Principles of Peri-Operative Veterinary Nursing Support for Horses
Info: 7161 words (29 pages) Dissertation
Published: 9th Mar 2021
Tagged: Veterinary
Introduction:
The word ‘Peri-operative’ is a term used to describe around the time of surgery, more specifically the time extending from when the patient is admitted to the hospital to the time they are discharged. This assignment will present 4 surgical cases that require different types of peri-operative nursing support that will cover both planned and emergency surgeries including abdominal, orthopedic and a head and neck procedure. This will demonstrate the varied reality of nursing in relation to veterinary staff, owners and most importantly the patient itself.
Case 1- Emergency Abdominal
Species: Equine
Breed: Irish Draft
Age: 17 years
Weight: 650kg/ 17hh
Case Identifier: 3856
Veterinary Diagnosis and treatment:
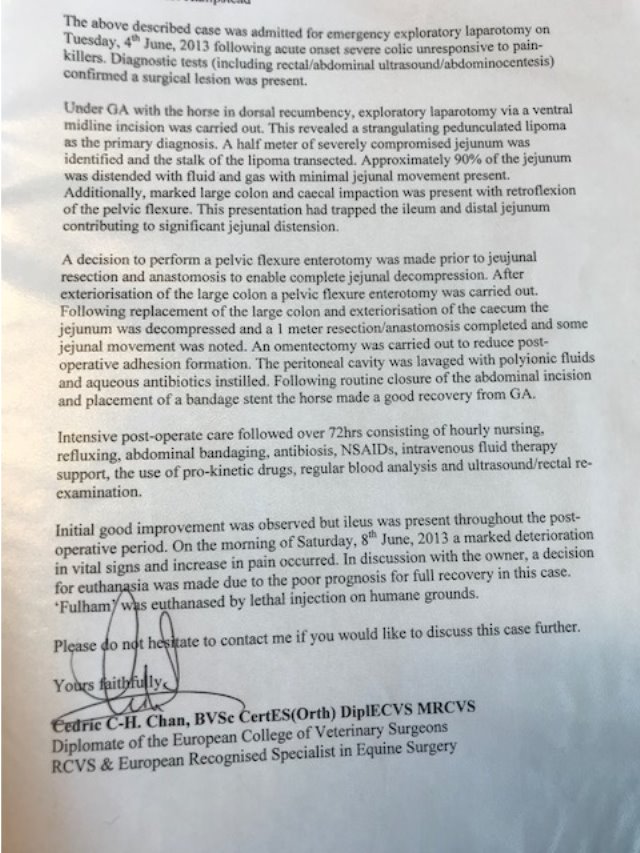
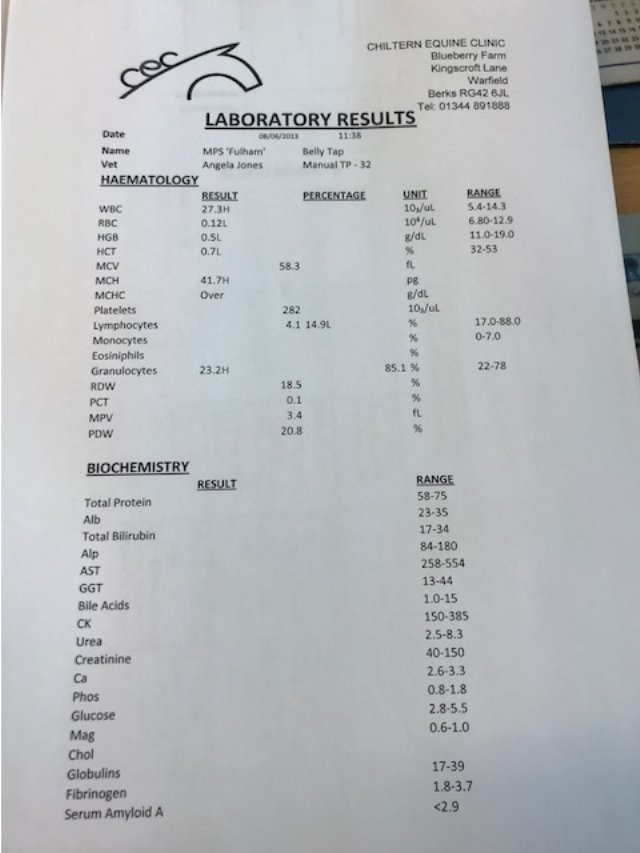
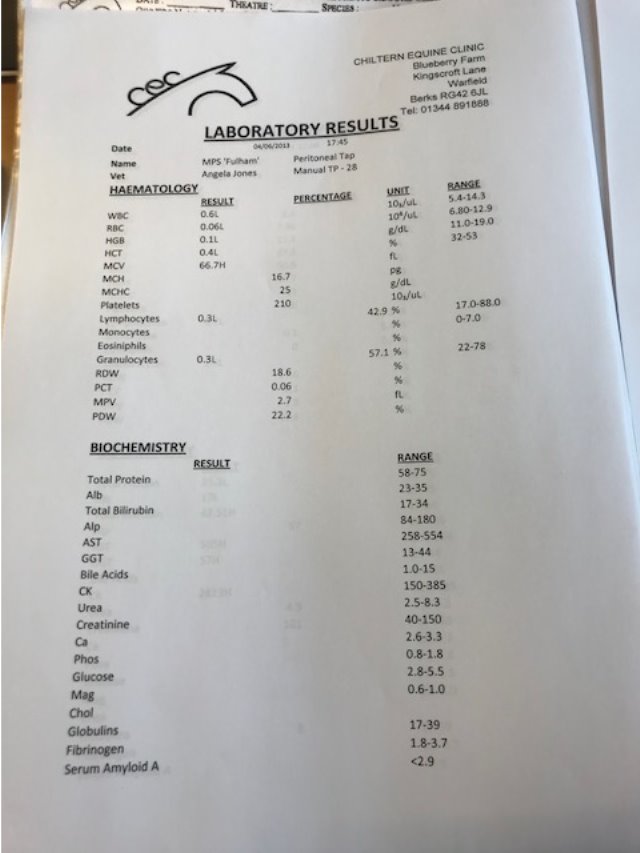
The above case was admitted for emergency exploratory laparotomy following acute onset of severe colic signs, unresponsive to analgesia. Diagnostic testing confirmed the likelihood that a surgical lesion was present.
Diagnostic process: Rectal examinations, abdominal ultrasound and abdominocentesis confirmed the need of surgical intervention and an exploratory laparotomy was required.
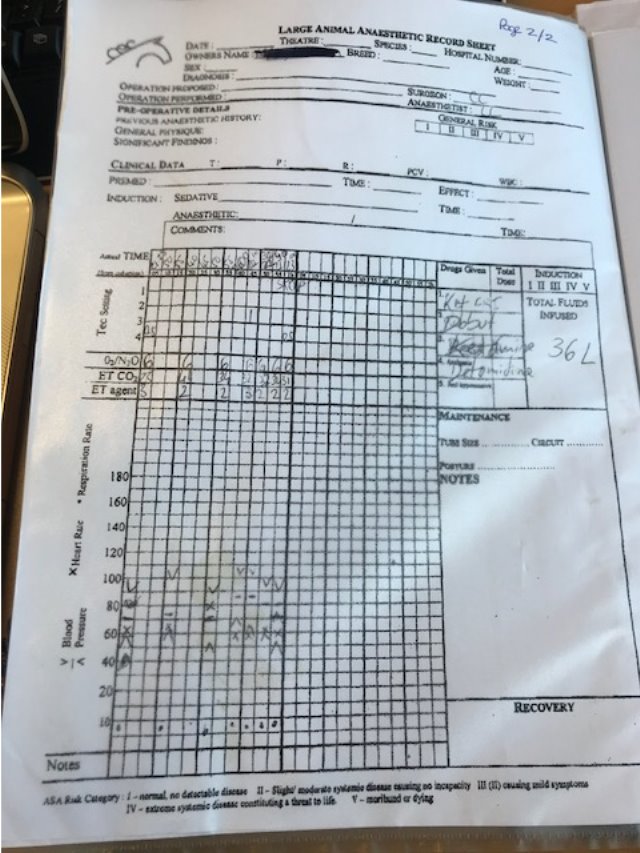
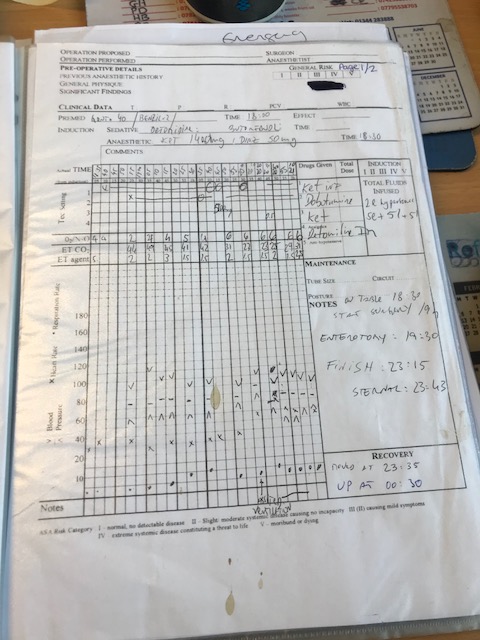
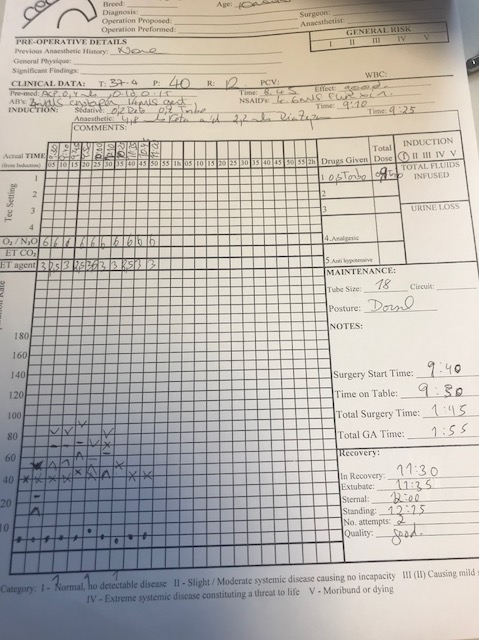
Anaesthetic: (Appendix 1- Anaesthetic record sheet) The above procedure was carried out in dorsal recumbency under general anaesthetic.
