Early Enteral Vs Parenteral Nutrition in Patients Undergoing Total Gastrectomy
Info: 9058 words (36 pages) Dissertation
Published: 11th Dec 2019
Tagged: Medical
Comparing early enteral versus parenteral nutrition in patients undergoing total gastrectomy – Systematic Review
Contents
Abstract 4 – 5
Introduction 6 – 9
Aims and hypotheses 10
Methods 11 – 17
Results 18 – 36
Discussion 37 – 40
Limitation 41 – 42
Conclusions 43 – 44 References 45 – 50
Abstract
Total gastrectomy with roux-en-y oesophago-jejunal anastomosis for reconstruction remains the primary therapeutic method for resectable gastric cancer. Recent literature reported on the beneficial effect of early enteric feeding to facilitate early enteral nutrition. There is controversy in the literature regarding the optimal route of feeding post-total gastrectomy- total parenteral nutrition (TPN), early enteric feeding (EEN) with nasojejunal tube or oral diet on post-op day 2-3 as tolerable with support of intravenous fluid.
The aim of this systematic review is to compare differing feeding strategies in the early post-operative period for patients following curative total gastrectomy for malignancy.
A comprehensive search of medical databases including PubMed, Cochrane Library, ScienceDirect, CNKI were performed using the keywords “gastric cancer, total gastrectomy, supplemental tube enteric feeding, total parenteral feeding, NJ feeding”. Selection criteria: randomized controlled trials (RCTs) that compare TPN versus EEN feeding post-operatively for patient who undergone total gastrectomy. Post-operative complications and length of hospital stay were evaluated. Bariatrics surgery and sub-total gastrectomy patients are excluded. Animal studies are also rejected.
PRISMA Flow Diagram used as guidance to carry out this research. Began with identification of records through database search with keywords. Then followed by screening where duplicated studies will be removed. All studies will be screened for eligibility. Those which not matching inclusion criteria has been removed. Finally, inclusion where studies will be for qualitative synthesis. Results of trials are analysed individually under different outcome measures including post-operatively complication, length of hospital stay and cost effectiveness. Risk of bias chart generated by using RevMan5 software.
The main area of potentially difficult is due to some limitations in data analysis for example bias risk and heterogeneity among the included RCTs. Different discharge criteria due to geographical variation also leading to inconsistent outcome measurement. Total of 17 randomized clinical trials included in this systematic review which consisted of total 1093 patients with total gastrectomy. Results concluded that early post-total gastrectomy EEN reduces the length of hospital stay and post-operative infectious/non-infectious complication. EEN is also more cost-effective compare to TPN.
Introduction
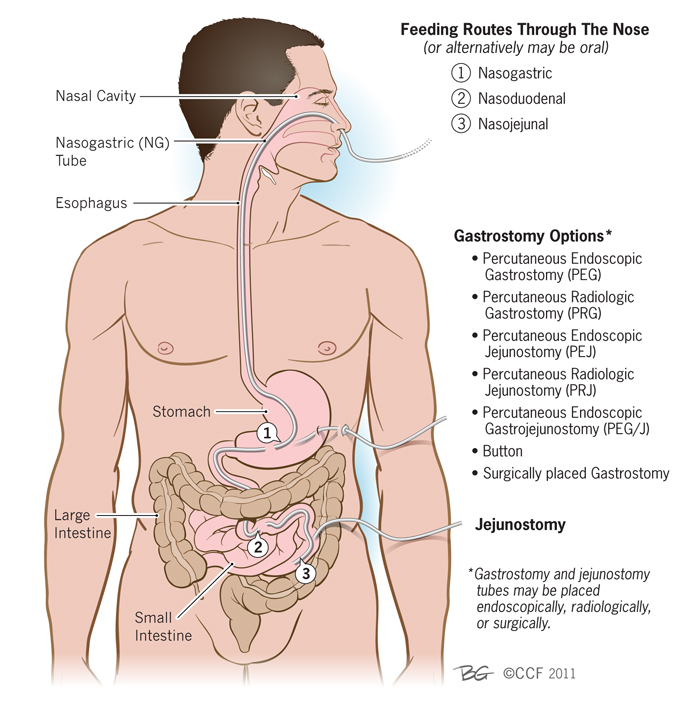
Gastric cancer is 3rd common cause of cancer death worldwide. [1] There are four main types of gastrectomy which all carried out under general anaesthetic – subtotal/partial gastrectomy, total gastrectomy, sleeve gastrectomy and oesophagogastrectomy. This surgery could be done either open or laparoscopically. Total gastrectomy with roux-en-y oesophago-jejunal anastomosis for reconstruction remains the primary therapeutic method for resectable gastric cancer. [2] Nutritional support to reduce morbidity and mortality in patient undergone total gastrectomy is vital and should be optimize to enhance recovery.
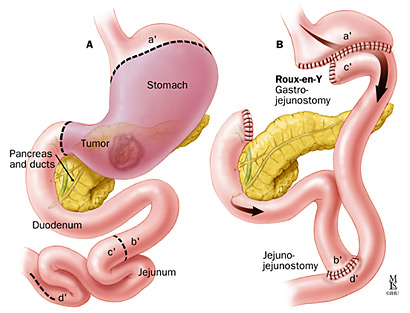
Figure 1: Total gastrectomy with Roux-en-y oesophagojejunal anastomosis for reconstruction.
Over the last 20 years, new concept perioperative care or referred to as “enhanced recovery after surgery” (ERAS) has been introduced and the main pillar of ERAS include early enteral feeding (EEN) after surgery. [3] National Institute for Health and Care Excellence (NICE) guideline (CG32) recommended enteral tube feeding for patient who are malnourished or at risk of malnutrition and due to major abdominal procedure unless contraindicated. [4]
Surgeons traditionally preferred total parenteral feeding as opposed to enteral route feeding after surgery, citing that to protect the newly formed anastomosis. Recent literature reported on the beneficial effect of early enteric feeding to facilitate early enteral nutrition (EEN). [5] There is controversy in the literature regarding the optimal route of feeding post-total gastrectomy- total parenteral nutrition (TPN), early enteric feeding with nasojejunal (NJ) tube or oral diet on post-op day 2-3 as tolerable with support of intravenous fluid.
