Nursing Home Organisation Structure Evaluation
Info: 11459 words (46 pages) Dissertation
Published: 9th Dec 2019
Tagged: NursingHealth and Social Care
TABLE OF CONTENTS:
- Key Features of Work Practice Organisation
a). evaluate the work practice organisation in terms of status and size in relation to both the irish economy and world economy.
The HSE provides health and social services to every one living here in Ireland, health care in Ireland is two – tier public and private sectors exist. The public health care system is governed by Health Act 2004, which established the HSE, a new body to be responsible for providing health and personal social services, the services is rendered to both young and old people in communities all over Ireland, in hospital, and health care centers.
There are private and public services. The new National Health Service came into being officially on 1 January 2005. A person may be required to pay a subsidized fee for certain health care received; this depends on income, age illness or disability. The HSE is a large organization of over 130, 000 people, whose job is to run all of the public health services in Ireland. The HSE manages services through a structure designed to put patients and clients at the center of the organization. The HSE is funded by the Irish government. The health service has a budget of 14.6billion euro for 2016. The HSE, chief executive officer is Tony O Brien, who reports directly to the Minister OF Health, Simon Harris. The health budget for Sweden, comparable to Ireland in Population in 2016 was 4.6M.
The Minister for Health is the one in charge of the department of Health in Ireland and also he is responsible for the health care services in Ireland and he is called Simon Harris (TD) 14.6 billion was awarded in 2017 for the budget of health care, the highest ever in health care budget, they are investing the gains from recovering economy in a better health service.
I completed my work placement in a private nursing home in Limerick city. The private nursing home sector in Ireland is a rapidly growing business and provides 80% of the long term care beds for the elderly. There are approx. 4000 public nursing home beds.
The private nursing home sector contributes 190 million euro per year to the economy from employing people in this sector. There are over 400 hundred private nursing homes in Ireland, they employ over 22,000 staff throughout Ireland. And an average cost of a bed in private nursing home cost 1, 000 euros per week, as opposed to 1500 to 1600 euros in public nursing homes, but where am doing my work placement is a private nursing home and is costing 860.00 euros per week, and with a number of 57 residents. Most of the private nursing homes are affiliated to Nursing Homes Ireland, an organization which represents them and lobbies government.
The nursing home provides employment for different people ranging from nurses, care assistants, cleaners, kitchen staffs, electricians, plumbers, hair dressers, taxis, chiropodists, opticians, pharmacist, etc. Employing local people supports local environment as these people buy houses, shop, socialize and send their children to local schools. Musgrave’s wholesalers supply St Paul’s nursing home of all their goods, including all food stuffs, toiletries and cleaning agents. A local butcher supplies all the meat so this creates other jobs and revenue for the local economy. The financial status of my work placement has a huge benefit to the economy, all goods and products that are used are sourced from local suppliers, it is very beneficial as it creates employment.
Private owners of nursing homes can avail of Properties Based Incentives scheme, a tax based scheme where they can claim tax against the cost of building and redevelopment. There is wide and varied range of personal employed in the nursing home sector. Private nursing homes can benefits from a Fair Deal scheme, it is called a fair deal because it is a nursing home support scheme, it helps financially to support people who normally needs a long term stay in the residential care services. With the fair deal people makes their own contribution towards the cost of their care and the state helps in paying up the balance. It is means tested. It is of great benefit to private nursing homes as the majority of residents would not be able to afford private nursing home care otherwise.
The government fund the ETB’s in the county to deliver training courses in order to qualify people as HCA’s. There is great demand for HCA’s in all healthcare services.
HIQA are’’ The Health Information and Quality Authority is an independent authority established to drive high-quality and safe care for people using our health and social care services in Ireland.’’ www.hiqa.ie
Meeting HIQA’s 32 Standard for older people in residential care is essential. HIQA monitor and inspect nursing homes to ensure they comply with the standards. If a nursing home is found to br in breach of standards penalties can be applied and in some instances the license to practice suspended.
In order to work in the nursing home sector all staff has to be properly qualified.
Nurses must be registered with a Board Altranis
HCA’S, Have a QQI level 5 major health care award.
Other professionals like doctors, physiotherapist, electricians, plumbers, etc. must be registered with their professional bodies.
(B) SUMMARISE THE WORK PRACTICE ORGANISATIONS STRUCTURE, MAIN AIMS AND OVERALL AIMS AND OVERALL OBJECTIVES
St. Paul’s Nursing Home is a friendly, comfortable residence for individuals who require dedicated care delivered with patience, kindness and understanding. St Paul’s nursing home is a private nursing home that carters for 57 residents, mostly old people with dementia disease. It is situated at St Nessan road in Dooradoyle in Limerick.
They aim is to provide a high standard of care in a homely relaxed atmosphere.We all have the same values towards caring for our residents that is to give them the best care possible, also it is important to value our resident’s cultures. The Aims and Objectives of the nursing home are to provide a professional standard of care and the service within a safe, homely and warm environment.
Mission Statement
Person centred care, is to focus on the person, and not his or her illness, we know that each of them have a personal history and a way to approach life. It is the policy in the nursing home that all residents has a detailed care plan discussed with him or her if cognitive, or with a nominated family member, the care plan is be written with residents and a family member.
The nursing home’s employs qualified staffs to enable them carry out their jobs in an efficient way, all staff has to be Garda vetted and they must be up to date in their training. All staffs must comply to the health and safety rules in the work place to make it safe for both the residents and workers, infection prevention and control must be carried out at all times. A healthy diet is provided to the clients to nourish them and keep them in form, their policy is to provide the residents with fresh food to keep them healthy and sound. Choices of food is been provided to the residents, after each meal, the chef’s ask them what they will like to eat for dinner, because there are some that are allergic to certain kind of food.