Premedication consisted of:
Antibiotics: Gentamycin at a dose rate of 6.6mg/kg and Benzyl Penicillin at a dose rate of 10mg/kg as prophylactic treatment prior to surgery. A prophylactic is a medication, or a treatment designed and used to prevent a disease from occurring (medicinenet, 2011). The use of prophylactic antibiotic therapy was used to prevent the growth of bacteria at the surgical site, this in turn will help reduce the risk of wound breakdown post- surgery. If these drugs are not used pre-surgery then the possibility of infection, wound breakdown and even systemic infection could occur causing damage to the internal system of the animal and endotoxemia. These toxins are generally due to the presence of certain types of bacteria in the horse’s gut that have breached the gut wall and entered the blood stream. If not treated promptly, endotoxemia can lead to shock, laminitis, and death (PetMD, 2017). The non-steroidal anti-inflammatory drug Flunixin Meglumine has anti-endotoxic effects and therefore was used post-operatively in this case.
Induction: Ketamine 2.2mg/kg and Diazepam 0.04mg/kg were given to induce anaesthesia.
Throughout surgery anaesthesia was maintained with oxygen and isoflurane using a large animal circle circuit. A Dobutamine infusion drip was maintained throughout the surgery to support the horses arterial blood pressure (ABP). The patient also received fluid replacement to counteract the loss of fluid during surgery. This also helped minimise the risk of the horse going into hypovolaemic shock. This occurs through significant loss of circulating fluid volume that may happen following haemorrhage or rapid fluid loss through other sites such as gastrointestinal tract (Cooper,B Mullineaux,E Turner L 2011).
Recovery: Romifidine was administered intravenously to allow for safe movement from the surgical table into recovery box, the patient was to ‘free’ recover and did so satisfactorily.
Surgical Procedure: A ventral midline incision was carried out, this revealed a strangulating pedunculated lipoma, as primary diagnosis. Half a metre of severely compromised jejunum was identified, and the stalk of the lipoma was transected. The jejunum was distended with fluid and gas with minimal movement observed (ileus), ‘Ileus is defined as the absence of propulsive aboral movement of gastrointestinal contents, irrespective of its pathophysiology.’ (Cote, N and Koenig J. 2006).
Marked Impaction of the large colon and caecum was present with retroflexion of the pelvic flexure. Prior to jejunal resection and anastomosis a pelvic flexure enterotomy was performed. The subcutaneous layers and the linea alba were closed using absorbable suture material and the skin was closed using skin staples. A bandage stent was placed for recovery where the patient would then be placed in a full belly bandage.
Postoperative treatments and follow up: Intensive post-operative care followed over 72 hours, consisting of hourly nursing checks, regular blood analysis (Appendix 1), ultrasound and rectal re-examinations, hourly reflux of fluid from the stomach via naso-gastric intubation (NGT), abdominal bandaging, antibiotic therapy, NSAIDs, Intravenous fluid therapy at a rate of:
The fluid deficit was calculated at 10% dehydration. The calculated requirements were as follows:
- 650kg x 10% dehydration x 10 =65000mls
- 65000mls / 24 hours = 2708mls per hour
- 2708mls / 60 minutes = 45 mls per minute
- 45mls x 20 (drip factor) = 900 drops per minute / 60 seconds = 15 drops per second to replace the deficit.
The patient was then maintained on 50ml/kg/day.
- 650kg x 50ml = 32500mls per day.
- 32500 / 24hours = 1354mls per hour.
- 1354mls / 60mins = 22mls per min.
- 22mls / 60 seconds = 0.36mls per second
- 0.36mls x 20 (drip factor) = 7.2 drops per second.
.
Although initial good improvement was observed, ileus was present throughout the post-operative period. 4 days post-surgery a marked deterioration of vital signs and an increase in pain were observed and after discussions with the owner a decision for euthanasia was made due to poor prognosis for full recovery of this case. The patient was euthanased on humane grounds.
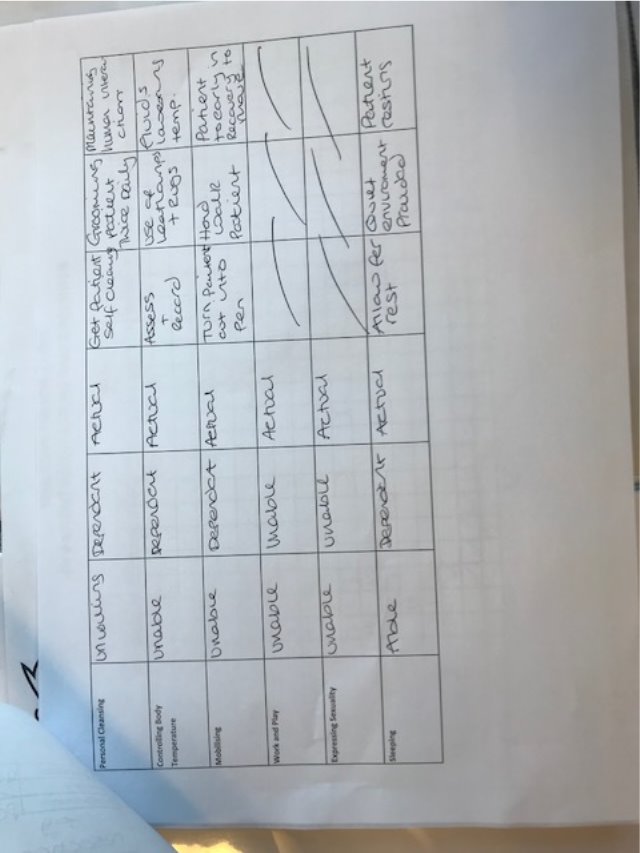
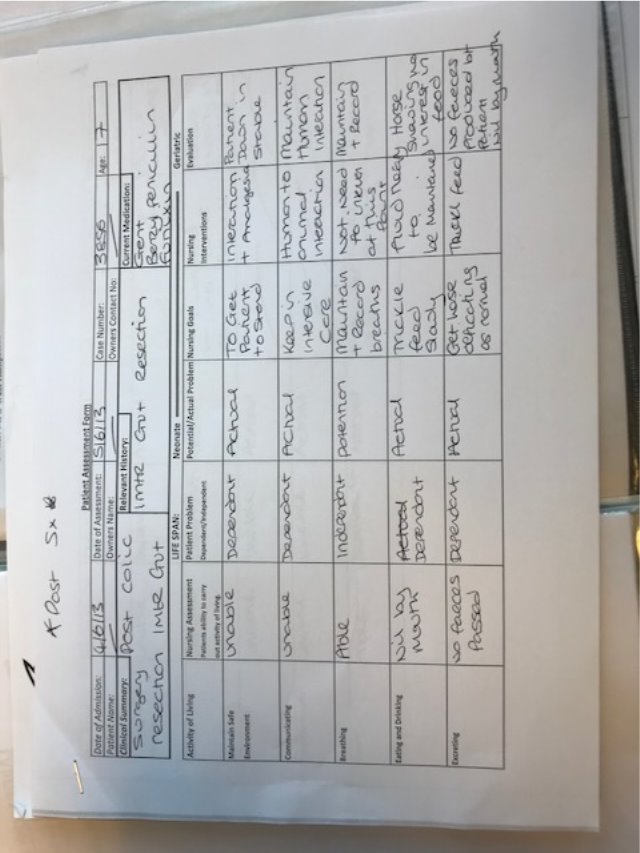
Nursing Needs:
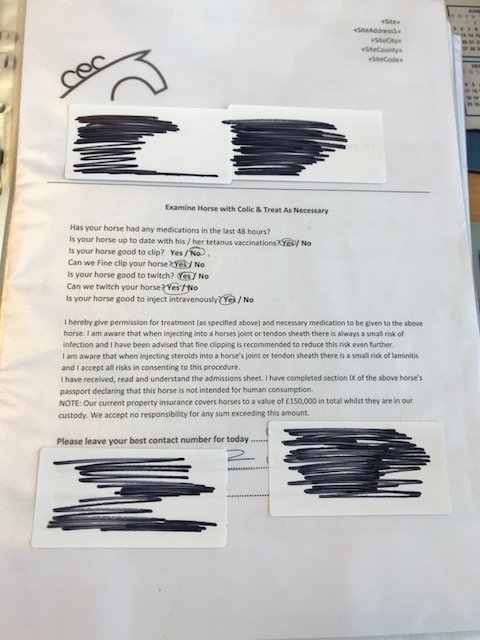
On admission to the hospital a vital role of the veterinary nurse upon admittance is the handover from the owner. It is fundamental to find out what is ‘normal’ for the patient as this can be monitored and recorded if any differences are observed and any information that could be relevant to the surgery or recovery of the patient. Contact information for the owners, especially in such an intensive case as this is an important part of any consent and handover from an owner, this is so the owner can be kept up to date with the patients’ condition.