There are still some practice around the world where surgeons not fully convinced that EEN is harmless to anastomoses. Traditionally post-operative management often involves TPN plus intravenous IV fluid for 7-10 days. Therefore, this patient’s population only commence oral diet or (NJ) tube feeding after fasting post total-gastrectomy for 5 – 7 days and this is detrimental to nutritional status of patient who had total gastrectomy. Therefore, this systematic review is to summarize the various studies published in major database comparing different feeding strategies in the early post-operative period which is vital for recovery of patients’ nutritional status. Hence, our first research question is “Is early enteral feeding better in nutritional support for recovery of post total gastrectomy patient compare to total parenteral feeding”
Early enteral nutrition was delivered via a needle catheter jejunostomy which usually commenced within 12 hour postoperatively starting with slow feeding rate and then increasing as tolerated by 10ml/h every 12 hour until maximum feed target feeding rate of 80ml/h was achieved. Intravenous fluid was administered in addition to maintain fluid balance closely.
Besides, there is also non-consistent studies finding whether NJ tube or jejunostomy created whilst on operation is preferred way of enteral feeding compare to early oral diet without NJ tube feeding. Hence this leading to second study question “Which is the preferred route of early enteral feeding? NJ tube feeding, jejunostomy feeding or oral diet?”
Figure 2: Various methods of enteral access (i.e.: nasojejunal tube, jejunostomy) for postoperative nutrition
Deficiencies in evidence around this subject leading to this systematic literature review project. This is to identify studies available electronically from multiple databases, to appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a given research question.
Aim and hypotheses
The aim of this systematic review is to compare differing feeding strategies in the early post-operative period for patients following total gastrectomy for stomach cancer.
Study Question 1
Is early enteral feeding better than total parenteral feeding for postoperative nutrition for patient underwent total gastrectomy?
Study Question 2
Which route of early enteral feeding is the best? Nasojejunal (NJ) feeding vs jejunostomy feeding vs purely oral diet
Methods
Protocol and registration
This systematic review was performed in accordance with the PRISMA guidelines through a systematic search in attempts to identify as much studies as possible. This review has been registered with the International Prospective Register of Systematic Review (PROSPERO). The registration of this systematic review can be found online at this Web address: https://www.crd.york.ac.uk/PROSPERO/registerreview.php Registration number 64479.
Eligibility Criteria
Selection criteria: Randomized controlled trials (RCTs) including prospective and retrospective randomized control trial, cohort studies of comparing enteral and parenteral nutrition post-operatively for patient who undergone total gastrectomy. PICO’s Criteria has been used to select trials to be included in systematic review.
| PICO’ Criteria | Descriptions and search terms used for each criterion |
| Patients | Patients with upper gastrointestinal cancer after surgery (total gastrectomy) |
| Intervention |
|
| Comparisons | Comparison between TPN and EN (randomized controlled trial) |
| Outcome | Morbidity (infectious complication or non-infectious complication)
Length of hospital stay (length of post-operative hospital stay or time in hospital) |
Table 1: PICO Criteria
Systematic review search was carried out in multiple databases but only applicable to studies with language in English and Chinese only. Outcome measures of trials which aimed at comparing EEN vs TPN in terms of postoperative length of hospital stay, post-operatively complication is included in this systematic review.
Exclusion criteria
Any trials which did not meet eligibility criteria such as bariatrics surgery and sub-total gastrectomy patients are excluded. Animal studies are also rejected. The rationale of these is because of different age group of patients presented with Upper GI malignancy versus patient for bariatric who usually with background of multiple comorbidities which might hinder the outcome of post-operative complication morbidity and mortality. Sub-total gastrectomy patient group are excluded because the nature and indication of surgery is different from total gastrectomy [sub-total gastrectomy was performed in patients with antral tumours and total gastrectomy was performed for tumours of the cardiac Siewert type II, body and linitis plastic. Hence sub-total gastrectomy patient group were also excluded from this systematic review.
Following articles were excluded: 1) articles not reporting outcomes of interest 2) duplication of RCTs publication 3) studies lacking essential information or study characteristics.
Information sources
Randomized controlled trials published in databases between period from year 1996 to 2016 are included in this systematic review.
Literature Search
A comprehensive full electronic search of medical databases which including PubMed, Cochrane Library, ScienceDirect, Embase, CNKI were performed using the keywords “gastric cancer, total gastrectomy, supplemental tube enteric feeding parenteral feeding, total parenteral nutrition, nasojejunal feeding” to identify published trials evaluating total parenteral nutrition versus early enteral nutrition feeding for post-operative total gastrectomy patient.
This study included many studies which published in Chinese language in CNKI. Database CNKI searched using mandarin key words and date ranging from 1997- 2006 year included. Most of the research trials from CNKI has got English version in their abstract. Detailed search steps were described using the PRISMA 2009 flow diagram.
Study Selection
PRISMA Flow Diagram used as guidance to carry out this research. Begin with identification of records through database search (on CNKI, ScienceDirect, PubMed) with keywords (total gastrectomy total parenteral nutrition, early enteral nutrition, supplemental tube feeding, NJ feeding). Total number of 367 studies identified which then followed by screening where 41 duplicated studies have been removed.
All records have been screened and excluded the studies which are not relevant to aim and research questions of systematic review. By screening through the title and abstracts of paper, a total of 289 of record were excluded from study because those study does not fit into the criteria. Finally, 25 study trials assessed for eligibility and those which are not matching inclusion criteria have been removed for example non-RCTs, meta-analysis, insufficient data, animal studies. Finally, a total number of 17 randomized controlled trials included in this systematic review.