It is the policy of the nursing home to provide activities for the residents, to enable some of them who are paralysed in one part of the body, to allow free movement of the body, allow easy circulation of blood and to keep them fit, and it also give them room to meet one another and have some quality time together. Activities like bingo are done once a week in the nursing home, it makes them look forward to that day, and it brings discussion to them sometimes. Physiotherapist visit is also part of the policy in the nursing home. Families are encouraged to involve in their daily activities, families are allowed in feeding, showering, and even taking them out on sightseeing, this will burst them up and keep them happy.
Up to date training is very important to all staffs, because the key role is to make the nursing home safe for both the client and the workers, clean, and to minimize the spread of infection, so all staffs must be trained in their own field’s that no area is lacking, it is a chain work and everybody is important.
HIQA is to promote the safety and improve the quality of health and social care in Ireland, they make sure that all task is been carried and well implemented to the safety of the residents.
ORGANISATION STRUCTURE CHART
REGISTERED
PROVIDER


Shane Scanlan, Director of nursing Person in charge
D
D
D
an

Daveen Heyworth, Assistant Director of nursing




Clinical Nurse, Manager
Service Manager







Registered Nurses
Laundry Assistants
Chefs
Cleaners
Reception


Health care Assistants
Kitchen Assistants
St. Paul’s nursing home currently employs 57 staff; the following gives a breakdown of staffs complement by grades and whole time equivalents.
- Determine the organisations culture and values as demonstrated by management practices and staff client engagement.
The nursing home has a wide range of policies, regarding staff’s performance and client care practices. It is in the policy that all staffs should report to work on time, and it is on essential to notify the nursing home if you will not be at work if you are going to be absent.
it’s in the policy that all uniform’s must be worn properly, should be clean, neat and tidy at all times, hair should not be left untidy or dangling over your face, hair should be tied neatly at all times. It is required to wear comfortable, secure shoes at all times.
In the policy all residents come first, their needs should be met at all times, their privacy and dignity should be respected all times. The environment in the nursing home should be safe at all times for the residents. It should not be cluttered with equipment’s, and all equipment’s should be placed after each use in their proper storage units to avoid any accidents to the residents or staff’s. All soiled clothes should go to the appropriate laundry bins, sharps and needles should be disposed of in sharps containers.
All staff’s must be Garda vetted at all times to make sure they are all free from crimes or convictions.
The management in my work placement are all friendly staff, there are many different cultures working in St Paul’s between Nurses and Health Care Assistants, some from Africa, Indian, polish, Latvia, Russian, Irish etc. It is very important to respect everybody’s culture no matter where they come from. We as staff respect the resident cultures and beliefs; I personally should not inflict my culture and values on anyone of the residents. In St Paul’s nursing home most of the residents are catholic, and the church inside the nursing is catholic, they have mass twice in a week, the priest comes in to say the mass, not all the residents are able to attend the chapel, so they do have some sisters who do go around the rooms with a bell in their hand and giving them holy communion and even some of the staffs do receive the holy communion too.
We all have the same values towards caring for our residents that is to give them the best care possible, also it is important to value our resident’s cultures. I feel comfortable working in St Paul’s because the staffs are really helpful, they are reliable when you need them, I like team work, because it gives room to know the staff, team work also makes me know my weakness and strength, and know where to improve on. The staffs are really helpful in St Pauls because when you ask questions they are very ready to give you genuine answers without mocking you, they are quick to respond to any questions that needs answers, they are very easy to contact at any time.
In St Paul’s nursing home, some mornings are very tense when there is shortage of staff, we have to make sure that all the residents are been cleaned and dressed up for morning mass. I find it difficult sometimes with clients with stroke, but with the assistance of other staffs, we are able to get along quickly, but in the afternoon time, things are kind of calm, because most of the residents are in bed, or doing activities. Those that are not sleeping, I will go around giving them water or juice, then I have the opportunity of talking to some of them and giving them a listening ear. The staffs are very willing at any time to support one another when in need, and most of them we are in pairs working so there is someone to support you at all times.
St Paul’s Nursing home has a free parking space for worker’s and visitors, there are restricted areas that has marked name on it, that nobody is allowed to park there, like the space for the director of nursing, and some few senior staff’s. The nursing has a canteen, but a small one , just a round table with about 6 chairs, which is very small, compare to the number of staff’s working there, but they provide bread and milk for all staff, but meal’s are not been given to us on work placement, all staffs are entitled to a meal each day.
There is a private rest room in my nursing home for staff only, it is been locked at all times, and the key hanging over the door, and there is a sign on it written for staff only, which is always kept clean and tidy. There is a counselling room for clients and family, when a resident dies the families are been called in the counselling room and talked to them about the procedures to be followed.
There are various activities carried out in the nursing home to encourage them and make them feel comfortable, like birthdays are been celebrated, the families comes in to decorate the room with pictures. Birthday cakes are been brought in by family member’s, soft drinks, juice are been shared, photographs are allowed with only members, staffs are not allowed to take photographs without the consent of the family. Sometimes when it’s very hot the nursing home do organise the ice cream van do come in and all the resident’s will be brought out and given ice cream, and we care assistants and nurses do supervise it. Once in a while the nursing home do organise BBQ, for the residents, and their families are all welcome to assist in feeding them.
Staffs are allowed to take residents out once in a week for shopping, sometimes sight-seeing picnics are been organised for the residents considering if the weather is friendly, and they do go in groups, and families and friends are all welcomed.
