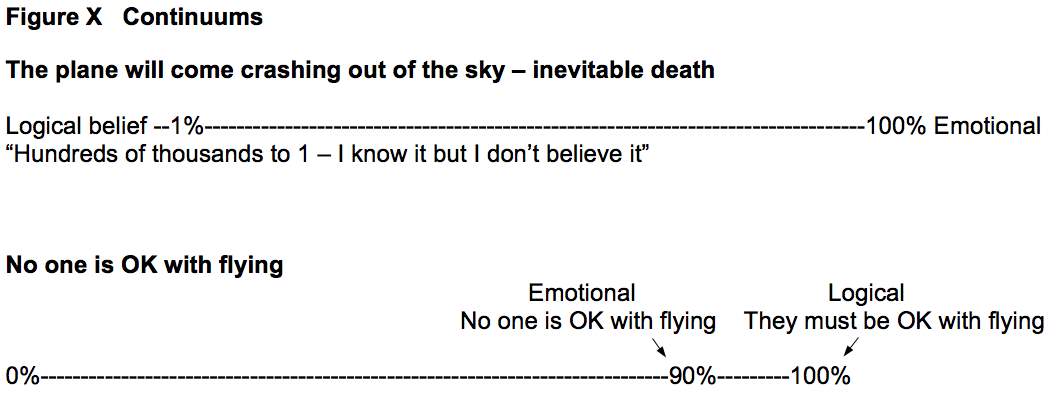
‘tolerate anxiety enough to watch an airline advertisement’. A continuum helped Lucy separate her logical belief from emotional fear (Figure X). She found this extremely difficult, but slightly easier when using the third person.
Homework: A thought record of NATs about an airline advertisement. Record anxiety and rationalising thoughts.
5.3 Session two
Lucy completed the thought record (Appendix 9.8) identifying a hot thought of “it will crash”. She rationalised “I am at home safe” and recognised no evidence supporting the NAT. She described her vivid imagery of pictures and smells, thinking them “utterly fixed and too powerful” and previous imagery and exposure work had made them worse. Lucy, struggling to understand the difference between her logical belief and emotional fear seemed stuck, so I considered why previous therapies been unsuccessful, for example, client engagement, therapist skills or an previously undetected issue. A downward arrowing technique revealed a FD with assumptions and beliefs (Transcription, Appendix 9.9). Lucy completed the DDS identifying ‘death sadness’. She cried describing her sadness about death. She experienced daily NATs about her own or parents death. We explored her assumption, “if I avoid death then I won’t need to experience judgement or the afterlife”.
Hypothesis A: I won’t like what comes next and it is infinite
Hypothesis B: What comes next is better and there is no fear or pain
I asked why she would believe A over B, she said, “I can’t imagine B so I can’t identify with it”.
Homework: A thought diary of NATs about dying including her emotions.
5.4 Sessions three and four
I sought supervision which guided me to explore more about the links to her past, completed in two sessions. Lucy had not completed the thought record for fear of “making myself miserable” but recognised this as avoidance. There had been little effective support from parents or school staff to address the bullying or inappropriate touching, parents stating they “felt sorry for the tutor because he was trying to help”. Links in the meanings of her thoughts, emotions and behaviour were formulated using a vicious flower (Figure III). These were: ‘physically/emotionally trapped’, ‘loss of agency/choice’, fear/terror, isolation, helplessness and avoidance. Lucy realised that feeling “trapped” and “lack of agency” were major anxiety triggers of her phobias.
Homework: As this was an intense process, Lucy’s homework was to reflect on these links and what they meant to her.
5.5 Session five
Between sessions, Lucy recognised “lack of agency” included conforming to routines historically at school and currently within work, where she maintained full agency within self-employment. She understood how her anxiety was maintained through a shared development of the Kirk and Rouf, (2004) SP model. She said, “I still can’t understand how it can help me though as I don’t believe I can ever stop believing that I will die on a plane so will always be terrified”.