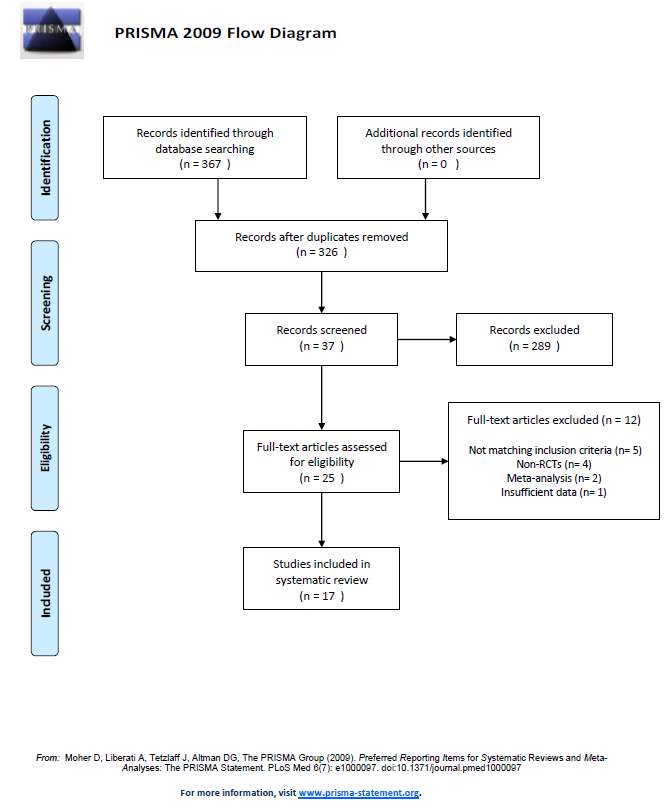
Figure 1: The Flow Diagram of study selection according to PRISMA 2009
Data collection process
Data extracted by author according to following characteristics for each study: author, journal, publication year, number of patients, research design, geographical region, post-op infectious and non-infectious complication and length of hospital stay.
Quality assessments
Among the 17 trials which finalized for inclusion into this systematic review, no trial was completely free of bias. Most of the trials were identified to be of low-risk.
Risk of Bias
Bias risk evaluated as per Cochrane methodology by using the assessment tool published in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 to evaluate six main domains.
| Random sequence generation | Selection bias |
| Allocation concealment | Selection bias |
| Blinding of participants and personnel | Performance bias |
| Blinding of outcome assessment | Detection bias |
| Incomplete outcome of data | Attrition bias |
| Selective reporting | Reporting bias |
Table 2: Example of a ‘Risk of bias’ table for a single study (table taken from Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0)
Quality of studies assessed using Cochrane collaboration tool which including: randomization sequence generation, allocation concealment, blinding of participants and personnel in all studies, blinding of outcome assessment, incomplete outcome of data, selective reporting and other bias.
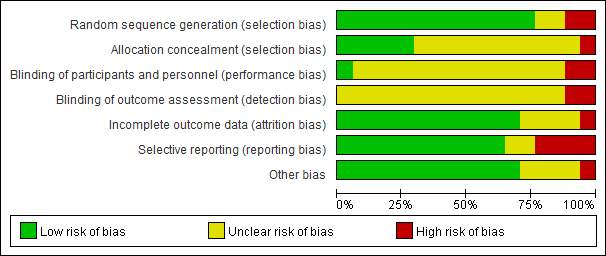
Figure 2: Bar chart showing sources of potential risk of bias for the 17 randomized controlled trials included in systematic review assessing the TPN and EEN patients group post total gastrectomy.
Results
By using PICO’s Criteria where focused appropriate study characteristic included in systematic review. Quality assessment of study through bias risk evaluation as per Cochrane methodology by using the assessment tool published in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [4].
| Author, date | Study type | Patient group | Outcomes | Key Results |
| Brage et al. 2001 Italy [6] | Prospective randomised trial | Gastrectomy (n=111) | – Length of stay (days)
– Infectious Complications |
– EEN 16.1 +/- 5.9 vs TPN 17.5 +/- 6.1
– EEN 13/55 (23.6%) vs TPN 16/56 (28.5%) |
| Sand et al. 1997 Finland [7] | Prospective randomised trial | Gastrectomy (n=29) | – Complications | – EEN 3/13 (23%) vs TPN 4/16 (24%) |
| Reynolds et al. 1997 UK [8] | Prospective randomised trial | Gastrectomy (n=67) | – Infectious complication
– Non-infectious complication |
– EEN 13/33 (39.4%) vs TPN 20/34 (58%)
– EEN 13/33 (39.4%) vs TPN 17/34 (50%) |
| Baigrie et al. 1996 Australia [9] | Prospective randomised trial | Gastrectomy (n=97) | – Infectious complication | – EEN 3/50 (6%) vs 10/47 (21.3%) |
| Wei Chen et al 2014 China [10] | Prospective randomised trial | Gastrectomy for gastric cancer (n=72) | – Length of stay (days)
– Incidence of complication |
– EEN 12.2+/- 2.5 days’ vs 14.9 +/- 2.9 days (p value of 0.982)
– EEN 8.1% vs TPN 25.67%. (p > 0.05) |
| Li et al. 2011 China [11] | Retrospective randomised trial | Gastrectomy (n=116)
TPN 54, EEN 62 |
|
– EEN 12/62 (19.35%) vs TPN 13/54 (24.07)
– EEN 15 +/- 7.31 vs TPN 15.41 +/- 11.57 |
| Barlow et al. 2011 UK [12] | Prospective randomised trial | Total Gastrectomy (n=20) |
|
– EEN 32.8% vs TPN 50.9% (p = 0.044)
– EEN 16 days vs TPN 19 days (p= 0.023) |
| Kim et al. 2012 Korea [13] | Prospective randomised trial | Gastrectomy (n=56) |
|
– EEN 12 days vs TPN 13 days (p = 0.289) |
| Weng et al. 2008 China [14] | Prospective randomised trial | Total gastrectomy (n=40) |
|
|
| Chen et al. 2005 China [15] | Prospective randomised trial | Total gastrectomy (n=57) |
|
|
| Deng et al. 2008 China [16] | Prospective randomised trial | Total gastrectomy (n=46) |
|
|
| Liu et al. 2006 China [17] | Prospective randomised trial | Total gastrectomy (n=66) |
|
|
| Yuan et al. 2010 China [18] | Prospective randomised trial | Total gastrectomy (n=86) [TPN 31 vs EEN 55] |
|
|
| Li et al. 2016 China [19] | Prospective randomised trial | Total gastrectomy (n=72) |
|
|
| Hoon et al. 2011 Korea [20] | Prospective randomised trial | Total gastrectomy (n=54)
TPN 26 vs EEN 28 |
|
|
| Kim et al. 2008 Korea [21] | Prospective randomised trial | Total gastrectomy (n=66)
TPN 31 vs EEN 35 |
|
No difference in the morbidity rate (p= 0.392)
EEN 8.03 +/- 1.43 vs TPN 9.97 + 2.07 |
| Zhang et al. 2009 China [22] | Prospective randomised trial | Total gastrectomy (n=38) |
|
TPN 14.8 + 5.1 vs EEN 11.1 +3.2 days |
Table 3: Summary of results of 20 trials for systematic review
Results of individual studies
Systematic review included total of 20 trials, published from 1997 to 2016 with 1093 patients who underwent total gastrectomy (with other types of Upper GI surgery including subtotal gastrectomy excluded). 516 patients and 577 patients were randomized to postoperative TPN and EEN group respectively. Among these, 10 trials reported postoperative complications. 13 trials reported length of hospital. Finding were summarized as in Table above.