Since July 2009 the law has required horses, ponies and donkeys to have a passport, registered in your ownership. The purpose of the law is to ensure animals treated with medicines cannot enter the food chain. The penalty is up to £5000 for any animal that is found being transported without a passport. On admittance to the clinic the passport should be checked to ensure that section IX has been signed by the owner and a veterinary representative. Upon signature of this section means that the animal will no longer be able to enter the human food chain. Certain drugs are not such as ‘Phenylbutazone’ do not permit an animal to enter the food chain. The veterinary medicines directorate published a pharmacologically active substances list and their classification called ‘Commission Regulations 37/2010’. This list tells you what is permitted within the food chain and how long the active substance is residual within the body of the animal. ‘If any substance which is not on this list or is not listed in table one of 37/2010, such as phenylbutazone, is administered to an animal, that animal must be permanently excluded from the food chain and the declaration in the passport signed by either the horse owner, its keeper or the vet’ (Veterinary Medicines Directorate. 2015).
Obtaining consent to any procedure whether written, verbal or signed consent is vital. written consent is most preferable within a court of law only, however only if it has been verbally explained to the owner. As all anaesthesia carries considerable risk to patients it is imperative that the client has had all risks explained with the surgery itself and the aneasthetic thus allowing the opportunity to ask questions in relation to the procedure. This time also allows for the surgical protocol to be reiterated to the client such as shoe removal and starving. Informed consent means that the client has been given all the information in terms of what the treatment involves, including the benefits and risks, whether there are reasonable alternative treatments, and what will happen if treatment doesn’t go ahead. This is best achieved face-to-face with the client.
Prior to any elective surgery it is important to starve the patient especially in equine surgery. Any food content within the stomach could compromise breathing when the animal is in dorsal or lateral recumbency which in turn carries the risk of aspiration of food. As this was an emergency case it was not possible to starve the horse and the patient had to go to surgery with the impaction and stomach of food. The equine stomach is large and therefore when full can put pressure on the lungs, which in turn can make it harder for the patient to breathe independently under anaesthesia. The risk of food or acid refluxing up the oesophagus and being aspirated into the lungs is present. This could cause airway obstruction or aspiration pneumonia and these added risks should be mentioned to the client on admission.
Post-Surgery Nursing Needs-
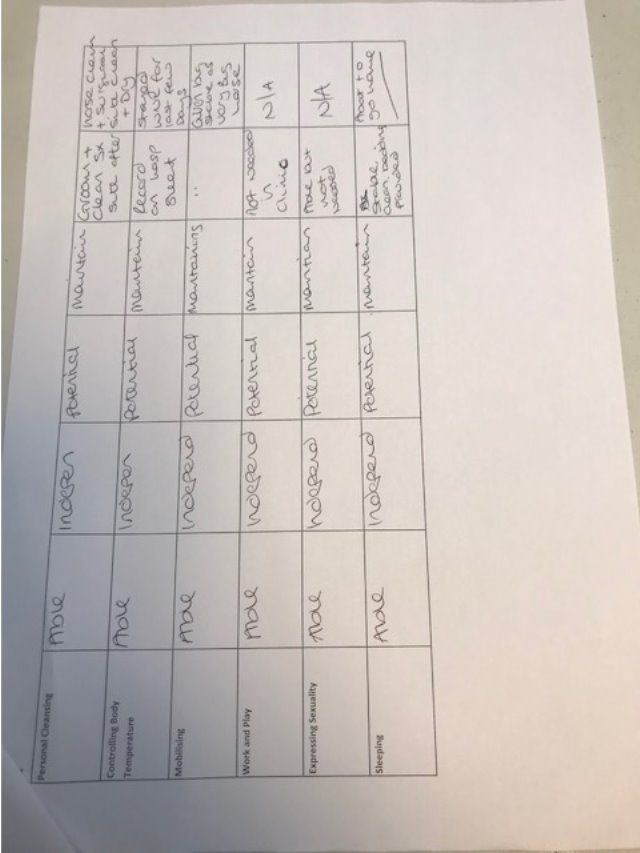
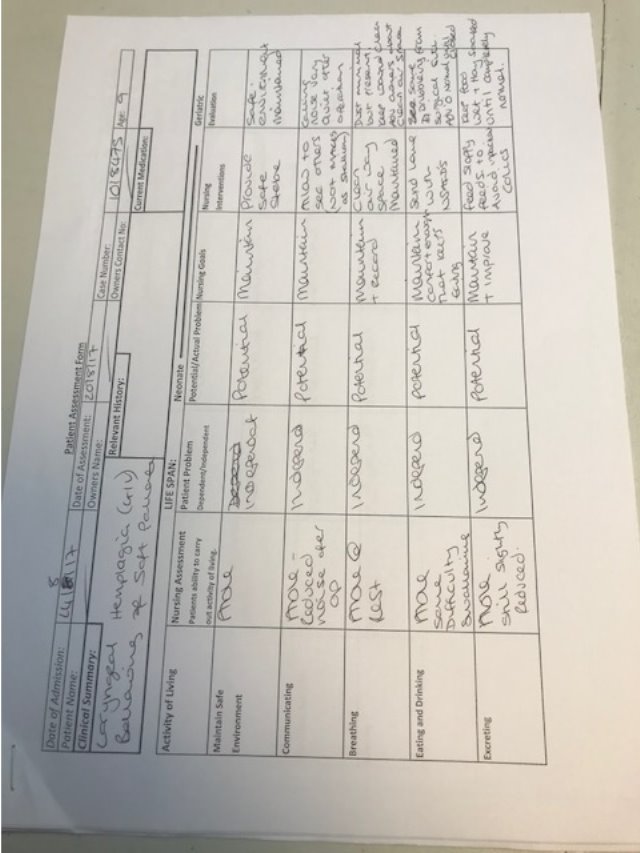
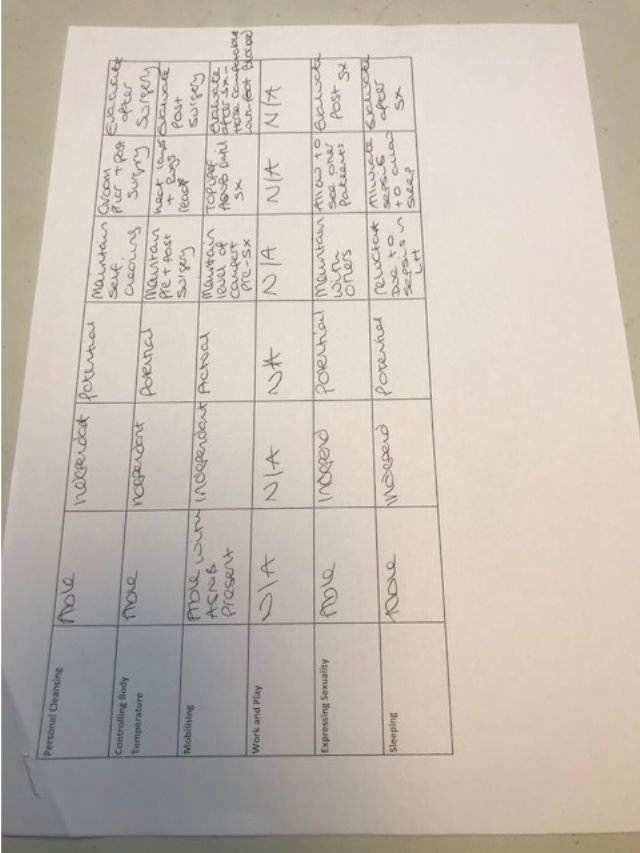
Upon admission of the patient a Nursing Care Plan (NCP) was implemented (Appendix 1 page 21), this demonstrated that the patient was very much dependent on the veterinary team prior to surgery. This made it vitally important that the handover from the operating theatre was clear and concise. As much information should be acquired as possible such as;
- Length of surgery- first cut to dressing placement.
- Timings and doses of drug administrations during surgery.
- Quality of anaesthesia and induction.
- Recovery- timings, quality, drugs administered and any complications.
- Prognosis- Post-surgery and overall.
- Post-operative plan- IV fluids, medications, dressing changes, observation times, refluxing, catheter status and care, wound care and food, water.
- Patient and client information- contact details, temperament of patient.
- Clinician in charge – who to report to should anything change or deteriorate with patient.
All this information will aid the nursing team that will be carrying on the post-operative treatment of the patient thus maximizing efficiency for the best possible recovery of the patient.