Fear overwhelmed her so quickly, she had extreme difficulty focussing on her logical, rational beliefs. Familiarity with the concept of fight/flight/freeze never helped so I explained the process of stress activating fight/flight and as stress increases the ability to process rationally decreases (Kircher, et. al., 2013). Understanding the need to experience fear with exposure whilst maintaining logical processing of her rationalising thoughts, and concluding that her fear was, in principle, tolerable rather than indicating danger, gave her a flicker of hope for the first time (Craske & Rowe 1997). Airline safety information given (Appendix 9.10)
Homework: consider a suitable behaviour experiment.
5.6 Sessions six, seven and eight
Over three sessions, three behaviour experiments were conducted (Table III).
Table III Behaviour experiments
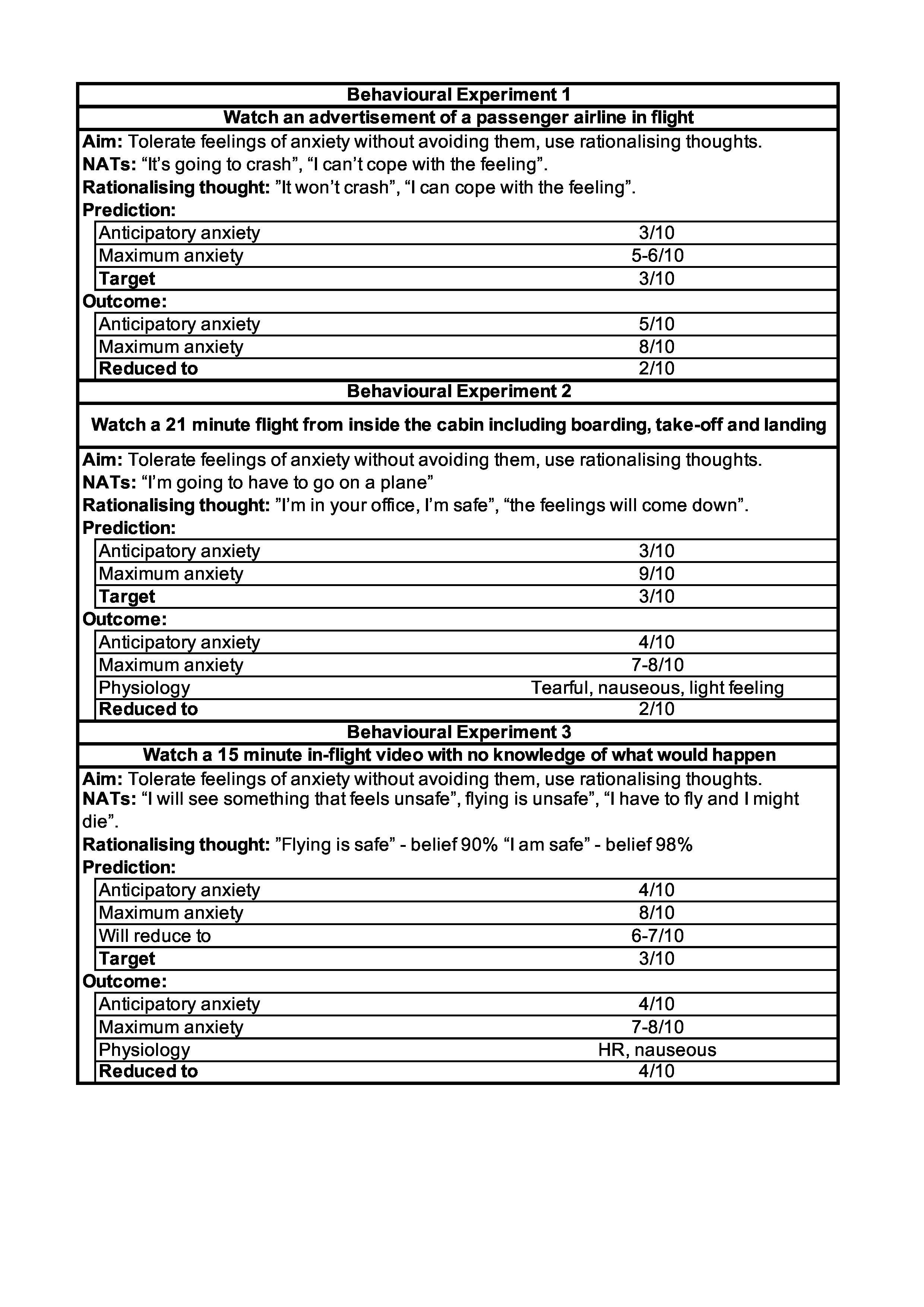
Behavioural experiment 1 (Appendix 9.11)
Over 45 mins, Lucy watched the advertisement. Initially she had numerous NATs and projected worries about “never being able to get on a plane”, “plane looked evil” and “the more people on the plane, the more would mourn”. Her body was curled up and rigid, her voice strained and her breathing quickened. I asked her to focus on her rationalising thoughts and her anxiety gradually decreased with only a brief spike when flying over the sea. At thirty minutes I remained quiet and at forty five minutes her anxiety was 2%. Lucy reflected, “exposure can work if there is also a strategy”, “I have never spent that long looking at a plane and my anxiety reduce”, “I understand how it works now”, “I still don’t think I will ever get on a plane”.