Gut Motility & Function Recovery
Wei Chen et al. [10] study suggested that the gastrointestinal anatomical structure and physiological normal function are abnormal because of post-traumatic stress which leading to reduce sugar usage, increased protein and fat decomposition and increased urinary nitrogen excretion. Hence, disturbance to carbohydrate metabolism and consequence by hyperglycaemia increased the chance of post-operative complication i.e. wound infection and diabetic complication for certain group of patients.
Wei Chen at el. [10] suggested that EEN with continuous enteral nutrition provided closer to natural form of nutrition and able to minimally disturb postoperative changes of physiological function of gastroenterology system. The method of EEN used in Wei Chen et al. through nasojejunal tube that was inserted during route-en-y reconstruction after gastrectomy beginning with PepTI EEN formula infusion slow infusion and gradually increase rate of infusion as patient’s tolerance increased. TPN group patients were given internal jugular vein catheterization on day 1 postoperative. Nutrient solution ratio of saccharides to fat and non-protein to protein calories were 2:1 and 100:1 respectively with supplement nutrient such as vitamins and other trace elements. The supplement continued until patient able to tolerate certain amount of oral diet. This study doesn’t specify the criteria of the day patients starting oral intake hence there is risk of reporting bias in this study.
EEN promote the recovery of intestinal peristalsis by maintaining the structure and function of the intestinal epithelial cells, reduce the metabolism reaction of the intestinal mucosa, reduce the ischaemic status of intestinal mucosa and improving splanchnic blood flow. Slow infusion rate of the nutritional enterally followed by gradually increasing speed of infusion to avoid abdominal distension caused by early too fast and too much infusion of nutrient solution. [23]. Some studies shown that intestinal peristalsis and absorption functions could only return to normal state 6-8 hours postoperatively and absorption function of gastrointestinal could then meet our body’s minimum requirement.
Wei Chen et al. study [10] included study sample of reasonable size of total 82 patients and included their study characteristics. Table provided in this paper which summarized number of postoperative complications, length of hospital stays in day, hospitalization expenses, and time of first bowel movement post-operative. The time of first bowel movement and time of first soft diet were 2.5 days and 6.9 days in comparison to TPN group which is first bowel motion at 5.4 days and first intake of soft diet orally at 8.0 days respectively.
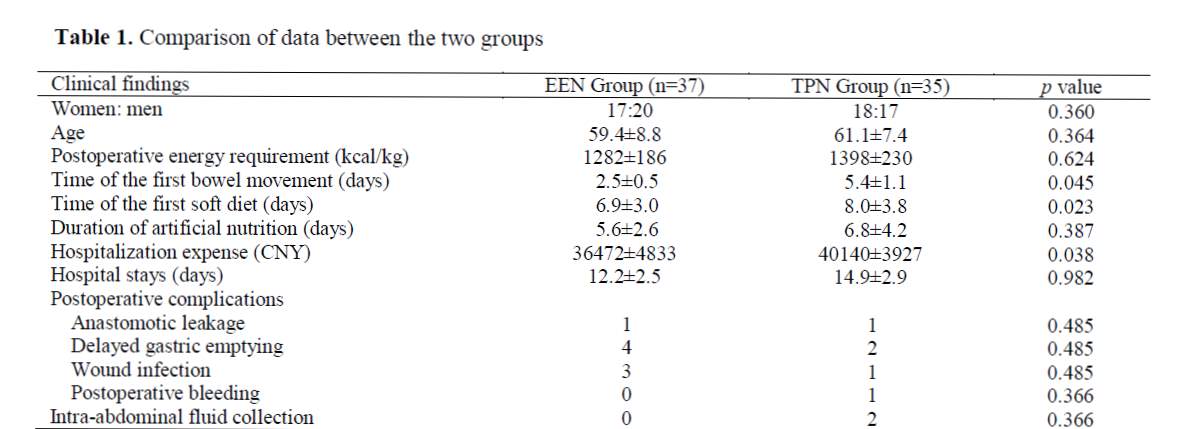
Appendix 1: Wei Chen et al. Comparison of data between the two groups.
Liu et al. [17] conducted study effects of early enteral nutrition after total gastrectomy in elderly patients of gastric cancer group. 66 cases divided into two equal group randomly. The results shown that no statistical significance between EEN and TPN group in nutritional status and incidence of postoperative complication, but EEN had earlier recovery of intestinal function and shorter length of hospital stay.
This study concluded differently comparing to Wei Chen et al. [10] who suggested that the early feeding encourage better nutritional status leading to less postoperatively complications because Liu et al. [17] measure the recovery of intestinal function by monitoring patient’s first time of flatus or first bowel movement. The study did not associate the link between early intestinal function recovery reduce the incidence of postoperative complication. Hence, future study of this relationship would be useful to consider EEN and TPN effect on gut motility and function.
Post-operative complication
Post-operative complication is widely used in many trials as a primary outcome measure. Sand et al. [7] presented a study of a group of 29 patients in which 13 of the patients receiving NJ tube early enteral feeding and 16 of the rest of patients receiving TPN feeding. The study concluded that 3 of the patient who receiving EEN versus 4 of the TPN group of patients suffered with minor non-infectious complication. This study also concluded that enteral nutrition is significantly cheaper than parenteral nutrition.