KEY FACTOR WHICH IMPACT THE WORK PRACTICE ORGANISATION
- Evaluate the impact of globalization, new technology and science on the work practice
My work placement St Paul Nursing home is not Global healthcare company, but it is part of the worldwide healthcare service industry.
There are many practices and issues in healthcare that are global such as smoking, diabetes, ageing and obesity. Healthcare settings around the world implement common practices and treatments in managing various conditions and diseases. Worldwide there are many challenges facing health services due to obesity, dementia, smoking, alcohol consumption and supporting an ageing population.
One of the global practices that we use in St. Paul’s Nursing home is the 5 moments of hand hygiene.
The 5 moments of hygiene has emerged from WHO Guidelines on hand hygiene in health care, it is known factor that, clean hands saves life and stops the spread of any infection. Washing of hands is the most important practice in any healthcare sector and its easiest way to saves lives, because the hand is the most easiest way to pick bacteria’s. Washing of hands prevent the spread of bacteria’s like MRSA, common cold and flu, runny nose, chest infection, eye infection like conjunctivitis. In my nursing home to stop the spread of bacteria’s, it is necessary to wash hands before and after touching a patient, their surroundings, after handling bodily fluids and when carrying out ascetic procedures. Washing of hands after the use of toilets is also advisable to avoid the spread of infection. The 5 moment of hand washing also applies to visitors that do come in to visit their family member, its advisable for them to wash their hands before leaving the health care sector.
DEMENTIA VILLAGE
Due to the ageing population globally dementia is a major health concern. There is a wide range of global research and huge amounts of money invested into finding out the cause and finding new treatments and approaches to dementia. One model of care that has started been replicated globally is the 1st dementia specific village ever built.
Hogeweyk is a gated model village setting in weeps Netherland, the village was opened in December 2009, with a budget of about 19.3 million euros. it was designed specifically as pioneering care facilities for elderly people with dementia. The Hogeweyk is set out like a village with 23 house’s, for 152 dementia suffering senior’s, there is a super market, hair dressing saloon ,theater, pub and a walk way garden. Hogeweyk dementia village offers 7 different lifestyle settings, they have the Christian, Goois ( upper class) Artisan, homey, Indonesian and cultural. The residents are allowed to manage their own house hold with a team of staffs to assist them regularly with washing of their clothes, cooking, and showering. The dementia village has 250 staff, including volunteers trained in aspects of dementia working there. Their grocery shopping is been done in the Hogeweyk super market.
The village has a street, squares, parks, and gardens, where the residents are free to roam about at any time, selection of restaurants, bar’s, theater are available for the residents and also for people who lives in the neighborhood, visitors are welcome.
Based on this model of care for people with dementia, Ireland is to open its first Dementia specific village in the village of Bruff, in Limerick in September. This dementia village will be set on a 4 acre sit in the central of Bruff. 18 homes will be build and each rooms will be having their own living room, bathroom, bed room and their own separate garden, Colette Ryan care bright general manager said that those going to live in this new village will feel safe, and it is a place that they will flourish, she also promise that friends and family will be able to pass the night with their relatives in the dementia village.
NEW TECHNOLOGY
Recently technology in the health care facilities continues to advance, it is considered now that technology is the driving force behind improvement in the health care sector, one of the key factors that has improve is the patient care, this days the information technology has now made patient more safer.
physicians and staff’’

The use of Epiccare in the nursing home has made things generally easy for staff’s and client, all activities of day of the client is recorded in to the Epiccare data base, recording of how much fluid each client consume in a day, how much food that was eaten, elimination pattern, vital signs, personal hygiene attended to, and medication dispensed. The Epiccare monitor is located on each office of each floor in the nursing home.
ALARM MAT’s
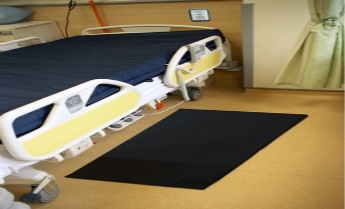
Clients suffering from dementia are known to wander at night, This day’s there are major concerns to prevent the risk of falling mostly at night in the nursing home to residents who like to wake and wander about in the nursing home, so a new device of technology came up with the idea of alarm mat, this device is placed in front of the client’s bed. When he or she stands up on the mat, the alarm goes off calling the attention of the career. Some alarm mats can be placed by the exit doors, lift entrance, stairways entrance, so as to detect where the clients is.
In St Paul’s nursing home, there was a case of a lady who likes to wander at night, on this particular night; she was nowhere to be found. They searched all over the nursing home, but she was not seen, they were about ringing the police, when one of the care assistant said they should check the nursing home chapel, , there she was on her own in the dark on the floor, she has fallen down and couldn’t call for help, so since that day an alarm mat was brought under bed, and been used at night when putting her bed.
SCIENCE
There is an enormous and continuous amount of global scientific research in the healthcare industry. Scientists are always looking for cures and treatments for the many different illnesses and conditions that exist,. Everyday there is new developments and clinical trials for new drugs emerging. One of the advances that have been made is the development of fluid thickners for people with dysphagia.
Thickener’s for dysphagia
The thickener is normally used in the management of dysphagia, it is to help Bolus control, and also help in preventing aspiration. Experts discovered that the thickener helps the liquids to go down the throat without causing choking. Older people with swallowing problems are always at risk in choking, dehydration and aspiration. Most experts suggest using the commercial thickener because there are different brands, and they come in different taste, texture and flavors. Some taste very awful. The majority of older people suffering from advanced dementia or Alzheimer disease, start to lose their sense of taste, so majority of them doesn’t even notice the taste. In my WPO, there was a lady that who was still a intermittently cognitive, when her thickener was changed she noticed the taste and refused taking the new one, I had to report to the nurse, when the old thickener was brought and given to her, she drank it confidently, while the other lady she was sharing room with, who has a chronic dementia couldn’t even notice the new change.