The patientwas placed on IV fluids to counter balance the loss of fluids during surgery, a constant rate of Hartmanns Isolec-Combi (Isotonic and Hypertonic) to expand the circulating blood volume which will also help with stopping the patient going into hypovolemic shock post-surgery. Recognition of a patient that is suffering from post-operative shock can include the horse to be tachycardic, a weak and barely palpable pulse, pale and tacky mucous membranes, weakness, unsteadiness and cold extremities.
Nursing Treatments:
This patient required intensive nursing care. This included hourly observations, regular blood and hydration analysis, IV Catheter placement and care, intravenous fluid therapy, medications that consisted of:
- Benzyl penicillin
- Gentamycin
- Flunixin Meglumine
- Metoclopramide
Clean bedding was provided by the yard staff. Grooming and other human interactions were provided for the patient post-surgery, in an aid to retract the horses mind away from any pain and provide normality as best possible.
Discussion:
Although the patient did not show vast improvement after surgical intervention, it was necessary for the surgery to have been performed. The NCP’s that were followed before and after surgery did not alter in the few days that the patient survived after surgery. If the prognosis had been better and the patient had showed improvement the NCP’s could have reflected this. This case provides the knowledge that intensive nursing is extensive with lots to think about. As the patients’ intestines remained in ileus for the post-operative period, further complications such as necrosis of gut would be likely to arise. In this case all possible treatments were given to this patient, unfortunately the pathology meant that these did not offer a favorable outcome and euthanasia was required.
Case 2 – Planned Minor Surgery.
Patient Information and Identifier:
Species: Equine
Breed: Pony
Age: 1 years
Weight: 211kg/ 11hh
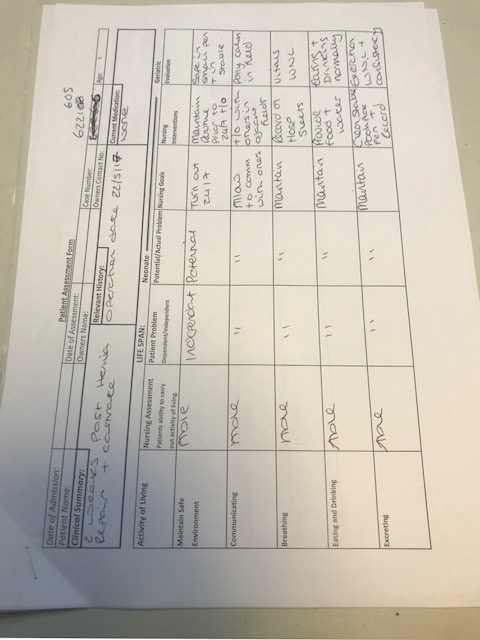
Case Identifier: 6221605
Veterinary Diagnosis and treatment:
The minor surgical case I will be discussing is an umbilical hernia repair. The patient was examined on the yard to establish the size of the hernia, it was deemed too large to band so surgical intervention was advised.
Diagnostic process: Digital palpation of the hernia and Ultrasonography.
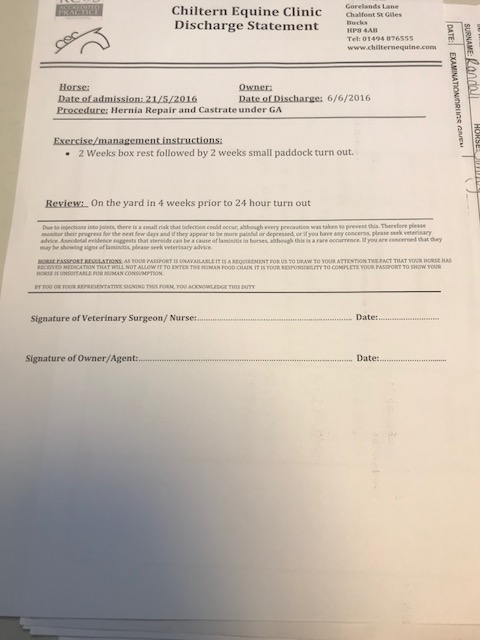
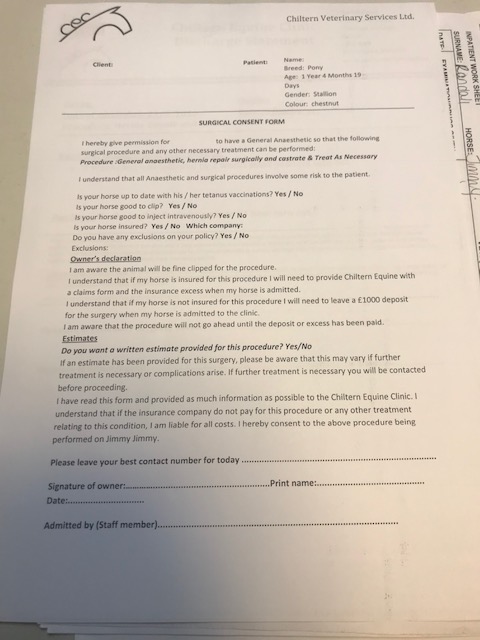
Anaesthetic: (See appendix 2)
Premedication included:
- 0.4mls Acepramazine Maleate
- 0.1mls Detomidine
- 0.1mls Butorphanol
Prophylactic Antibiotics:
- Gentamycin at a dose of 6.6mg/kg
- Benzyl Penicillin at a dose of 10mg/kg
Non-steroidal Anti-inflammatory Drugs (NSAID’s):
- Flunixin Meglumine at a dose of 1.1mgs/kg
Induction agents:
- Ketamine at as dose of 2.2mg/kg
- Diazepam at a dose of 0.04mg/kg
Maintenance of Anaesthesia:
- Isoflurane inhalation agent
Surgical procedure:
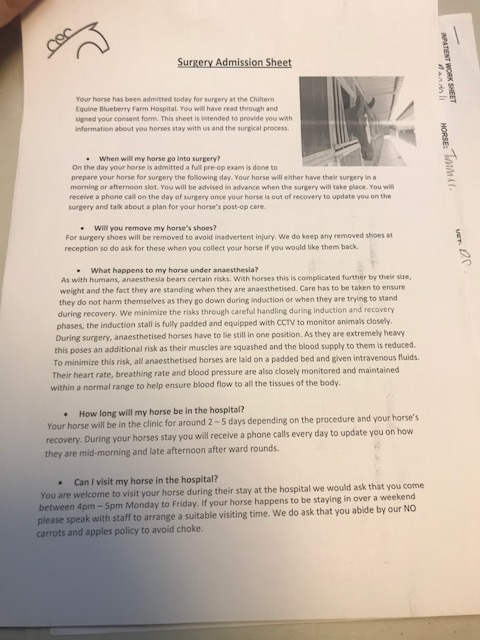
The Patient was admitted to the hospital 24 hours prior to the surgical procedure to allow the patient to settle and so starvation could happen. Starvation for 12 hours prior to anaesthesia will reduce the volume of the gastrointestinal system. ‘The pressure imposed by the weight of a full abdomen compromises diaphragmatic movement and contributes to hyperventilation, particularly when the horse is positioned in dorsal recumbency’ (Coumbe, 2001). It is not necessary to remove water as this is easily absorbed through the stomach and deprivation could cause dehydration.
Consent from the owner was obtained on admission (Appendix 2), this involved the surgeon explaining the procedure to the client, allowing for questions to be asked. Whilst the surgeon was explaining to the client, the passport was checked for:
- Vaccination status.
- Section IX was signed out of the food chain.
- That the patient matched the passport. This was checked by scanning the microchip.
The visiting hours and post-operative updates were explained to the client and the client completed the consent form thus allowing for the procedure to go ahead. This is called written and informed consent.
The Patient was admitted to the stable yard where it could continue a normal feeding routine until 10pm that evening. On the morning of surgery, the patient was thoroughly groomed and a tail bandage applied to reduce the risk of contamination in the theatre. The mouth was washed out to avoid any food debris being forced down the trachea during intubation. The author established with the surgeon that the patient was being positioned in dorsal recumbency and therefore the left jugular vein was chosen and prepared for catheter placement. The area was clipped with a fine surgical blade and scrubbed with a dilute chlorohexidine scrub (1:10) and alcohol swab to clean off the residual detergent and grease. Once the area was clean a catheter was placed ready for surgery.
A hernia describes a defect in a structure through which an organ or part of an organ can pass or potentially become trapped (Coumbe, 2001). This patient underwent the repair of an external umbilical hernia, this is most commonly observed in younger horses and spontaneous resolution is common but unfortunately this was not the case for this horse. After the induction of anaesthesia, the patient was transported via hoist to the surgical table and placed in dorsal recumbency on the surgical table. The surgical site was identified around the abdominal hernia and the area was clipped using a well maintained, lubricated, clean pair of clippers and a fine surgical blade. A 40x40cm region was clipped around this and scrubbed using dilute chlorohexidine at a dilution of 1:10. The site was scrubbed beginning at the proposed incision site in a circular motion working out to the periphery of the clipped area. Gloves were worn to prevent contamination from any bacteria on the hands. Once the edge was reached the swab was discarded of and a fresh one taken. Once the swabs were coming away clean, an alcohol spray was used to remove detergent and grease and a dry swab was wiped over to assess the efficiency of the scrub. Had there been any further discolouration of the swab the scrubbing procedure would have been repeated until clean. The hernia was repaired by manipulating the intestine back through the inguinal ring and suturing the abdominal wall together. The skin was closed with absorbable suture material and a stent was placed over the incision for recovery.