Li et al. [11] conducted a retrospective review of 116 patients who undergone total gastrectomy with Roux-en-Y oesophagojejunostomy all under standard midline laparotomy. This study which included reasonable size of sample group with relatively equal baseline characteristic (i.e. gender ratio, mean age, BMI, preoperative morbidity, TNM staging and ASA classification). Patient in EEN group was inserted with a single-lumen nasojejunal tube, fed into jejunum lumen with catheter tip advanced approximately 10-20 centimetres beyond the actual site of jejunum-jejunum anastomosis. EEN feeding was well tolerated by most of patients , only two cases excluded from studies due to non-compliance of NJ tube feeding. Difference between this study to open study trials is that the timing of commencement of enteral feeding.
Li et al. [11] study started within 24 hours of operation although there is no specify exact of infusion started. There are slight variation of this study compare to other trials because the rate of infusion of enteral feeding was adjusted according to patients symptoms (for example: abdominal cramping, distention, nausea or vomiting). If the goal of nutrition was not achieved, they will supplied nutrition parenterally. This study divided the complications into major and minor categories. Major complications included pneumonia, wound infection, abdominal infection, intestinal obstruction, anastomotic leak, lymphoid leak, duodenal stump leak, anastomotic stenosis and death.
Risk of bias
In the study report, only one death in EEN group has been discussed which is due to anastomotic leakage and the patient gave up for financial reason and died. There is no report of the reason of other 2 deaths in TPN group which is important to know whether it is related to TPN used. Therefore, there might be reporting bias in this study because the author selectively reporting mortality of one group but not the other.
Below is a summary table of postoperative major and minor complication.
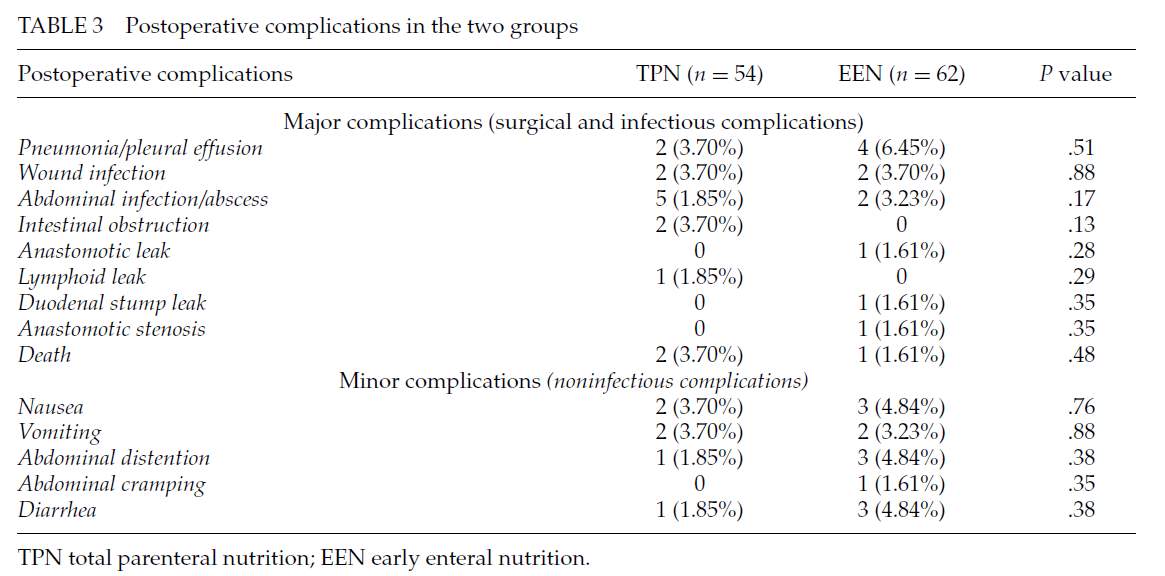
Appendix 2 Table from Li et al. Postoperative complications in the two groups
Baigrie et al. [9] randomised total patient of 97 divided into 47 patients receiving TPN feeding at day 1 post-operation and 50 patients receiving enteral feeding via NJ tube which inserted operatively. They presented this study and showed there is no statistical difference in post-operative complication. On the other hand, the cost of EEN was concluded with 10 times cheaper than TPN therefore they are more in favour of EEN than TPN due to cost effective.
Barlow et al. [12] also concluded that EEN group associated with lower percentage of 32.8% postoperative complication compared to TPN group of 50.9%. This is largely due to wound infection 28.1% in TPN group and 10.9% in EEN group, chest infection 21% in TPN group and 7.8% in EEN group, anastomotic leak 12.2% in TPN group and 3.1% in EEN Group.
Kim et al. [13], a study from Korea presented a paper which shown that there is no significant difference found in the nutritional status parameters, complications and length of hospital stay between EEN and TPN groups on 7th day after total gastrectomy. Length of hospital stay in EEN group was 12 days, which is one day shorter than TPN group 13 days.
Risk of bias
Even though Kim et al [13] conducted study on total of 56 patients (36 EEN vs 20 TPN). Unfortunately, the drop out during study in almost 50% for EEN group due to various reason (i.e. 9 patients had feeding tube occlusion, 3 patients had feeding tube and 7 patients quit from study). Hence, the study scale of only 17 patients is relatively small compare to other study.
Length of hospital stays
Yuan et al. 2010 [18] studied done in China presented a total of 86 patients in which 31 patients received TPN and 55 patients received EEN. This study compared post-op commencement of bowel movement, post-op complication and length of stay of hospital. Study concluded that there is no significant difference (p>0.05) between patient’s receiving TPN or EEN. Hence, they suggested the insertion of NJ tube or TPN will be depending on patient’s preoperative status and patient’s preference.
Barlow et al. [12] conducted an open, prospective multicentre randomised controlled trial within a regional UK cancer network which included 38 total gastrectomy patients and analysed based on intention-to-treat and length of hospital stay as primary outcome measure. Barlow et al concluded that EEN was associated with significant shortened length of hospital stay. Barlow et al. study shown that median length of hospital stay was 16 days after EEN compared with 19 days after control management (which is total parenteral nutrition feeding) with statistically significant p value of 0.023 which p-value is less than 0.05.