Behavioural experiment 2 (Appendix 9.12)
Lucy’s anticipatory anxiety pre take-off was higher than during the flight and she became nauseous, tearful, anxious with the ‘light feeling’ but this quickly settled. NATs were considerably less than the previous video and anxiety gradually decreased.
Homework: Watch videos at home using the same techniques and record anxiety.
Lucy watched the video at home just once as she experienced nausea, however, her anxiety remained low (4). After discussion she felt under confident to view videos without me. This needed to be addressed in future sessions to reduce dependence.
Behavioural experiment 3 (Appendix 9.13),
After one minute Lucy felt nauseous. Her HR increased when turbulence was announced, but said she “felt OK”. She experienced disturbing thoughts and images of her mother’s account of fear on a difficult flight. Lucy was able to rationalise “they were never going to crash into the sea”. At the end she rated excitement 4 rather than anxiety. We used imagery of Lucy reassuring her mother on the plane and both feeling calm to reduce her anxiety (Greenberger & Padesky, 2015).
Homework: Practice the imagery.
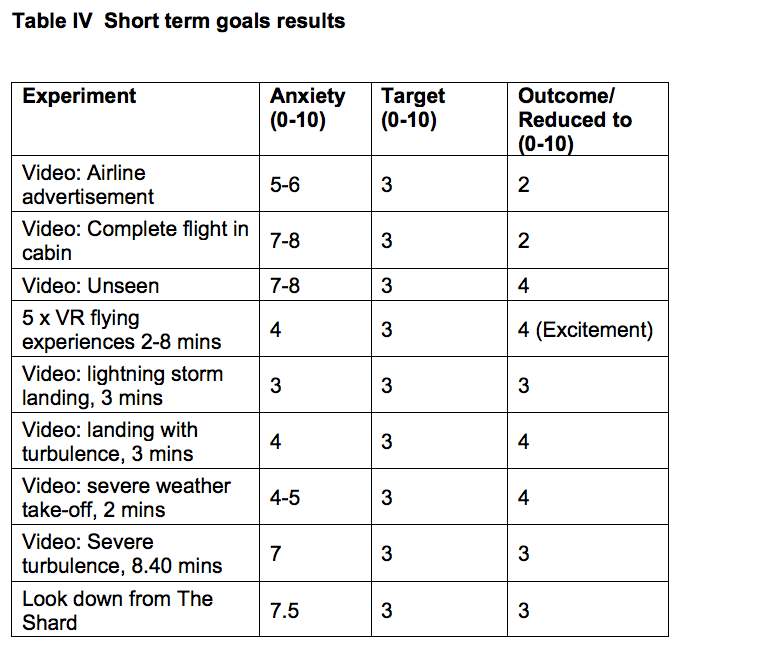
5.7 Session nine VR
By the next session Lucy had successfully replaced her negative images. Five fully immersive, 360° flight videos of between 2-8 minutes were selected from YouTube to run on an Oculus Rift HMD system. These included: landing, boarding, short take off, in the cockpit with pilots, a formation flight with Air Force pilots including roll-overs, flying upside down and a simulation of the passenger airline landing on the Hudson River with actual cockpit recordings. The session time was not limited. We agreed an agenda including: viewing VR non-flight content enabling adjustment to the experience, order of flight videos and preparation for each experiment. Anxiety would be rated out of ten.