Diabetic implant
Those with insulin dependent diabetes must constantly monitor their blood sugar level, they must constantly monitor their food intake, they must know what to eat, they must keep track of almost everything to make sure they maintain stable blood sugar levels and assess the amount of insulin they require.
Technology has advanced, that this days there is a huge difference in testing blood sugars to the days of finger pricking. Now there are wearable, waterproof implants that are equipped with a sensor to detect blood sugar levels. They come with a small scanner which the person swipes over the implant and a digital recording of the blood sugars is displayed. The person then calculates the amount of insulin they require.
Some of the new technologies are smart skin patches, contact lens, and foot wear. Skin patch has a sensor to monitor the blood glucose in sweat and it will instantly release the dose of insulin to correct high blood glucose. Technology has developed skin patches can be attached to your skin, in the event of low blood sugar it will send direct message to your phone telling you to eat. Implanted technology is a special capsule that is implanted in to the patient’s body, it will function like the pancreases, as of now the product is currently in the clinical trials, and it has been successfully carried out in 4 humans, more of this trails are expected.
- Review the impact of relevant government policy on the Work Practice Organisation
Garda vetting policy
St Paul’s implements many government policies which must be adhered to at all times
The National Vetting Bureau (Children and Vulnerable Persons) Acts 2012 to 2016 provide a statutory basis for the vetting of persons carrying out relevant work with children or vulnerable persons. The Act also creates offences and penalties for persons who fail to comply with its provisions.
The Garda Central Vetting Unit (GCVU) provides vetting on behalf of organisations employing people working with children or vulnerable adults. The GCVU carries out vetting for each sector through a central point of contact. The vetting unit releases criminal history information on the person who is been vetted. When HIQA carry out their staff inspections they check to ensure that all staff have been vetted.
Every employee in the health care sector requires Garda vetting; everyone in the nursing home must be vetted before the commencement of work placement. They need to cross check the individual if they are free from any conviction’s in the state, and the Garda can only disclose your personal information to the sector that need it. The details must include all completed prosecutions, if they were successful or not, or any pending prosecution. It is very important that every employer should adhere to this policy because it protects the people who are been cared for. Without this Garda vetting sex offender, violent criminals, murderers etc, might GAIN employment in the services and they may be dangerous to this vulnerable group of people, and also to their co workers
In 2012 a bill was passed, it was an offence to employ any one to work with vulnerable adult or children before receiving a Garda vetting, and there is fine of 10,00 euros, or a minimum of 5 years imprisonment. To commence any job, the Garda vetting must be filled through the internet, but before it was getting a form, but due to advance technology it can be filled through the net and summited on line, and a confirmation will be sent to your email, when it is ready a copy will be sent to you, and one copy to your employer. Before my work placement I was vetted and got the confirmation before I commenced my work at St Paul’s Nursing home. And I still have to be vetted before starting a new job.
HIQA Standards for Residential Care Settings for Oder People – Health Act 2007

HIQA was established it may 2007 under the 2007 Health Act to continuously drive the improvement of health in Ireland’s health and social care services. They are responsible for developing the quality and safety standards in care settings. They monitor standards of quality and safety in the health services and they also investigate issues regarding serious concerns about the health and welfare of service users. HIQA does this inspection to safe guard the older people, they ensure that the wellbeing, quality and health of the vulnerable people are very well protected and promoted. The regulations played an important role in marking sure that there is continuous improvement in health care sector.
They developed 32 standards that all residential care facilities for older people must adhere to. These standards cover issues such as privacy, dignity, management, recruitment, care plans and safe environments. HIQA carry out planned and unannounced inspections of nursing home facilities. If a nursing home is found to be in breach of any of the standards a report is issued and recommendations for improvements required made. They give the organization a time frame in which to comply with the standard. If breaches are not corrected HIQA have the power to apply penalties or remove the licensee to operate.
In St Paul’s HIQA standard has a huge impact on the way work is been carried out, there are 32 standards that must be met, and the instructions set out by HIQA, gives the nurses and career directions on how care should be carried effectively which will lead to a better and safe environment for both the residents and staff’s. HIQA visited St Paul’s nursing home on the 6th of April 2017, during my placement, the standard was met and they passed all requirements.
- Asses if social or ethical issues have affected the work practice organization or may impact in the future.
St Paul’s nursing home has accommodation for 57 residents with diverse abilities and needs. Some of the residents are cognitive, while some are suffering from dementia, some are cognitive but paralyzed, and some of them need daily care in feeding, showering, toileting, and moving from bed to wheel chair, while some are able to feed themselves, some need just a little bit of assistance.
There is a bit of discrimination there because some clients do have family and friends who do come for visits, so the staff gives them more attention than those who has nobody to visit them. There was a day I gave a lady a bath bed, got her dressed up, only for the staff to come in and told me to change her clothing, and I asked her why ?, she told me that the dress is not for today because the children are coming and they won’t like their mum wearing them cloths. I changed her clothes, and she asked me to do some make up for her, of which we don’t do that every day, but for one dementia lady nobody even cares to give her extra care, because no one comes to visit her, she has no children, and all through my time there no came to see her.