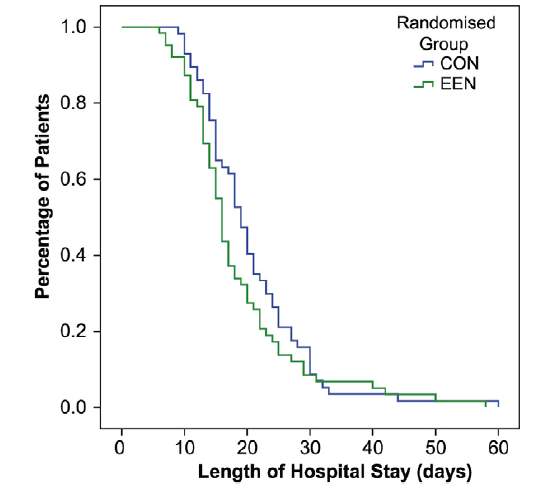
Appendix 3: Chart adopted from Barlow et al study showing length of hospital stay of EEN and control group (TPN)
Chen et al. [15] conducted a study on total of 57 patients with total gastrectomy considering effect of early enteral nutrition on immunological recovery of patient. The levels of serum albumin, transferrin, pre-albumin, CD3, CD4, CD8 were checked one day before operation and 9 days after operation. They found out that the levels of CD3, CD4 were significantly higher in EEN patient group than in TPN patient group. The number of postoperative infectious complications in EEN and TPN group were 5 and 2 respectively. The length of stay in EEN group was significantly shorter than that of TPN group (p value of <0.05). The costs of nutritional support were also lower in EEN group (CNY 1540 dollar = 173pound) versus TPN group (CNY 3986 dollar = 448pound). This figure of cost is consistent with another study done by Braga et al. which shown TPN is approximately 3-4 times more expensive than EEN.
Zhang et al. [22] study results shown that there is statistically significant decrease on length of hospital stay for patient received EEN compare to TPN post total gastrectomy. 38 patients divided equally into two groups of 19 patients each. Length of hospital stay for EEN group was 11.1+/- 3.2 days, whereas TPN group was 14.8+/- 5.1 days. (P value of <0.05). Hence this study again shown us that EEN is more effective for patient’s nutritional status post gastrectomy.
Cost Effective
Braga et al. [6] study shown that overall complication was lower in EEN patient group with 37.1% versus TPN patient group 52.0%. This study failed to demonstrate any improvement in term of the length of stay but they did however show statistically significant lower severity of postoperative complication in the early enteral nutrition group patient compare to total parenteral nutrition feeding patient group. Besides that, the mean cost per day for TPN group was 90.60 dollar which is almost 3-4 times more expensive than EEN group which is only 25 dollars. Finally, their conclusion is early enteral feeding is superior to TPN after major GI surgery particularly in high-risk surgical patients.
Reynolds et al [8] done a prospective randomised trial level II which consists 33 patients’ post-op enteral feeding and 34 patients with parenteral feeding postoperatively. This study shown that EEN has got less complication compare to TPN. The length of stay postoperatively wasn’t reported, but this study still recommended that EEN should be used because EEN is 10 times cheaper than TPN. This is consistent with Baigrie et al [9] and Braga et al [6] study results which proven that EEN is cheaper than TPN and hence more cost effective.
Hoon et al. [20] study conducted on 54 patients and divided into two groups with 28 patients under early feeding group and 26 patients as control group (TPN). Chi-square tests were used to analyse the distribution of enrolled patients according to appropriate clinic-operative and demographic characteristics. An independent t test was used to compare the duration of hospital stay, hospital cost and QOL questionnaire across two group of patients which wasn’t used by most other trials.
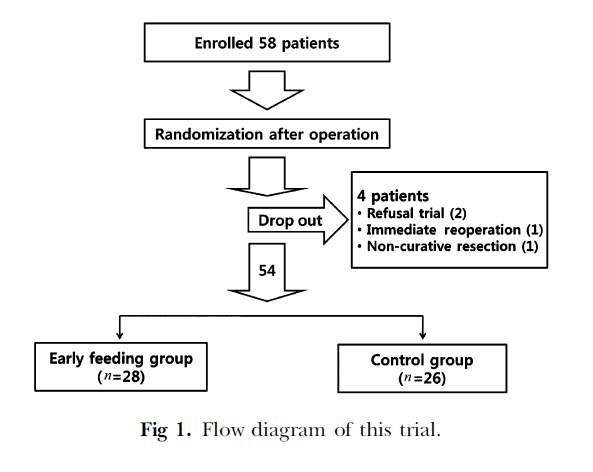
Appendix 4: Flow diagram of Hoon et al. study
Study shown that early oral feeding after total gastrectomy decrease the duration of hospital stay without increasing complications. The QOL (quality of life) questionnaire to access quality of life in which symptoms such as nausea vomiting, pain, dyspnoea, sleep disturbance, appetite lost, constipation or diarrhoea, physical & cognitive function is assessed using a scoring system and total score are calculated and published. For example, intensity of pain was assessed using scale measuring from 0 to 10 and postoperative symptoms including abdominal distension, vomiting, nausea, and diarrhoea were recorded on day 1, 3 and 5 post- gastrectomy.
QOL was conducted by nurse who was blinded to the patient treatment group. 8 out of 54 patients refused to answer questionnaire. Early oral feeding shown to improve bowel movement and some aspects of QOL immediately after gastrectomy for gastric cancer.
Performance bias has been avoided by blinding of participants and personnel. The results of this questionnaire presented as the sum of the scores from 22 items and did not show any differences in any categories.