Lucy enjoyed non-flight VR, experiencing awe and excitement but no anxiety even when on top of a high building. She had a high tolerance of the VR flight videos and her anxiety remained low throughout (Appendix 9.14). As the Hudson River aircraft went down she commented, “the pilot sounds very calm”. Lucy had imagined “mass hysteria” in an emergency rather than a calm captain in control and passengers reported quiet in their own thoughts. We had not anticipated that she would view VR as exciting and fun, likening it to “simulators”. We therefore considered she had little opportunity to learn tolerance (Clark & Beck, 2010). Lucy felt confident so after a break, four challenging non-VR videos were selected (Appendix 9.15):
- Plane landing in a lightning storm (3 mins)
- Plane landing in turbulence (3 mins)
- Take off in severe weather with significant wing shaking (2 mins)
- Severe turbulence (8.5 mins)
Videos 1-3 ran smoothly but video 4 was challenging with anxiety 7/10 (A7). She was nauseous and tearful, commenting, “I don’t want to fly again it looks horrible” and “I would believe I was going to die”. She struggled to use rationalising thoughts but after two more viewings her anxiety increased briefly (A6) without nausea or tears. She reflected “You can build up a tolerance”.
Homework: Watch some of the earlier videos.
5.8 Sessions ten and eleven
Lucy watched earlier videos without difficulty, but had lost confidence after ruminating over video four believing loss of all progress. Her perceived setback led to dichotomous thinking of failure. As a relapse management strategy she re-watched it in session, surprised to discover her anxiety remained low and she became bored (Marlatt & Donovan, 2005). We reflected how far she had come and reviewed the formulation. She still felt too afraid to fly so she suggested going up The Shard the following week. She said, “it’s nearly as bad as on a plane but I can tolerate it”.
Behavioural experiment The Shard (Appendix 9.16)
Look down from the Skydeck of the Shard and tolerate feelings of anxiety.
Lucy’s anxiety rose (A6) with increasing heart rate (HR) and sweating palms as we reached the level below Skydeck. She froze at the entrance but with gentle prompting approached the window holding on (A7). After five minutes she experienced wobbly legs, nausea, and became tearful (A7.5). I resisted reassuring her, gently prompting her to remember rationalising thoughts. After sixteen minutes she could walk around (A6.5) and twenty one minutes could look down (A5). She felt ready to attempt the Skydeck and as she predicted her anxiety increased. While ascending she froze, stating “I don’t think I can do this”. We discussed progress so far, predicting if we stayed still the anxiety would fall. This occurred and Lucy made it to the Skydeck. After seventy five minutes she walked around confidently, moved quickly to a window, looked down, leant against the glass and finally pushed hard against it with her shoulder. When her anxiety had fallen to three, we left. Lucy reflected “I didn’t believe it could actually work until now, in a real situation. I can tolerate the feelings and it does get better”.
5.9 Sessions twelve and thirteen - Edinburgh flight
We planned a flight and Lucy booked it (Appendix 9.16). I suggested a minimum flight time of 1.5 hours but it was only 55 minutes. Lucy practiced learned techniques to reduce her anticipatory anxiety in the preceding days. Her anxiety (A5) and unsafe feelings (U6) increased driving to and arriving at the airport, decreasing after two hours in the departure lounge (A4, U2). As predicted, they increased while boarding and awaiting take-off (A9, U9). Lucy began to cry. After ten minutes they decreased (A8, U8). An increase at take-off gradually reduced over thirty minutes (A8, U8) and she visibly relaxed. At thirty five minutes we hit sudden turbulence so violent the cabin crew dropped to the floor and held on. Lucy terrified, panicked believing “I will never see my husband again” (A100/10, U100/10). Unable to use rationalising thoughts, I spoke calmly reinforcing “we are safe” and “planes are designed to deal with turbulence” although my fear was possible injury in the cabin to myself and others. Lucy’s anxiety and unsafe feelings decreased (8.5) before turbulence subsided. Her anxiety decreased seeing the ground and at touch-down was 0, her usual pattern. We discussed that although terrifying, the plane proved to be safe in extreme turbulence. Her scores reflected the process of decreasing anxiety as the literature suggests and our previous experiments demonstrated. However, extreme turbulence and a short flight gave little opportunity for anxiety reduction beyond her normal patterns. Lucy later cried when recalling her fear during turbulence.