Post-Surgery-
Following surgery, a swelling was noted at the left side of the surgical site. As the clinical exam was normal, no pyrexia or haemorrhage was noted and the horse remained bright, an abdominal support bandage was placed. Once the dressing was in place the patient was taken to the holding box, the heat lamps were put on as the patient was not used to wearing rugs due to age, a wrap of Elastoplast was placed around the neck to cover the catheter to minimise patient interference and to keep the catheter in place. This was checked every few hours to make sure it was not too tight on the neck.
Upon discharge of the patient it was advised that he received a small amount of sedation to travel home, this was because the patient was inexperienced on the horse box and was to help keep him calm when in transit.
Nursing needs:
Post-operative pain management included the administration of Flunixin Meglumine twice daily and monitoring at the time of clinical examinations. Vital signs were monitored closely for any changes as an increase in temperature, respiration rate and heart rate can all be indications of pain as well as behavioural changes, therefore handover between nurse and owner are vital prior to surgery, to ascertain what is normal for this patient.
Omeprazole was administered at ¼ syringe daily 30 minutes prior to feeding as a prophylactic action to reduce the risk of stress and NSAIDS’s related gastric ulceration during the stay in the hospital. ‘The ability of non-steroidal anti-inflammatory drugs (NSAIDs) to cause gastrointestinal ulcers is well established in equine practice’ (Succeed-Veterinary Centre, 2017).
An abdominal support bandage was placed and monitored for any excessive exudate. The patient received intravenous antibiotic therapy for 72 hours and then continued a course of oral antibiotics and NSAID’s.
Discussion:
The above case would be classed as a ‘semi-elective’ surgery, this means that the surgery needs to be done as it poses a risk to the animal but is not classed as an emergency. Had the hernia been smaller then the potential to band the hernia rather than surgery could have been an option. The surgery and recovery period for this case was relatively uneventful as shown in the NCP’s. The nursing needs in this elective case were not as intense as the emergency abdominal surgery above. All entrance into the abdominal cavity is classed as major surgery due to the weight of the organs in the abdomen and a weakening of the abdominal wall could cause a rupture which is a documented risk of this surgery. Post-operative infections can occur with any wound even if great care was taken before, during and after surgery. Complications with healing within this case can arise from many things, such as wound contamination from the stable, the patient getting up and down could also damage the surgical site. Having an immunocompromised patient can cause great complications and delay healing, factors that can alter a horse’s immune system include:
- Age (neonatal and very old horses)
- Antibody deficiency if foals suffer failure of passive transfer of maternal antibodies.
- Malnutrition.
- Physical or psychological stress, including training, transport, social isolation, hospitalisation.
- Diseases such as Cushing’s disease.
- Corticosteroid administration.
- Sepsis (blood infection).
These factors could be witnessed, assessed and acted upon if present on the care plans taken during hospitalisation.
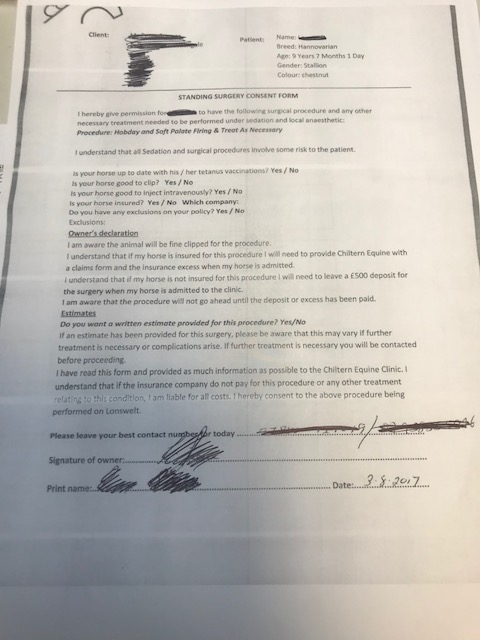
Case 3- Standing surgery, head and neck
Patient Information and Identifier:
Species: Equine
Breed: Hannoverian Stallion
Age: 9 years
Weight: 678kg/ 17hh
Case Identifier: 1018475
Veterinary Diagnosis:
Laryngeal Hemiplegia and bellowing of the soft palate.
Diagnostics included-
- Resting and Dynamic Endoscopy.
Prior to admission it was known that the owner would not be bringing the horse himself to the clinic, but the rider would be. The author checked with the owner via telephone that the agent had permission to sign the consent form for the surgery, contact numbers for both the owner and the trainer, whom plays an active role in the wellbeing of the patient, were left as communication points for the horse. Previous relevant history was obtained from the rider who had observed first-hand the issues, this is especially important as the author was able to ask if anything had changed since initial diagnosis that could influence the surgery (i.e. patients’ health or any deterioration). An estimate was provided for the dynamic endoscopy and it was asked if an estimate was required for the Surgery. The Owner declined this service verbally. Estimates play a key role in informed consent to any procedure. If requested and not given prior to it happening, this may then not be classed as full ‘informed consent’. In human and veterinary medicine the term ‘informed consent’ is often used; however in law the term ‘consent’ or ‘consent to treatment’ is used, as ‘informed’ is an essential component of valid consent and there cannot be valid consent without information. (Pullen, S and Gray, C,2006)
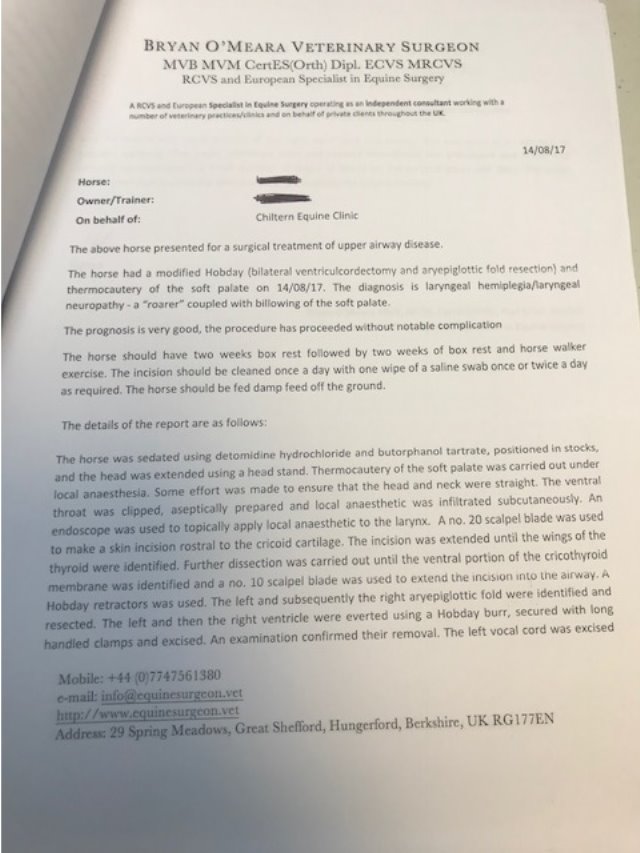
Anaesthetic and Surgical Procedure:
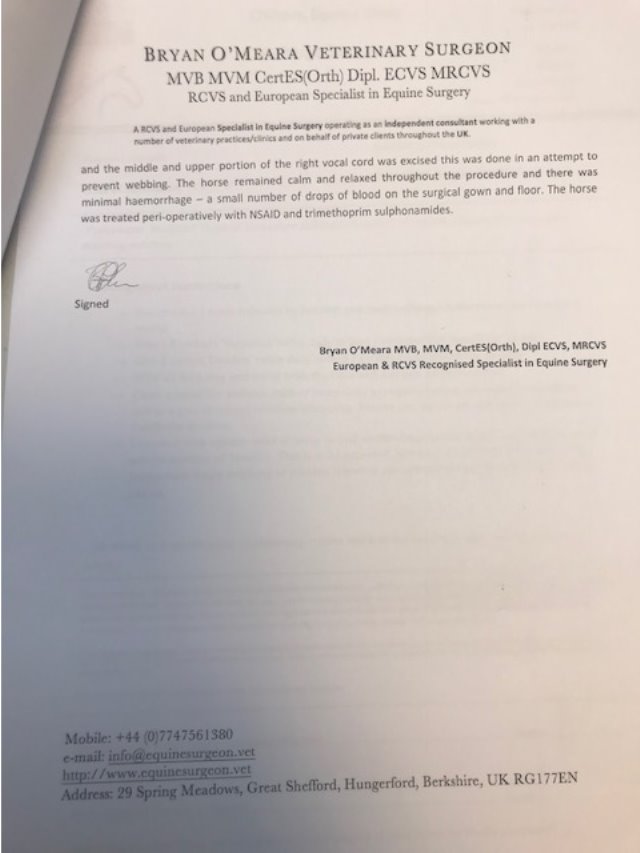
The horse was sedated using a continuous rate infusion of detomidine and butorphanol and thermocautery of the soft palate was carried out under local anaesthesia. The ventral throat was clipped, aseptically prepared and local anaesthetic was injected subcutaneously. An endoscope was used to visualize and topically apply local anaesthetic to the larynx. A scalpel blade was used to make a skin incision rostral to the cricoid cartilage then the incision was extended until the thyroid was visualised. The epiglottic folds were identified and resected. The left and right ventricle were turned using a Hobday burr, secured with long handled clamps and excised. The surgical incision was left to close by second intention to encourage the drainage of the wound. This was to minimize any discharge from being aspirated or swallowed.