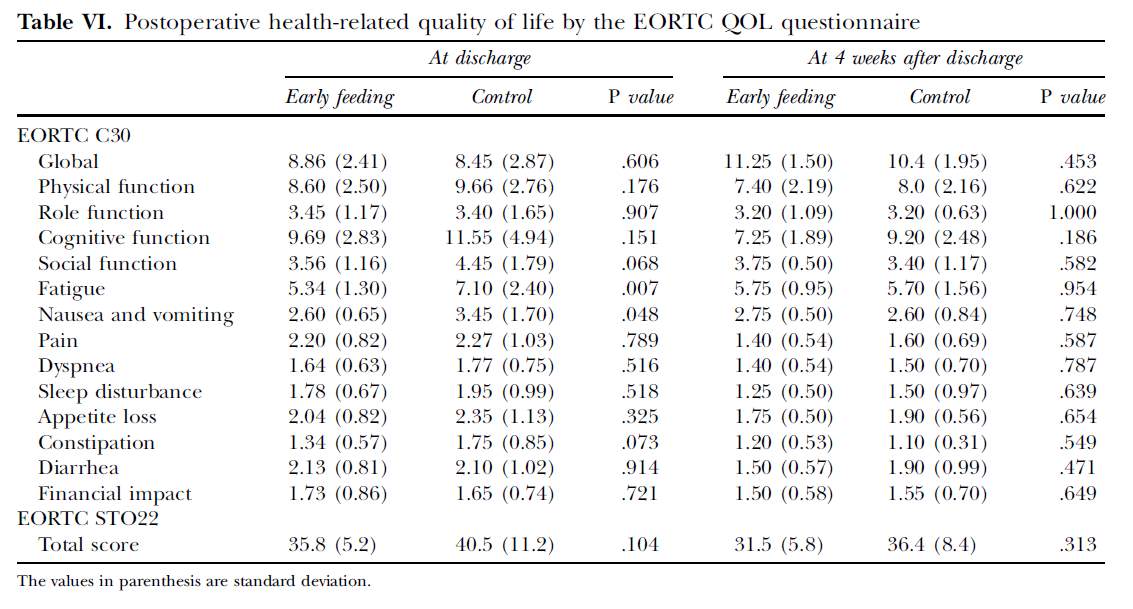
Appendix 5: QOL questionnaire outcome of quality of life assessment by Hoon et al study
Hoon et al. [20] study suggested oral feeding for enteral nutrition feeding instead of other enteral routes like tube jejunostomy or nasojejunal tube feeding which require another procedure that may lead to complications or inconvenience to patient. The discharge criterion including no specific complaints or abnormal signs 2 days after starting soft diet.
One of the latest study done by Li et al 2016 China [19] which included large scale of total 108 patients. 72 patients received early enteral nutrition while 36 patients received total parenteral nutrition postoperatively. Study concluded that EEN group of patients managed to reduce the length of hospital stay for 1.36 days (p < 0.05). This study suggested that early enteral feeding could improve the recovery and preservation of gut structure and function. Hence enhance gut mediated immunity and lessen the length of hospital stay.
Discussion
Summary of evidence
This systematic review of 20 randomized controlled trials, containing 1093 patients. From the results, although there is lack of homogenous consistency of outcome measure in terms of postoperative complication. We found that EEN could generally improve clinical outcomes by decreasing the rate of postoperative complications (including wound infection, anastomotic leakage, postoperative bleeding, intra-abdominal fluid collection, pneumonia, pleural effusion, lymphoid leak, duodenal stump leak, anastomotic stenosis, abdominal abscess), shorten the length of hospital stay postoperatively. However, the length of hospital stay remain heterogeneity due to variation of geographical location/country.
This study included many studies which published in Chinese language in CNKI. China is a country which known to have one of the largest number of gastric cancer due to diet that included large amounts of smoked food, pickled vegetables, salted fish and meat. This systematic review also focused on studies from East Asian countries such as China and Korea where gastric cancer is most common malignancy in the geographical region.
Recent RCTs studies shown that early enteral nutrition reported to preserve gut structure and function and enhance gut mediated immunity therefore is superior to parenteral nutrition because of fewer associated septic complications, and shorter lengths of hospital stay. Even though randomised comparisons studies have reported that EEN is superior to TPN, yet contemporary opinion is that EEN hasn’t formally recommended for routine clinical practice in various guidelines partly because benefits above remain unproven or lack of evidence (including size sample etc.).
Method of enteral nutrition also remain controversial because NJ tube feeding refused by some patients due to multifactorial i.e.: lack of compliance (happen in elderly age group of patients with dementia), or poorly tolerated by patients. Jejunostomy placement for enteral feeding is not only invasive, but often associated with various complications.
More recently, there is discussion regarding whether early volitional oral intake as method of early enteral feeding in first 1-3 postoperative days is even better than using nasojejunal feeding or jejunostomy feeding. Without doubt, contemporary enhanced recovery after surgery programmes no long suggest prolonged periods of post-operative “nil by mouth” strategy. Therefore, early oral introduction of feed such a sip of water and soft diets following by early build up to free diet has been introduced by some surgeons.
Early nutritional support is most important and often required for patient undergoing total gastrectomy who are usually malnourished due to sign and symptoms of cancer. Patients with gastric cancer generally possess various degrees of malnutrition due to their symptoms including dysphagia causing inability to eat proper meal, and less consumption of food. Multiple techniques are used to give post-operative nutritional support (i.e.: via nasojejunal tube feeding, total parenteral nutrition or early enteral nutrition). Many Upper GI surgeons traditionally use TPN as opposed to early enteral nutrition citing the need to protect the newly formed anastomosis post total-gastrectomy.
Wei Chen et al. study included study sample of reasonable size of total 82 patients and included their study characteristics. Table provided in this paper which summarized number of postoperative complications, length of hospital stays in day, hospitalization expenses, and time of first bowel movement post-operative. This study also measured the time to achieve nutritional index by measuring the pre-albumin, transferrin and post op weight recovery. Study suggested that body recovery in EEN group is faster than TPN group at 3 weeks after gastrectomy by claiming that this is something to do with appetite, but unfortunately there is no clear evidence to support this mechanism hence this is not statistically significant.
Barlow et al conducted open prospective pragmatic multicentre randomised controlled trial in three NHS National Health Service UK trust which were part of South East Wales Upper Gastrointestinal Cancer Network. This study provided clear description of how randomisation was stratified within each centre by randomisation sequence generated by computer in permuted blocks of 30. Data entry and statistical analysis were totally blinded to group allocation. Out of the total of 38 undergone gastrectomy, only 20 patients under category of total gastrectomy of which 12 patients received EEN and 8 patients received TPN postoperatively. Besides, precise definitation of primary outcome measurement of trials is crucial in future development but controversial because length of hospital stay could be dependent on many factors such as patients’ age group, and ASA performance status preoperatively, intraoperative complication, surgeonl’s skills and experiences, level of lymphadenectomy and blood loss intraoperatively, all of which have been associated with variations in length of hospital stay. [24] [25]
Limitations
The main are of limitations in data analysis are due to heterogeneity among the included RCTs. The population sample of each studies consists of mixture of patient undergoing different types of upper GI surgery such as oesophagectomy, total gastrectomy, sub-total gastrectomy etc. Some studies had poor quality assurance, which included prominent heterogeneity in terms of certain outcome measurements. Therefore, the risk of bias remains limitations of systematic review.