6. Outcomes
Goal
To tolerate anxiety and manage NATs enough to take a flight without alcohol, sedatives or reassurance seeking.
Initial anxiety: 10/10 Aim: 5/10 Outcome: Ongoing
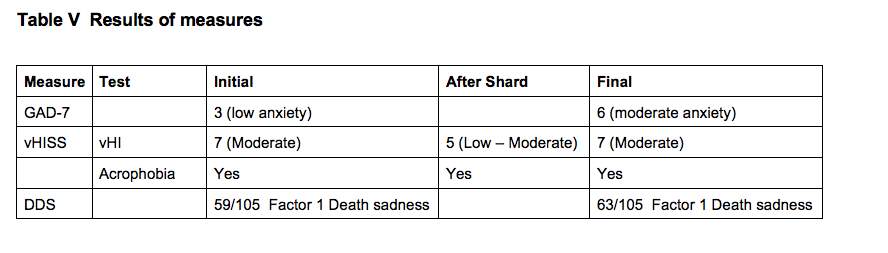
Lucy’s explanation for increased anxiety on GAD-7 was fear of the impending flight and her dissertation deadline (Table V). The vHISS showed reduced anxiety after the Shard but increased again after the flight. Lucy reflected that her acrophobia had not lessened for extreme heights like flying, but she was less afraid visiting tall buildings. “I am not less scared but now know how to bring it down and manage it. I would have less anticipatory anxiety. I would feel high anxiety at the beginning and it would take some time but it would come down. Now I wouldn’t avoid tall buildings.” Lucy acknowledged her increase in death sadness, but considered her death anxiety had reduced.
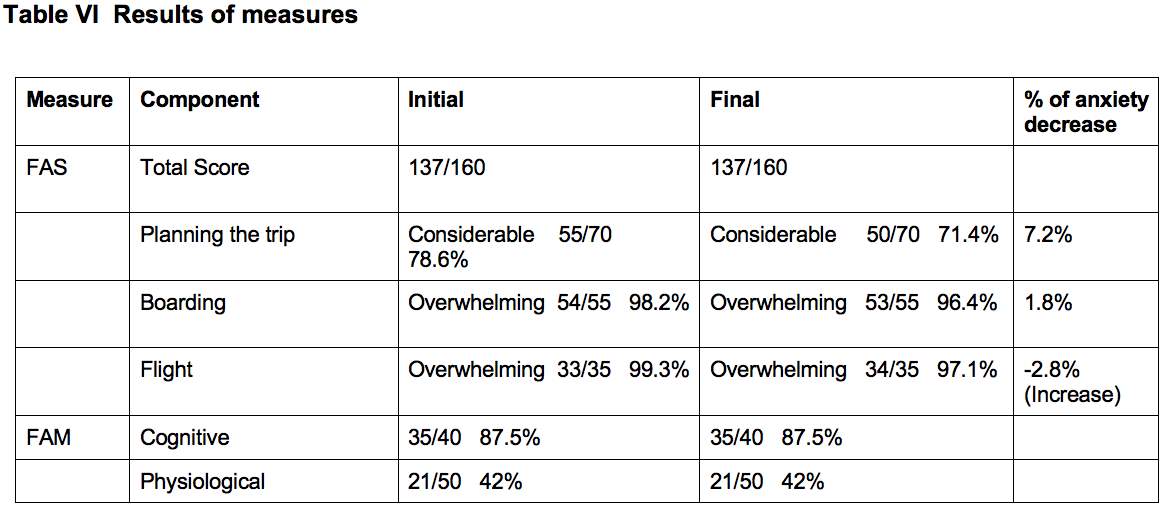
Lucy’s overall scores were identical for FAS and FAM, however, demonstrated reduced anticipatory anxiety in planning and boarding but increased anxiety of the flight (Table VI). This may be unsurprising as her anxiety reduced in the airport lounge but not on the flight.