Post-surgery:
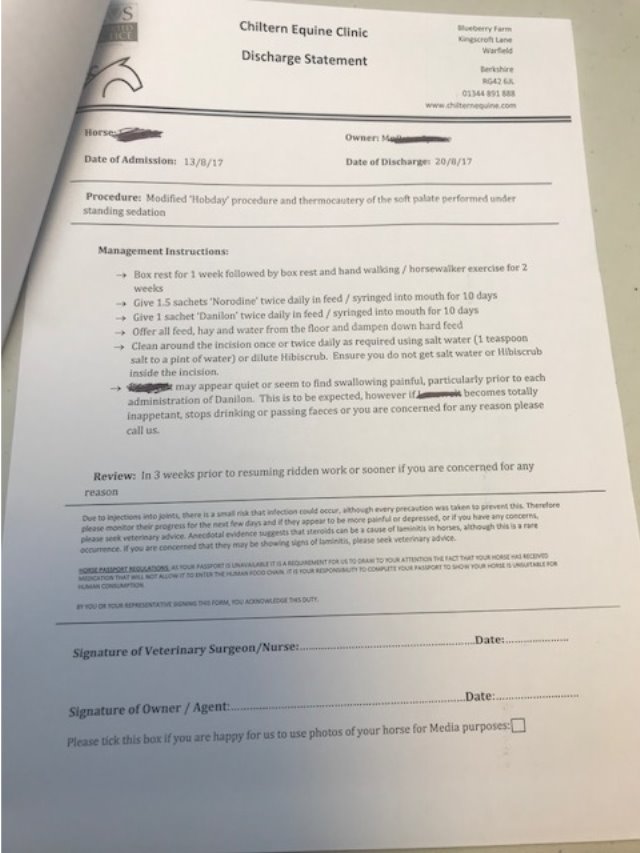
Post-operative intravenous Analgesia (Flunixin Meglumine at a dose rate of 1.1mg/kg ) was administered twice a day and antibiotics (Gentamycin 6.6mg/kg and Benzyl Penicillin 10mg/kg) were administered for 3 days post-surgery. As the patient was reluctant to eat much in the postoperative period the surgeon recommended the use of oral omeprazole to reduce the risk of gastric ulceration. Hand over from the surgical team consisted of box rest, maintaining a clean airway environment by soaking of feeds, placing the horse on dust free bedding, removing the horse from the stable when mucking/skipping out, cleaning the surgical site twice daily with one wipe of a sterile saline swab, feeding wet feeds, soaked hay and for all feed to be fed from the ground to encourage drainage from the surgical site. Initially fibrous feeds were fed and the patient was reluctant to eat this as it was possibly uncomfortable to swallow. This was noted and changed to a sloppy wet bran and pony cube feed with hand pick of grass and eaten straight away. All vitals remained normal at this point and urine and faecal output was normal. The following day the patient became pyrexic. Bloods were taken to assess the white blood cell counts to establish if the pyrexia was related to infection. The white blood cell count was within normal limits and therefore not indicative of an infection. As flunixin is a potent analgesic and antipyretic it was administered to make the patient more comfortable. The patient was due to be discharged however it was recommended to the client that he remained hospitalised. The horse stayed in overnight and remained inappetant with reduced faecal output. Oral fluids were administered to aid rehydration and a repeated dose of flunixin. The following day the horses’ demeanour, appetite and clinical exam including the white cell count returned to normal. Therefore, the patient was discharged on oral medications (Appendix 3).
Discharge:
On discharge the patient was to go home on oral medications and this was advised on how best administered. Box rest for 1 week then a further 2 weeks box rest with hand walking or horse walker was recommended and a likely return to resuming ridden exercise was provided. When the patient was discharged clean air management was advised initially when the horse arrived home as the author knew that the patient wold be returning to a closed indoor dusty barn, it was recommended the horse was moved into a different stable preferably outside the barn to ensure this could be done. Contamination to the wound can occur from dust entering the surgical site and the lungs as this was now a clear passage after removal of the epiglottic folds. It was reiterated that all feed should be fed from the ground verbally and written on the discharge It was recommended to monitor the patient for the following signs: total inappetence, dysphagia and reduced faecal output. It was advised that they contact the hospital should these signs be observed. (Appendix 3 page 34).
Discussion:
The longer the procedure takes the more prolonged the sedated period is. This increases the risk of colic by slowing down gut motility which occurred in this case. A standing surgical procedure presents risks because the horse is conscious and if they move this will prolong the surgical time. Post-operative nursing in relation to this case consisted of keeping the horse pain under control enough that he keeps eating and drinking, keeping the surgical site free of dirt and debris and maintaining the clean air environment.
Case 4-
Patient Information and Identifier:
Species: Equine
Breed: Irish Sport Horse
Age: 13 years
Weight: 431kg/ 16hh
Case Identifier: 6222724
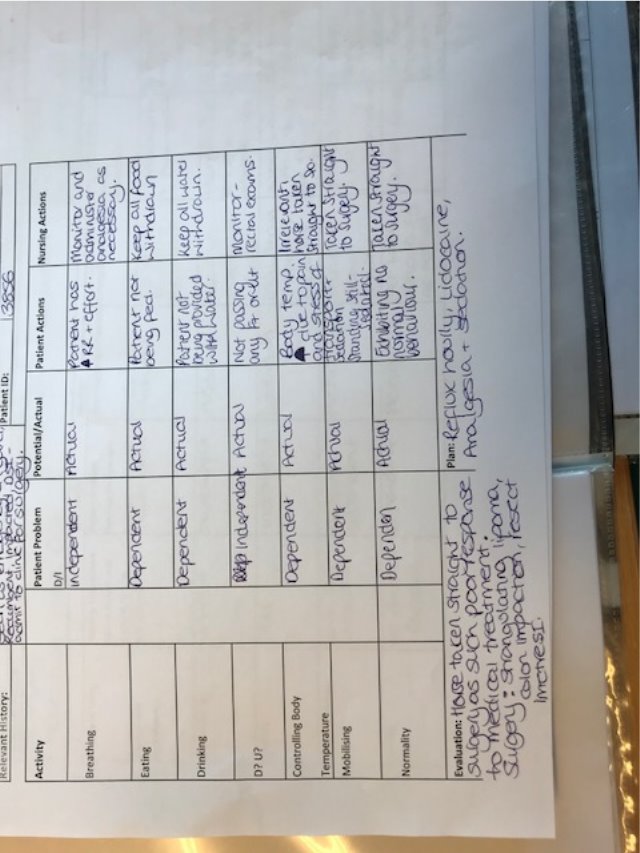
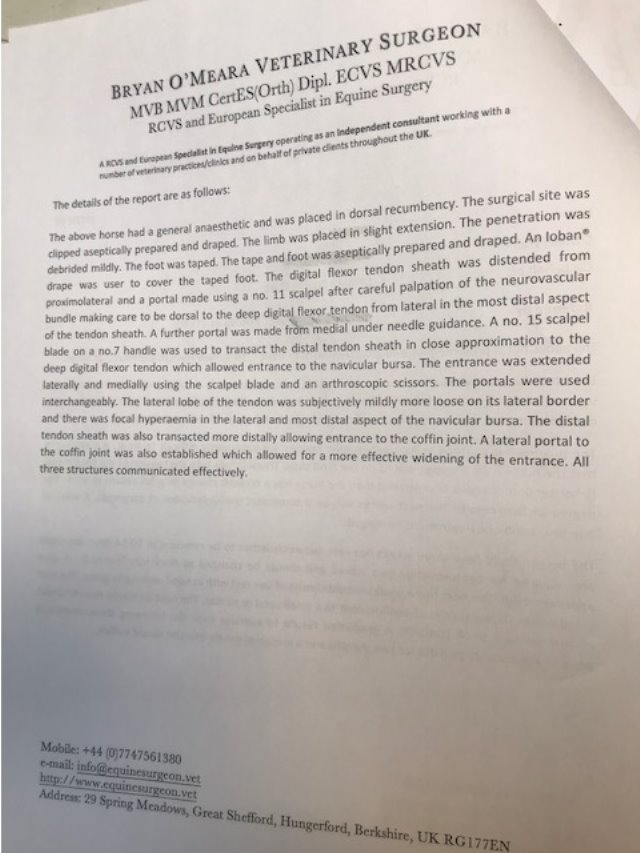
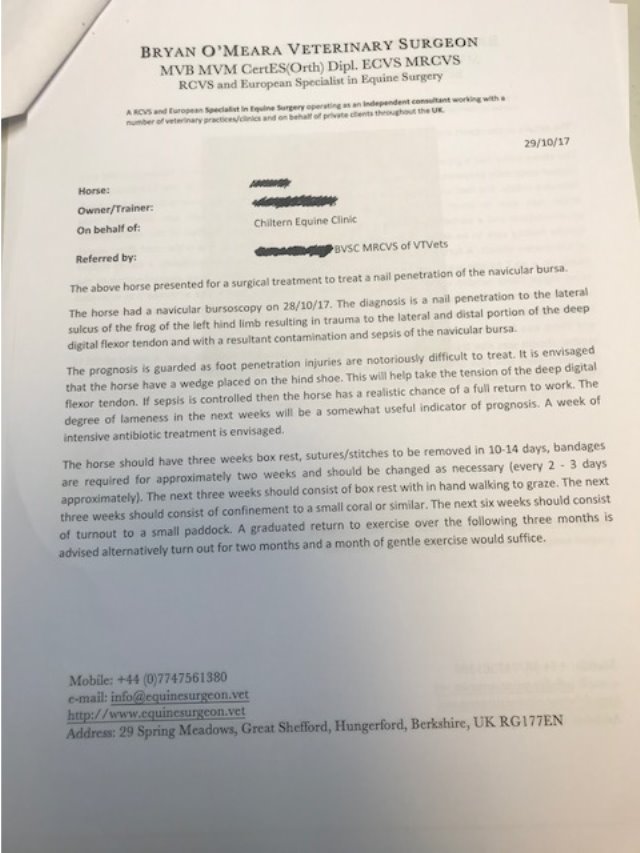
Veterinary Diagnosis and treatment:
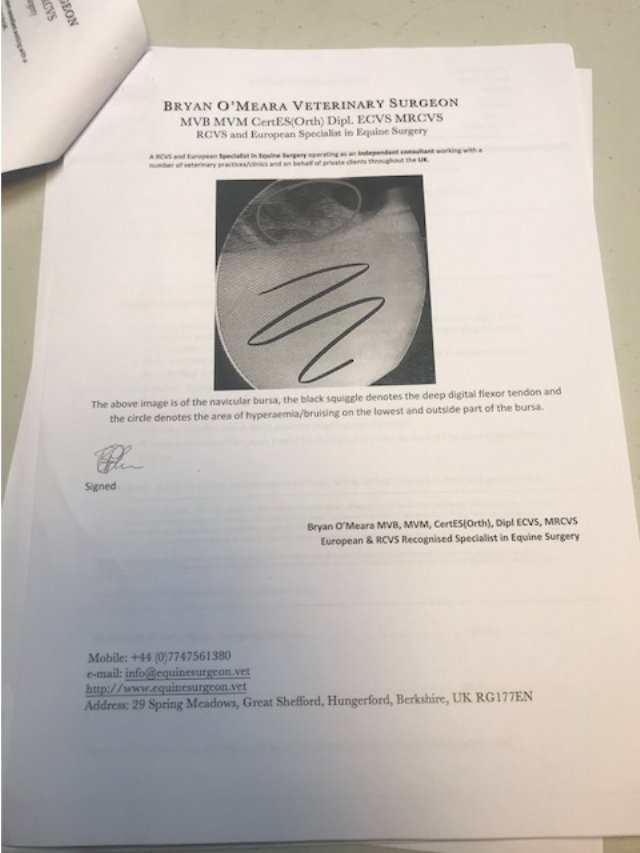
Nail penetration to the sole of the foot causing septic Navicular Bursitis.
Diagnostic Process:
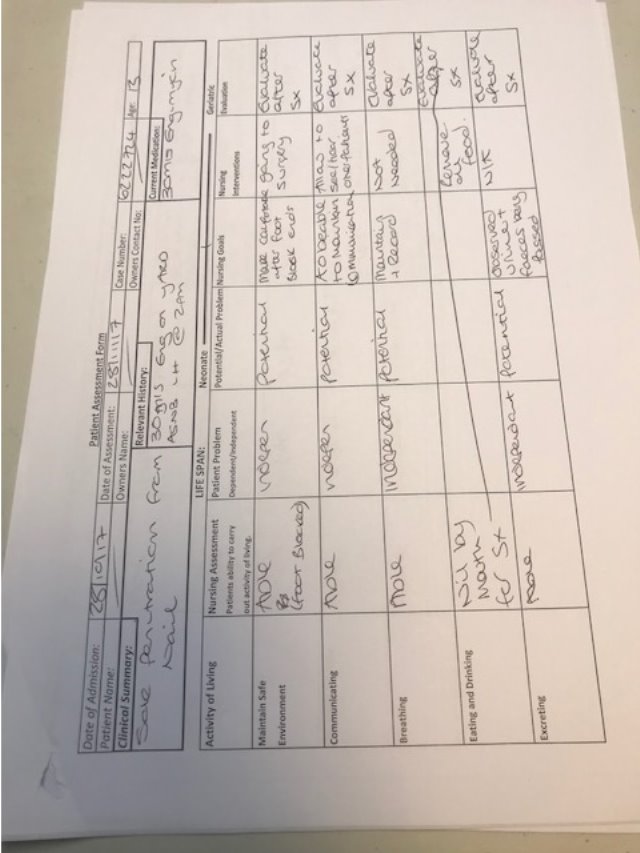
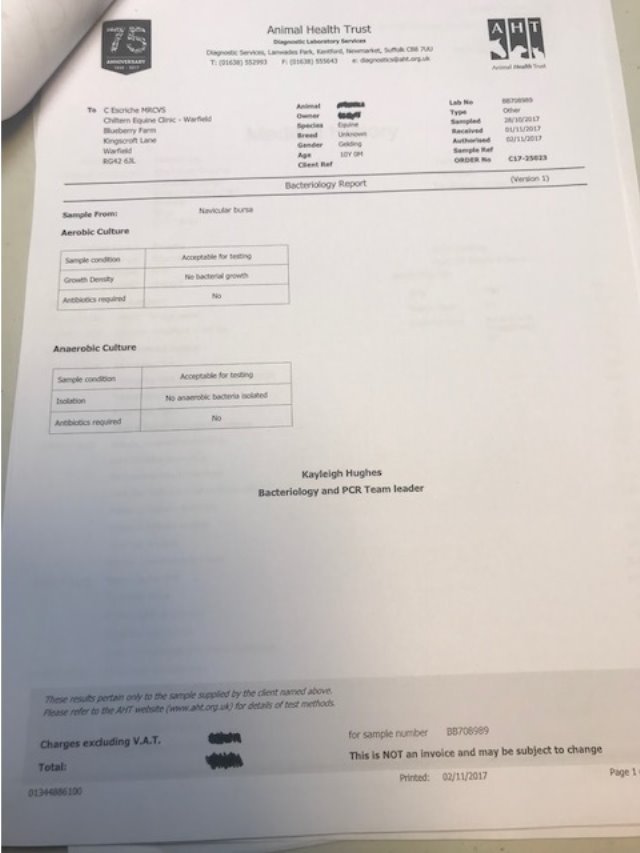
The previous history was taken from the owner and the referring vet including vaccination status, location of the nail and the approximate depth of penetration. Consent forms (Appendix 4) were completed for an examination and for surgery. The foot was examined and a sterile probe was inserted to ascertain the depth of the penetration. The foot was clipped in preparation for a tap of the navicular bursa, the area where the needle would be entering was identified and the area scrubbed with chlorhexidine. Then the area was wiped with surgical spirit to remove excess dirt, grease and detergent. The tap of the navicular bursa and a contrast study was performed. Radiographs were taken to confirm that contrast had dispersed out of the bursa, indicating a breach of the navicular bursa and the sample was analysed which confirmed a septic process. The results showed a white blood cell count of 552 x 10⁹ and a total protein of 6.8g/dl. This indicated a Navicular Bursoscopy was necessary to flush out the infected debris. A sample of the Fluid from the bursa was sent to an external laboratory for a culture and sensitivity test to be run (Appendix 4).
Nursing needs prior to surgery-
As this was a referral case, it was important to speak the referring vet to be able to find out what drugs were administered on the yard prior to being sent to the hospital. The patient was then weighed as drug doses are calculated on the basis of body weight (Coombe, 2001). The catheter was site clipped, scrubbed and placed in the left jugular vein as the horse was being positioned in dorsal recumbency. All shoes were removed prior to surgery, the clenches were raised using a buffer and hammer, using shoe pullers the shoes were removed. The sole of each foot was pared back and cleaned with a hoof knife and bucket of soapy water. Shoes are removed before the horse enters induction to reduce contamination to the surgical facilities, avoid injury to horse and personnel and to reduce damage caused to the induction area. The patient was groomed and mouth cleansed, further clipping of the surgical site was performed prior to induction.