Among the staff there many different cultures working in St Paul’s between Nurses and Health Care Assistants, we have some from Africa, some from India, some from Poland, and some Irish. I find out that those from the ethnic group like doing things in common, speaking their language, which is against the law of the nursing home. There was an incident that occurred, I was working with two polish ladies, we were taking care of a disability client, they both left the client unattended, they were talking in their language and laughing, neglecting the client, I felt bad for the client. Some residents do have some discrimination tendency in them, when they know you are from a different race, they don’t want you to carry out any (ADL) on them, there was an incident that occurred. I went into client’s room, immediately she saw me, she just turned her face to the other side and ask me to leave the room, that she doesn’t me come close to her. I felt bad at first thinking because of my colour, but I moved backward, was calm tried to explain to her that I am just here to help in caring for her, but she was not interested at all in what I was saying. When I found out I won’t be able to convince her, I had to call in a staff, immediately she heard the voice of an irish assistant, she quickly turned and gave her a smile, I felt bad, but I did not show it, I still put on my smile.
Privacy
Giving the resident their privacy gives them the sense of belonging, the residents has right to refuse what they don’t want, and what they desire, by ensuring the privacy of the residents, it is wise to knock on their door before going in, you just do not intrude on them, is like invading their privacy, it is also wise to call them by their names, than calling them pet names, giving them choice’s in selecting their own clothes makes them feel comfortable, while dealing with a resident in a shared room it is always in your interest to secure their privacy by drawing up curtains, protecting them from the other resident seeing them.
Making sure that all their personal belongings is well kept and secured after each use, things like jewelries should be kept in a safe place, and making the residents know were the items are kept. Asking permission before any ADL is been carried out on the residents. It is best to know your clients and study their mood, when they are down and sometimes you try to cheer them up, but if you notice they are not in the mood is best you live them than invading their privacy at that time. When the resident receives a mail, it is best to deliver it to them unopened, it is left for the resident to ask you to open or not. All information regarding the client is confidential to the MDT.
End of life facilities 
Definitely some of the residents living in the nursing home will die there, for some resident’s the nursing home is like waiting room for them to die. When the residents is no more responding to treatment, little or no more appetite, much pain’s, changes in blood pressure, not eating any more, or having difficulties in breathing, less bowel movement, this will indicate that the residents is almost coming to end of life, so the nurse in charge speaks with the families. She make an appointment with them in a quiet room, she will explain to them to them the condition of the resident and tell them what to expect and ask them what they will like the resident to wear, if they want rosary in their hand. If they wear glasses would they like him or her to wear his glasses, different kind of questions will be asked.
The families are allowed visiting even late at night, I remember a case of a lady who was in her end of life care, the families were allowed to stay till late night, and when she passed away at about 1am in the morning her families were by her bedside. St Paul’s has the hospice sign on the door to indicate the end of life; the signs can be displayed in the ward, nurse’s station, or the entrance to the ward. It can still be displayed even when the patient has died, very important to explain the hospice signs to the families of the resident, making them to understand that some quietness and respect is needed at this time. You cannot display symbol at any other time.
Ageing population
In Ireland the ageing population of over 65 years old has been increasing at a faster rate than that of our EU neighbors. As a standard and accepted international sector bench mark health care planners plan on the basis that 4.5% of the population aged 65+ will have a requirement for long term residential care. The evidence is now pointing significantly that the increase in the need of nursing home care and its future, Analysis conducted demonstrated that there will be a short fall in the number of nursing home beds, approximately 8,000 beds, the equivalent of approximately new nursing homes in 2021. There is a waiting list for beds in St. Paul’s and in other nursing homes in the country such is the demand for residential care. Older people would prefer to be cared for in their own homes but there is not enough financial aid provided to them to stay at home.
 (The Irish Longitudinal Study on Ageing (TILDA), 2014)
(The Irish Longitudinal Study on Ageing (TILDA), 2014)
Extract
22nd February 2017 – Statement by Marian Finnegan, Chief Economist, Cushman & Wakefield, Wednesday 22nd February, 2017.
There is a very strict policy on use of restraints in the nursing home. They are only, if ever used as a last resort. Any restraints used must be prescribed by a doctor, constantly monitored and documented. If a client has been referred for bed rails they must be checked every 15 minutes and the staff member who checked must sign the restraint form. St. Paul’s requires staff to access training in MAPA, this gives staff the skills and knowledge to manage challenging behavior in a respectful and dignified manner.
- Comment on any impact to the work practice organisation in relation to economic and population shifts
Public expenditure in Ireland on health has dropped by 9% since its historical peak in 2005. To a large extend the economic crisis also helped to highlight the need for health system reform. The global crisis led to the financial crisis in 2008, and it made the internal banking system to collapse, this also led to unemployment for the younger ones at the rate of 3% , the reduction of cut in staffs numbers and staff pay was reduced in the health sector, due to the critical crisis and financial pressure those on low income has to receive free medical card scheme.
Ireland began to recruiting nurses internationally in 2000; in between 2000 and 2010, 35 percent of new recruits into the health system were non EU migrant’s nurses. Ireland as for now is more heavily reliant upon international nurse recruitment than the UK, New Zealand or Australia.
International nurse recruitment campaigns were iniated in 2000 to attract migrant nurses from outside the EU into the Irish system. The migrant nurses became intergral to the health system, ( INMO) noted in 2008 that Ireland would be forced to close hospital beds without the presence of migrant nurses. As a result of the recession and the wage cuts for nurses, Irish trained nurses emigrated in big numbers. Newly qualified nurses pay was reduced by €4000 to €22,000 in 2010. The UK has been the most popular destination, with 4,270applications, followed by Australia with 3,594, a total of 1,214 nurses applied to go Australia in 2011 alone.