7. Future Treatment Plan
Another flight is being planned and Lucy would also like to target her FD. Building on her previous learning and based on the study by, Furer and Walker, (2008) the following treatment plan is suggested:
- Assessment and formulation of FD.
- Reflections of previous relevant learning.
- Exposure to FD anxiety triggers
- Reducing identified safety behaviours.
- Testing cognitions
- Increasing attention on lifestyle, enjoyment and goals
- Relapse management throughout
8. Discussion
This fascinating case study has been important for my development, significantly increasing my knowledge and understanding of FF. I felt some responsibility that Lucy considered this her last chance. She was motivated for change but felt hopeless and afraid of disappointment. Throughout therapy, it was important to consider why her previous therapy was unsuccessful. Factors in the literature relevant to Lucy were: as a female with more than one phobia (Barlow, et. al., 2007); a mother with a FF (Curtis et. al., 1998); fear of loss of control over external factors with FF, acrophobia and FD (Borrill & Foreman, 1996); FF acquired by life stress; safety behaviours of seeking reassurance from the cabin crew (Oakes & Bor, 2010a) and alcohol and sedatives to numb anxiety (Barlow, 2004).
It was crucial for Lucy to understand her FF to enable any cognitive shift. Relevant factors included: statistical facts, psychoeducation, developing shared formulations and connecting these to her life experience through a comprehensive assessment (Oakes and Bor, 2010b). My supervision was paramount in undertaking the comprehensive assessment and will be implemented at the beginning of therapy with future FF clients. As Lucy had little understanding of her FF at the outset, it is unsurprising that previous interventions were unsuccessful.
Lucy did not respond to VR as the literature predicted, finding the experience exciting. She demonstrated low fear to potentially frightening VR stimuli raising questions of why, and whether different generations respond differently to VR (for example, perceived as games, so less ‘real’). We assumed her lack of fear signified VR as less effective, however, her excitement when immersed in stimuli which previously terrified her, even if she did not associate it with reality may have been beneficial. This could be an interesting area for further research. The results of the actual flight were disappointing but a longer flight, without extreme conditions will hopefully produce the desired results. Lucy commented, “If not for the turbulence I would hope my anxiety would come down but I’m not 100% sure. It is encouraging that my anxiety was dropping, and then dropped during severe turbulence.” We agreed she has come too far to give up now so another flight is planned.
9. Appendices
Appendices have been reproduced as the scanned quality was unreadable.
9.1 DSM-V Diagnostic Criteria for Specific Phobia
- Marked fear or anxiety about specific object or situation (e.g., flying, heights, animals, receiving an injection, seeing blood).
Note: in children, the fear of anxiety may be expressed by crying, tantrums, freezing, or clinging.
- The phobic object to situation almost always provokes immediate fear or anxiety.
- The phobic object or situation is actively avoided or endured with an intense fear or anxiety.
- The fear or anxiety is out of proportion to the actual danger posed by the specific object or situation to the sociocultural context.
- The fear, anxiety, or avoidance is persistent, typically lasting for more than 6 months or more.
- The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- The disturbance is not better explained by the symptoms of another mental disorder, including fear, anxiety, and avoidance of situations associated with panic like symptoms or other incapacitating symptoms (as in agoraphobia); objects or situations related to obsessions (as in post-traumatic stress disorder); separation from home or attachment figures (as in separation anxiety disorder); or social situations (as in social anxiety disorder).
(American Psychiatric Association, 2013)
9.2 Kirk and Rouf (2004) model of Specific Phobia
9.3 Flight Anxiety Situations Questionnaire (FAS)
9.4 Flight Anxiety Modality Questionnaire (FAM)
| Flight Anxiety Modality Questionnaire (FAM): How Do I Express My Fear |
| Circle the number which corresponds to your level of anxiety in the situations mentioned. The numbers range from 1 to 5, where 1 = no reaction, 2 = a little reaction, 3 = moderate reaction, 4 = intense reaction, and 5 = very intense reaction. |
| Not at all A little bit Moderately Intensely Very
Item Intensely |
|
9.5 Huppert, Grill, and Brandt, (2017) Visual Height Intolerance Severity Scale
9.6 Death Depression Scale Templer, Lavoie, Chalgujian, and Thomas‐Dobson, (1990)
9.7 General Anxiety Disorder 7 (GAD-7)
9.8 Thought Record 1. Watching a flight advertisement
9.9 Transcription of extract of downward arrowing from session two
Th: This might sound like a silly question but your real fear is that the plane will crash?