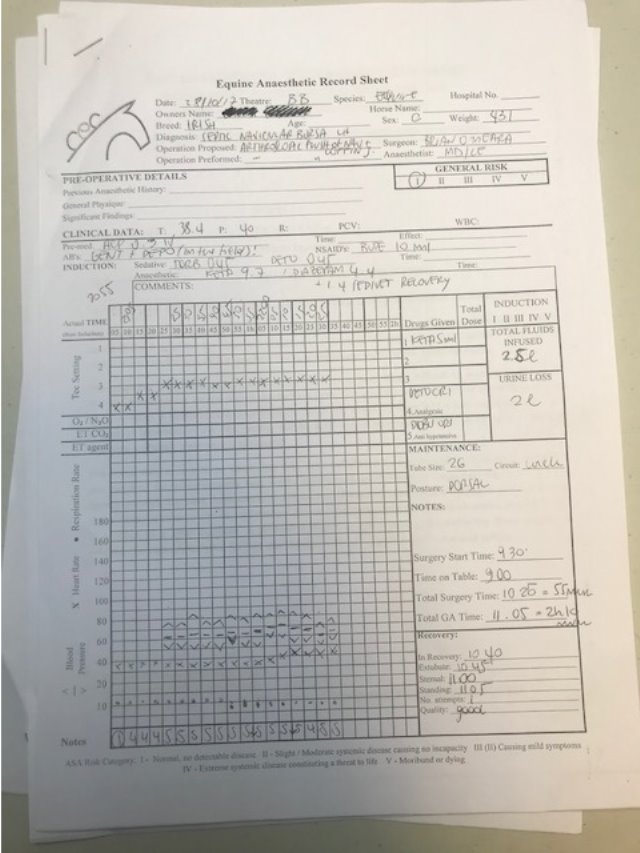
Anaesthetic:
Premedication consisted of
- Acepromazine maleate
- Gentamycin
- Benzylpenicillin
- Phenylbutazone
Induction agents:
- Ketamine
- Diazepam
Maintenance:
- Isoflurane (inhalation agent alongside oxygen)
Recovery:
- Romifidine
Surgery:
A Navicular Bursoscopy was performed. The diagnosis was a nail penetration to the lateral sulcus of the frog of the left hind limb, resulting in trauma to the lateral and distal portion of the deep digital flexor tendon, visible on the camera inserted during the surgery. Resultant contamination and sepsis of the navicular bursa was flushed out with sterile saline and the incision portals closed with non-absorbable Ethilon suture and a half limb Robert Jones bandage applied to stabilise the limb and hold the dressing in place. The dressing consisted of
- Primary layer- sterile dressing layer.
- Secondary layer- padding layer (including orthopaedic padding and cotton wool).
- Tertiary layer- conforming bandage.
- Adhesive layer.
Layers 2 and 3 should be repeated with even pressure down the limb at least 2 times. The bandage should be changed every 2-3 days but if any strikethrough (exudate) is noted beforehand or the dressing is wet or soiled then it should be changed sooner. Some ways to stop patient interference to the bandage such as deterrent sprays or anti-cribbing solution to make the outer layer foul tasting, these are usually enough to stop but if necessary collars and cross tying can be used.
Post-operative nursing and treatment:
The patient recovered from anaesthesia well and once safe to walk was moved back to a clean stable containing a shavings bed. A bran mash was provided 30 minutes after returning from recovery and a trickle feeding regime was initiated until the following morning. The next day the patient was assessed for comfort prior to administration of analgesia, this was withheld to ascertain the level of lameness post-surgery, a mild degree of lameness was evident, which was to be expected at this point. No pyrexia was noted and therefore analgesics were administered. It was noted that the patient had been inappetant overnight and had only passed minimal amounts of dark, hard faeces. After discussion with the clinician in-charge of the case the author assisted with administering 8ltrs of water and electrolytes via NGT and a trickle feed regime was maintained to avoid an impaction colic happening. The hole the nail penetrated was re-opened on the sole of the foot with a hoof knife, no pus was evident, the foot was hot tubbed and then another half limb Robert Jones applied with an integrated poultice on the foot. A re-tap of the navicular bursa was analysed 4 days after surgery this revealed a marked decrease in infection (WBC-7.1 10⁹/L and TP: 25g/l). Intravenous therapy was maintained for 5 days then the patient was switched to oral medication. The sutures that were used as closures of the portals would need to be removed 2 weeks post-surgery as a minimum, this time is needed to ensure that healing is complete. When wounds, surgical or non-surgical, require drainage the use of a Penrose drain would be advisable. These are used to encourage drainage to a site and provide a route for exudate to drain out. It should be dealt with in an aseptic technique with the animal being maintained on anti-biotics. The drain is anchored in the wound by a suture then the other end of the drain leaves to wound at the lowest point so the exudate is released as the gravity pulls it down. After 3-5 days the drain should be removed and the wound can then begin to granulate at the space the drain filled.
Discharge and discussion:
When planning for discharging of a patient it’s important to be actively involved in the case where possible. The author in this case was present from diagnosis, surgery and discharge. If given the responsibility of returning a patient to a client it is important to know the full facts about the case and procedure so that any client questions can be answered (Cooper, B, et al, 2011). The best way to discharge a patient is to break the discharge down into sections and not to bombard the client with information this is called ‘’Chunking and Checking’’, this means a chunk of information in the discharge is given to the client and the nurse then checks that it is understood prior to moving on ‘if you give information in small chunks and give patients ample opportunity to contribute, they will respond with clear signals about both the amount and type of information they still require’ (Unknown ,2011). In this case the initial part of the discharge was to arrange a farrier to fit a shoe with a wedge, the option was given for the farriers’ number to be given directly to the clinic and direct liaison could happen. Further instructions regarding the patients’ rehabilitation were then given and questions were allowed for to make sure all was clear. Medications were next and the boxes of medications were shown and their dosages and routes of administration demonstrated and explained. Failure of the surgery may result in further diagnostic testing, and these were listed on the discharge, such as: Magnetic Resonance Imaging (MRI). A review was scheduled for 12 weeks post discharge, the client was also explained should she have any concerns the practice was on call 24 hours a day to give advice or come and see the patient at home (Appendix 4). The daily nursing care plans written while the patient was hospitalised means even somebody not actively involved in the case would could discharge the patient and have the correct information and insight to answer the clients’ questions.
Appendix 1 – Emergency Abdominal
Appendix 2- Planned Minor
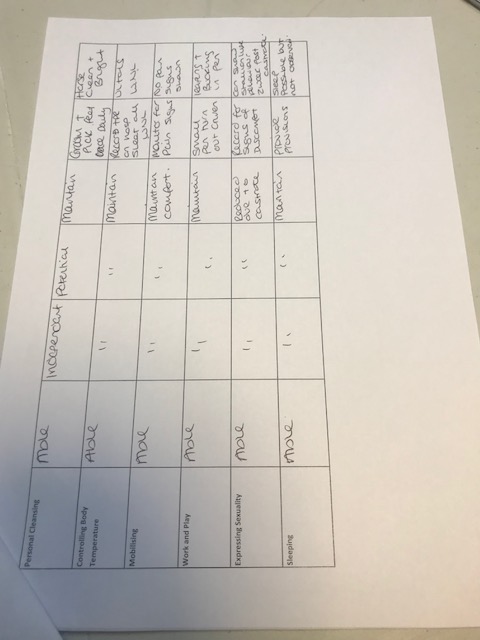
Appendix 3- Planned Head/Neck Surgery
Appendix 4- Planned Orthopaedic Surgery

Cote, N and Koenig J. (2006). Equine gastrointestinal motility — ileus and pharmacological modification. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1461410/. Last accessed 16th November 2017.
Cooper,B Mullineaux,E Turner L (2011). BSAVA Textbook of Veterinary Nursing. 5th ed. Gloucester: BSAVA. 601
Cooper,B Mullineaux,E Turner L (2011). BSAVA Textbook of Veterinary Nursing. 5th ed. Gloucester: BSAVA. Page- 601
Cooper,B Mullineaux,E Turner L (2011). BSAVA Textbook of Veterinary Nursing. 5th ed. Gloucester: BSAVA. Page- 216
Coumbe K (2001) Equine Veterinary Nursing. 1st Edition. Oxford- Blackwell. Page 370
Coumbe K (2001) Equine Veterinary Nursing. 1st Edition. Oxford- Blackwell. Page 418-419
Coumbe K (2001) Equine Veterinary Nursing. 1st Edition. Oxford- Blackwell. Page 418
Pullen, S and Gray, C (2006). Ethics, Law and The Veterinary Nurse. Philadelphia: Elsevier LTD. Page- 82.
MedicineNet. (2011). Medical Definition of Prophylactic. Available: https://www.medicinenet.com/script/main/art.asp?articlekey=11902. Last accessed 17th November 2017.
PetMD. (2017). Intestinal Bacterial Infections in Horses. Available: http://www.petmd.com/horse/conditions/digestive/c_hr_endotoxemia. Last accessed 17th November 2017.
Succeed Veterinary Centre. (2017). NSAID Toxicosis (Right Dorsal Colitis). Available: https://www.succeed-vet.com/education/equine-gi-disease-library/colitis/nsaid-toxicosis/. Last accessed 20th November 2017.
Unknown. (2011). THE SKILLS OF PROVIDING THE CORRECT TYPE AND AMOUNT OF INFORMATION. Available: http://web.warwick.ac.uk/md/ukc/Explanation_and_Planning/s9_the%20skills%20of%20providing%20the%20correct%20type%20and%20amount%20of%20information.pdf. Last accessed 27th December 2017.
Veterinary Medicines Directorate. (2015). Horse medicines and record keeping requirements. Available: https://www.gov.uk/guidance/horse-medicines-and-recording-keeping-requirements. Last accessed 17th November 2017.
(5068 WORDS)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Veterinary"
A veterinarian provides care to animals, including the diagnosis and treatment of any diseases or other conditions that animals may have. A veterinarian practices veterinary medicine, and can also be known as veterinary surgeons or veterinary physicians.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