 The international recruitment policy and the emigration of Irish nurses has led to a very multicultural healthcare workforce in Ireland. The majority of hospitals and nursing home have nursing staff and HCA’s from many different countries employed; they are actually dependent on them to keep operating.
The international recruitment policy and the emigration of Irish nurses has led to a very multicultural healthcare workforce in Ireland. The majority of hospitals and nursing home have nursing staff and HCA’s from many different countries employed; they are actually dependent on them to keep operating.
Irelands ageing population will present big challenges for the health services in the coming years. Every day over the next 10 years an additional 7 older people in the republic will require long-term residential care or home care. www.irishtimes.com
There are concerns as to who will provide this care as there is an expectation that their will be an increase in emigration of females.
Article Extract
Ireland’s Filipinos: caring for our young, old and sick
Nearly one-third of Filipinos in Ireland are nurses. Many more mind the elderly and disabled
Future Trends
“ By 2021: – The number of people aged 65+ using residential long term care will rise by 12,270 in ROI, an increase of 59% since 2006- An additional 23,670 older people in ROI will use formal home care, up 57% since 2006. Demand for all day/daily informal home care by people aged 65+ with disabilities will expand by 23,500 in ROI (57%) and the demand for informal care generally by 11,000 in NI (26%) (Wren et al., 2012). • 2,833 extra people will require residential or formal home care each year in ROI between now and 2021 and 565 extra people in NI (Wren et al., 2012). • The numbers requiring formal residential or home care will increase further if informal carers are unable to provide the same rate of care as in 2006, which would require all day/daily care for an additional 1,565 people each year in ROI and informal care to 730 in NI (Wren et al., 2012). • In ROI, 14% of older people with limiting disabilities living in the community were receiving no care (8,020 people) compared with 2% in NI (1,100 people) in 2006” (
Wren et al., 2012 http://www.cardi.ie/userfiles/Long%20Term%20Care%20(Web)%20(2).pdf c
Health, Safety & Welfare at Work: Employment & Equality
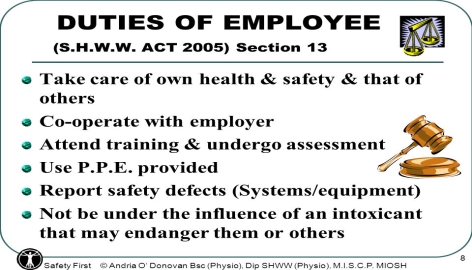
HEALTH SAFETY AND WELFARE AT WORK ACT 2005
‘’The Health and Safety Authority is the national body in Ireland with responsibility for securing health and safety at work. It is a state-sponsored body, established under the Safety, Health and Welfare at Work Act, 1989 and it reports to the Minister for Enterprise, Trade and Employment.’’
The 2005 Act tends to prevent or reduce accidents and ill health at work. The HSA is the center of information and advice to employers, employee’s and self-employed on all the aspect in the work place on health and safety issues, they also help to develop good policies and good work practices to risk assessments and safety statements. It also advises on the use of intoxicant at work it also deals with the medical fitness at work place.
The Safety, Health and Welfare at Work Act 2005, which came into force on 1st September 2005, repealed and replaced the Safety, Health and Welfare at Work Act 1989. It was brought in to make further provision for the safety, health and welfare of persons at work. This Act clarifies and enhances the responsibilities of employer’s, the self-employed, employees and various other parties in relation to safety and health at work. The Act also details the role and functions of the Health and Safety Authority, provides for a range of enforcement measures that may be applied and specifies penalties that may be applied for breach of occupational safety and health.
In St. Paul’s good housekeeping benefits both employers and employees are alike. There is a policy on elimination clutter which is a common cause of accidents like slips, trips and falls and fire and explosions. Housekeeping standards are set and monitored.
Effective housekeeping can eliminate some workplace hazards and help get the job done safely and properly. Poor housekeeping can frequently contribute to accidents by hiding hazards that may cause injuries. In St. Paul’s Housekeeping is not just for cleanliness, it includes keeping work areas neat and orderly maintaining halls, floors, free of slips and trips. Training is very important to promote and provide a safe and healthy enviroment for residents and staff.
St. Paul’s carries out regular training for its employees in fire safety, infection control and patient moving and handling. All staff are required to attend training when requested and are expected to keep their certification in date.
In the work placement there are visual signs regarding health and safety precautions alerts. Staffs meetings on health and safety is very important, it is an opportunity for staffs to voice concerns or suggestion on policy.
DATA PROTECTIONACT 2003
‘’When you give your personal details to an organization or individual, they have a duty to keep these details private and safe. This process is known as data protection. We refer to organization’s or individuals who control the contents and use of your personal details as ‘data controllers’’

Most People give out their personal information’s about their selves to Government bodies banks, insurance companies, medical professionals, telephone companies. Under the Data Protection information is to be used to meet up certain conditions. They collect details from person, and save it to the data base and can also be used to identify you when you need their services again. Under the law we all have the right regarding the use of these personal details, and the companies also have some right or responsibilities of how to handle this information and the company has no right to transfer your information to another company. You have the right to data protection when your details are held in computer or on paper.
The aim of the data protection rights is to help you in making sure that all information stored about you is correct, it is only available to the company that you gave it to, and must be used only for the purpose stated. Information should be kept no longer than when needed. Before giving out your information, you must know the name of company and even the name of the caller, in case of any emergency and you need to confirm certain issues, you need to ask why the details needed and what for. If your information is gotten from another company and they ring you, you have the right to ask them the name of the company that gave out your details. Compensations can be claimed through the court if your information’s is been damaged or miss handled.