L: Yes
Th: And inevitable death?
L: Yes
Th: Is that the worst thing that can happen?
L: Yes dying
Th: So dying is the worst thing?
L: Yes
Th: Are you fearful of death?
L: Erm… yes but not overwhelmingly ……but yes….. I think about it quite a lot
Th: do you?
L: Hmmm, it’s hard because I don’t know what’s a normal amount to think about dying but I think I probably think about it a fair bit.
Th: When you say a lot, what does a lot mean?
L: Even if it’s just fleeting, probably most days.
Th: OK so maybe we could explore that a little bit?
L: OK yes
Th: What are the thoughts and why is dying so bad?
L: But I think it’s absolutely terrifying and it’s horrible not knowing how or when it would happen although equally it could be horrible knowing how and when it would happen. The fear of what’s afterwards. I do have a Christian faith and I believe in an afterlife and a lot of people get comfort from that but I actually think that is really scary. This whole other afterlife that you know nothing about whereas I think I would be much more comfortable with the idea that I just die and then there is nothing because then you wouldn’t know anything about it. I know that’s a big existential issues for some people, the idea of nothingness but I think I would be less bothered by that and I’m just not ready to go. There is so much stuff I want to do and I don’t know if I will ever be done.
9.10 Aircraft Safety Handout
Aircraft Safety Handout
9.11 Behaviour experiment, watching an airline advert
9.12 Behaviour experiment, complete flight
9.13 Behaviour experiment, unknown flight video
9.14 VR Behaviour experiments
9.15 Behaviour experiment, The Shard
9.16 Behaviour experiment, Flight to Edinburgh
References
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington D.C.: American Psychiatric Publishing.
Barlow, D. H. (2004). Anxiety and its disorders: The nature and treatment of anxiety and panic. Guilford press.
Barlow, D. H., Allen, L. B., & Basden, S. L. (2007). Psychological treatments for panic disorders, phobias, and generalized anxiety disorder. A guide to treatments that work, 3.
Beck, A. T. (Ed.). (1979). Cognitive therapy of depression. Guilford press.
Beck, A., Emery, G., & Greenberg, R. L. (1985). Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books.
Borrill, J., & Foreman, E. I. (1996). Practitioner Report: Understanding cognitive change: a qualitative study of the impact of cognitive‐behavioural therapy on fear of flying. Clinical Psychology & Psychotherapy: An International Journal of Theory and Practice, 3(1).
Botella, C., Osma, J., Garcia‐Palacios, A., Quero, S., & Baños, R. M. (2004). Treatment of flying phobia using virtual reality: data from a 1‐year follow‐up using a multiple baseline design. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 11(5), 311-323.
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical psychology review, 26(1), 17-31.
Cardoş, R. A., David, O. A., & David, D. O. (2017). Virtual reality exposure therapy in flight anxiety: a quantitative meta-analysis. Computers in Human Behavior, 72, 371-380.
Chessa, M., Maiello, G., Borsari, A., & Bex, P. J. (2016). The perceptual quality of the oculus rift for immersive virtual reality. Human–Computer Interaction, 1-32.
Civil Aviation Authority. (2013). Global Fatal AccidentReview. Retrieved from http://publicapps.caa.co.uk/docs/33/CAP%201036%20Global%20Fatal%20Accident%20Review%202002%20to%202011.pdf
Clark, D. A., & Beck, A. (2010). Cognitive Therapy of Anxiety Disorders Science and Practice. New York: The Guildford Press.
Craske M. G., & Rowe M. K., (1997). A Comparison of Behavioral and Cgnitive Treatments of Phobias. In: G. C. L. Davey Ed.), Phobias: a handbook of theory, research and treatment. Chichester: Wiley.
Curtis, G., Magee, W. J., Eaton, W. W., Wittchen, H. U., & Kessler, R. C. (1998). Specific fears and phobias: Epidemiology and classification. The British Journal of Psychiatry, 173(3).
Ekeberg, Ø., Seeberg, I., & Ellertsen, B. B. (1989). The prevalence of flight anxiety in Norway. Nordisk Psykiatrisk Tidsskrift, 43(5), 443-448.
Epp, A. M., & Dobson, K. S. (2010). The evidence base for cognitive-behavioral therapy. Handbook of cognitive-behavioral therapies, 39-73.
Freeman, D., Reeve, S., Robinson, A., Ehlers, A., Clark, D., Spanlang, B., & Slater, M. (2017). Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychological medicine, 47(14), 2393-2400.
Furer, P., & Walker, J. R. (2008). Death anxiety: A cognitive-behavioral approach. Journal of Cognitive Psychotherapy, 22(2), 167.
Greenberger, D., & Padesky, C. A. (2015). Mind over mood: Change how you feel by changing the way you think. Guilford Publications.
Haug, T., Berntzen, D., Götestam, K. G., Brenne, L., Johnsen, B. H., & Hugdahl, K. (1987). A three-systems analysis of fear of flying: A comparison of a consonant vs a non-consonant treatment method. Behaviour Research and Therapy, 25(3).
Howard, W. A., Murphy, S. M., & Clarke, J. C. (1983). The nature and treatment of fear of flying: A controlled investigation. Behavior Therapy, 14(4), 557-567.
Huppert, D., Grill, E., & Brandt, T. (2017). A new questionnaire for estimating the severity of visual height intolerance and acrophobia by a metric interval scale. Frontiers in neurology, 8, 211.
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H. U. (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International journal of methods in psychiatric research, 21(3).
Kircher, T., Arolt, V., Jansen, A., Pyka, M., Reinhardt, I., Kellermann, T., … & Ströhle, A. (2013). Effect of cognitive-behavioral therapy on neural correlates of fear conditioning in panic disorder. Biological Psychiatry, 73(1), 93-101.
Kirk, J., Rouf, K. (2004). Oxford guide to behavioural experiments in cognitive therapy, Oxford University Press.
Marlatt, G. A., & Donovan, D. M. (Eds.). (2005). Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford press.
McNally, R. J., & Louro, C. E. (1992). Fear of flying in agoraphobia and simple phobia: distinguishing features. Journal of Anxiety Disorders, 6(4).
Oakes, M., & Bor, R. (2010a). The psychology of fear of flying (part I): A critical evaluation of current perspectives on the nature, prevalence and etiology of fear of flying. Travel medicine and infectious disease, 8(6).
Oakes, M., & Bor, R. (2010b). The psychology of fear of flying (part II): a critical evaluation of current perspectives on approaches to treatment. Travel medicine and infectious disease, 8(6), 339-363.
Rachman, S. (1977). The conditioning theory of fear acquisition: A critical examination. Behaviour research and therapy, 15(5), 375-387.
Salkovskis, P. M., Clark, D. M., & Gelder, M. G. (1996). Cognition-behaviour links in the persistence of panic. Behaviour research and therapy, 34(5-6).
Templer, D. I., Lavoie, M., Chalgujian, H., & Thomas‐Dobson, S. (1990). The measurement of death depression. Journal of Clinical Psychology, 46(6), 834-839.
Van Gerwen, L. J., Spinhoven, P., Van Dyck, R., & Diekstra, R. F. (1999). Construction and psychometric characteristics of two self-report questionnaires for the assessment of fear of flying. Psychological Assessment, 11(2).
Wilhelm, F. H., & Roth, W. T. (1997). Clinical characteristics of flight phobia. Journal of anxiety disorders, 11(3).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Psychology"
Psychology is the study of human behaviour and the mind, taking into account external factors, experiences, social influences and other factors. Psychologists set out to understand the mind of humans, exploring how different factors can contribute to behaviour, thoughts, and feelings.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