All nursing homes have to obtain and store important information regarding clients in their care, such as care plans, financial documents & medical history. In the nursing home sector confidentiality of residents is very important. Client information must not be passed to any third party. The nursing home has the obligation to protect his resident’s, personal information, any illness of residents must not be discussed out of the nursing home and even among staff, their privacy and dignity must be kept at all times. On commencing employment with St. Paul’s an employee has to sign a confidentiality agreement.

ORGANISATION OF WORKING TIME ACT 1997
Every worker has an entitlement to a specific set of rights as prescribed by the relevant employment legislation. However, these entitlements are only a minimum, and it is possible to contract or agree over and above those rights. Workplaces provide terms and conditions of employment above the minimum legal standards as set out in law. This regulates the different employment conditions including the maximum working hours, night work, annual and public holiday leave.
WORKING HOURS
The maximum average working hours in a week cannot exceed 48 hours; it doesn’t mean a working week cannot exceed 48 hours. The average is most important., it is clear that the 48 hrs doesn’t include the annual leave, sick leave or maternity leave, the average may be calculated as follows.
- Over 4 months for most employees
- Over 6 months for employees working in other industry like prisons, gas electricity, airport, agriculture and employees in business which have peak periods at certain times of the year such as tourism.
Over 12 months where there has been an agreement between the employer and the employees to this effect. The agreement between employer and the employees must be approved the Labour court.
NIGHT WORK
The Night Work Is Normally Done between midnight and 7 am, a night staff should not work more than 8 hours in 25 hourrs, the law also states that younger people cannot do the night shift, also pregnant women may be exempted from night shifts, if a doctor certify them unfit, that it might affect the health of the unborn child.
BREAKS
All staff’s are entitled to 15 minutes’ break after a 4and half hour work period, if you work more for more than 6 hours none stop you are entailed to 30 minutes break, and you will not be paid during this break period, 11 hours of rest is needed in 24hours.
ANNUAL LEAVE
4 weeks of annual basic paid leave you are instilled to
PUBLIC HOLIDAYS there 9 public holiday in a year, most people prefer working on this day because they get double pay.
In St Paul nursing home, you are allowed to work either 8 hours, or the 12hours shift, those doing night shift’s starts from 9pm till 8am. Those on long shift are entailed to one hour break, but it has to be taken after 4 hours of work non-stop. When was on placement I worked from 8am to 3 15pm with a 30 minutes break, but I have to take 15 minutes in the morning and the other 15 minutes in the afternoon, and they are very strict with their break schedule. I gathered from the staff that in every 100 hours you work, you are entitled to a week off, you either take it or accumulate it and go for annual leave. On public holidays like bank holiday’s, St Paul’s pay double, on Sunday’s they pay an extra of a euro/hour, and there are no difference paid on night or morning shifts.

INTERNAL AND EXTERNAL POLICIES AND PROCEDURES
- EXPLAIN THE INTERNAL AND EXTERNAL POLICIES AND PROCEDURES APPROPRIATE TO YOUR OWN ROLE AND THAT OF OTHER WITHIN YOUR ORGANISATION
INTERNAL POLICIES
DRESS CODE
 In any health care sector a uniform or dress code is needed to identify those working there, and it is always proper for employees and employers to maintain a professional appearances at work, they should always appear well groomed, clean and tidy because it will contribute to a positive impression. Appearance is significant in portraying a professional image to all users of its service, whether residents, visitors, or colleagues.
In any health care sector a uniform or dress code is needed to identify those working there, and it is always proper for employees and employers to maintain a professional appearances at work, they should always appear well groomed, clean and tidy because it will contribute to a positive impression. Appearance is significant in portraying a professional image to all users of its service, whether residents, visitors, or colleagues.
Our uniform is a white tunic and black/navy blue trousers. We have no changing facilities so we wear our uniform to and from work.
In St. Paul’s it is the duty of all employees to comply with the principles of the dress code policy, failure to adhere to the employers required standard of dressing and appearance may result in misconduct and can lead to some disciplinary actions. It is the right of the manager or supervisor to talk about the dress code to a new employee. They are also in charge in monitoring and reinforcing the dress code on new staff. It is the policy of the nursing home for all health care workers to always have their name badge on their chest and the name of the company is written on it. Personal hygiene is required at all times, hair should be tied up, no nail polish, nail’s should be cut short, no visible tattoo’s, no rings to be worn apart from wedding bands.
Hazards can occur at any time and it can result in foot injuries, so appropriate and comfortable foot wear is recommended to protect the employee’s.
‘’The Occupational Health and Safety Act and Health Care Regulations states: “if a worker is exposed to the hazard of a foot injury, the worker shall wear foot protection appropriate in the circumstances; and to the hazard of slipping on a work surface, the worker shall wear footwear with slip resistant soles.”
SMOKING

As Tobacco is one of the major factors leading to death, or cancer, in Ireland over 5,500 smokers die each year from smoking related disease’s
Smoking is forbidden in enclosed places in Ireland. The ban was introduced as part of the Public Health (Tobacco) Act, 2002 (section 47) regulations 2003. In St Paul’s nursing home there are facilities for smokers outside the building. Visitor’s and some residents who do smoke are free to go out and do their smoking. There is a facility for them to empty the butt of the cigarette, than littering it all over the place. No one is permitted to smoke inside the building, there is a sign in almost every area of the building of no smoking, and there is also an alarm bell if any smoke is detected. Staff is permitted to smoke outside in the gardens. Residents are permitted to use electronic cigarettes inside but staff is forbidden to do so. If I or any of my colleagues breach this policy we can have disciplinary action taken against us.
Confidentiality Policy
‘’Is one of the core duties of medical practice. It requires health care providers to keep a patient’s personal health information private unless consent to release the information is provided by the patient’’
Clients information are very important to the employer, all information should be kept from the public, all information taken from clients must be based on confidentiality, and should not be discussed with a third party, the residents can only nominate a family member that his private care can be discussed with.
All my information be given to St. Paul’s should be considered confidential and it must not be passed onto anyone else. All information’s given must be treated with respect and care. The management are required to assume responsibilities for the employees information’s entrusted in their care, it is advisable that confidential paper and records should not be kept open or unattended. All client and employee information is kept safe and locked away in a safe or drawer’s. The keys of such cabinet are not available to unauthorized persons. Any loss or unauthorized disclosure of confidential information has to be reported to your supervisor or director of nursing immiediately. An agreement of confidentiality should be signed before taking up their employment.
All employees in St. Paul’s signed a confidentiality agreement; they must not discuss or share information about the residents or the activities of the nursing home outside of the MDT. Any breaking of the confidentiality agreement will lead to disciplinary action. Employees are not allowed to post photographs or make comments about ST. Paul’s on face book or other social media.
EXTERNAL POLICIES

2017 – National Standards for the prevention and control of healthcare-associated infections in acute healthcare services
‘’Infection control is the discipline concerned with preventing nosocomial or healthcare-associated infection’’
HIQA’s revision of the National standards for the prevention and control of healthcare- associated infections in acute healthcare services identifies 29 standards that are up-to-date infection prevention and control practices that are effective in managing transmission of infections. Their purpose is reducing healthcare -associated infections. Healthcare-associated infections are infections such as surgical site infection, pneumonia, urinary tract infection, bloodstream infection and gastroenteritis.
Healthcare associated infections seriously impact on patients and their families, resulting in serious illness, long-term disability and on occasions death. There are also impacts on hospital services due to cost of healthcare associated infections such as prolonged hospitalization isolation beds and ward closure.
The standards cover eight areas. Some sections have been given extra focus, including communication with the patient; local, regional and national governance structures; and workforce training. New standards include risk management, decontamination of equipment and health and well-being of patients. There is a requirement for healthcare managers to achieve an outcome for each standard.
Infection prevention and control policy is assisting the members of staffs in reducing dissemination of infections associated with health care.. The important goal is to make sure that member of the state endorse quality health care, that is safe for the resident’s, staffs, , and everyone who comes in to the nursing home at all times from transmission of infection during care and hazardous procedures whether the risk is known or unknown. Having going through St Paul’s policy on infection control, I found out that it is very compulsory and important to wear PPE where necessary and the importance of cross contamination, or infection control by using the hand washing techniques at all times. The policy must be adhered to at all times.
In St Paul’s nursing home infection prevention control procedures must be followed at all times, staffs must undergo the training, all the staffs has the responsibilities in making sure all instructions are been followed in accordance with the policy so has to endanger their selves and the residents from any disease’s, using safe practice, I make sure am working in pairs when using the hoist, I always make sure I wear my PPE when necessary to avoid any infection.,
SAFE GUARDING OF VULNERABLE PERSONS (ADULTS ) POLICY(RISK OF ABUSE)
The Social Care Division of the HSE supports the ongoing service requirements of older people and persons with disabilities. They have developed the above policy and all people working in HSE settings must receive training in this area.
In recent years society has had to face the reality of abuse of children. Now there is a focus on incidents of Elder Abuse, and the difficulties in responding to the issue in a respectful manner All service providers must learn from these incidents and put in place g supports, policies and procedures to promote the welfare and preventing the abuse of vulnerable persons
The HSE, Social Care Division, considers a Vulnerable Person as” an adult who may be restricted in capacity to guard himself/herself against harm or exploitation or to report such harm or exploitation”.
The publication of this policy for statutory and non‐statutory service providers is part of the Social Care Division’s commitment to promoting the welfare of vulnerable persons and safeguarding them from abuse. Its purpose is to protect the rights of vulnerable persons to live meaningful lives in safe and supportive environments.
The implementation of the policy is committed to the safeguarding of vulnerable persons from abuse. It admits that all adults have the right to be safe and to live a life free from neglect, fear and abuse. All healthcare providers, statutory and non‐statutory, have to ensure that, service users are treated with respect and dignity, in an to promote welfare and to prevent abuse. It states all healthcare services have a publicly declared ‘No Tolerance’ approach to any form of abuse. It is the service provider’s responsibility to ensure that all staff has the required training in SOVA.
This policy was introduced to protect the rights of older people, their dignity, privacy, and independence. Elder abuse is a major concern of all staff’s in the health care sector. All staffs has to follow the procedures of the policy procedure’s, protocol’s, and guidelines in order in making sure of the safety of the older people in their care, this policy is concerned with people aged 65 and over. There are several forms of abuse, any or all of which may happen as a result of deliberate act, a person may experience more than one form of abuse at any time.
FORMS OF ABUSE ARE
- psychological abuse
- Financial neglect
- abuse
- physical abuse
- sexual abuse
As an health care assistant is my duty to be alert at all times because the older people are vulnerable to abuse at any time and if I notice or see any sign I must make sure I report to my supervisor following the correct reporting procedures in my nursing home. During my course I participated in SOVA – Safeguarding of Vulnerable Adults training for which I received a certificate. It has made me aware of the different types of abuse, my duty of care to report any suspicions. It has also made me aware that neglect of a person’s wishes and requests is a form of abuse.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Health and Social Care"
Health and Social Care is the term used to describe care given to vulnerable people and those with medical conditions or suffering from ill health. Health and Social Care can be provided within the community, hospitals, and other related settings such as health centres.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