Secondly, language remains to be a barrier in the global communication of research. Limitation by retrieval process only conducted in selective databases such as PubMed, CNKI, ScienceDirect which mean studies in language other than English and Chinese were excluded from systematic review, there is possibility that additional relevant extended studies may have been missed.
Besides, the study trials conducted by China included in this systematic review are mainly in Chinese language with English version of their abstract. Hence there are limitations in accessing the full text of research paper due to various reason including not accessible via institutional login.
There is limitation as well in study done by Wei Chen et al. [10] regarding the use of scored Patient-Generated Subjective Global Assessment (PG-SGA) [26] as a nutrition assessment tool in patients with cancer. This PG-SGA was not given in blinded fashion by staff to patient and the size of sample is only 72 patients in total. Hence, further large size of study samples in a randomized blind fashion should be used to reach statistically significance of PG-SGA scoring system.
In study conducted by Barlow et al [12], the primary endpoint of study was length of hospital stay and it was defined as patient assessed by operating surgeon and deemed fit for discharge home or transfer to sub-acute service (whichever comes first). The limitation for this study is that there are no strict, precise discharge criteria were used to define when patients were fit for discharge. There are many patients who waiting for package of care on discharge, or requiring input from rehabilitation team (i.e.: occupational therapist, physiotherapist) prior discharge.
Hence, there might be patient who surgically fit for discharge but patient keep in hospital due to various reason (i.e.: awaiting care package, not able to cope at home due to background past medical history). Non-consistent of discharge criteria has been used by different hospital from different geographical location also limitation of this systematic review There are also discrepancy regarding ASA grade of patient undergone total gastrectomy
Conclusions
This systematic review suggests that early enteral nutrition for post total gastrectomy patients could reduce the incidence of morbidity, reduce the length of hospital stay which leading to relatively cost effective compare to total parenteral nutrition. Morbidity including respiratory tract infections, post-operatively wound infection, anastomotic leakage, abdominal infection/abscess, duodenal stump leak, intestinal obstruction etc.
Early enteral feeding regardless of what methods used generally improved clinical outcomes in terms of postoperative morbidity, mortality, shorten length of hospital and cost effective. This review confirmed and refute the findings observed in previous small trials. Most studies shown that EEN was associated with significantly shortened length of hospital stay and improved clinical outcomes. Early post-total gastrectomy nasojejunal NJ tube feeding and oral diet also reduces postoperative complication – including infectious and non-infectious complication.
The common way of EEN feeding are nasojejunal tube or jejunostomy. One study (Wei Chen et al) study suggested that nasojejunal tube is superior to jejunostomy because firstly there is no need of fistula to be created for jejunostomy therefore avoiding jejunostomy related complications. However, there are some studies also shown that NJ tube has also some disadvantages which including throat discomfort, mucus hypersecretion, induce nausea and vomiting, interfere with patient’s cough reflex and expectoration hence there is concern about leading to risk of reflux and aspiration pneumonia.
Novelty of this research project addressed a question that is important and relevant to daily practice of ERAS amongst the upper GI surgeons and this could potentially lead to the implementation of guidelines by introducing the use of criteria to stratify the route of early enteral nutrition post total-gastrectomy. Overall, EEN is more cost effective compare to TPN and EEN should be the optimal management while the use of TPN should only be reserved for patients with severe intolerance to enteral nutrition. This eventually purposed to provide recommendations based on a higher level of evidence to standardize our practice.
This systematic review was carried without meta-analysis. Recommendation for future development of meta-analysis of comparing TPN vs EEN by measuring more consistent post-operative complication and length of hospital stay with consistent discharge criteria. Besides, more randomized controlled trials or cohort studies comparing different routes of EEN (comparing: NJ tube, jejunostomy or simply oral diet) is also high recommended.
Funding
This work has not received financial support.
Conflict of interest
The authors declare no conflict of interest
References
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray, F.GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 Lyon, France: International Agency for Research on Cancer; 2013.
- Scurtu R, Groza N, Otel O, Goia A, Funariu G. Quality of life in patients with esophagejejunal anastomosis after total gastrectomy for cancer. Rom J Gastroenterol 2005; 14(4): 367-72.
- Dorcaratto D, Grande L, Pera M.Enhanced recovery in gastrointestinal surgery: upper gastrointestinal surgery. Dig Surg. 2013; 30(1): 70-8 Epub 2013 May 25.
- Nutrition Support in Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. NICE Guidelines (2014)
- Rachael Barlow, Patricia Price, Thomas D Reid, Sarah Hunt, Geoffrey W.B.Clark, Timothy J. Havard, Malcolm C.A. Puntis, Wyn G. Lewis. Prospective multicentre randomised controlled trial of early enteral nutrition for patients undergoing major upper gastrointestinal surgical resection. Clinical Nutrition Volume 30, Issue 5, October 2011, Pages 560-566.
- Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, Di Carlo V, Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med 2001;29:242-8.
- Sand J, Luostarinen M, Matikainen M. Enteral or parenteral feeding after total gastrectomy: prospective randomised pilot study. Eur J Surg 1997; 163(10):761-6.
- Reynolds JV, Kanwar S, Welsh FK, Windsor AC, Murchan P, Barclay GR, et al. Does the route of feeding modify gut barrier function and clinical outcome in
patients after major upper gastrointestinal surgery? J Parenter Enter Nutr 1997;21:196e201.
9. Baigrie RJ, Devitt PG, Watkin DS. Enteral versus parenteral nutrition after oesophagogastric surgery: a prospective randomized comparison. ANZ J Surgh 1996:66:668e70.
10. Wei Chen MD, Zheng Zhang MM, Maoming Xiong MD, Xiangling Meng MM, Fen Dai BS Nurs, Jun Fang MM, Hong Wan MM, Miaofeng Wang MM. Early enteral nutrition after total gastrectomy for gastric cancer. Asia Pac J Clin Nutr 2014;23(4):607-611
11. Junsheng Li MD, Zhenling Ji MD, Congwei Yuan MD, Yanan Zhang MD, Weidong Chen, Xingtang Ju & Wenhao Tang MD. Limited Efficacy of Early Enteral Nutrition in Patients after Total Gastrectomy. Journal of Investigative Surgery.
12. Rachael Barlow, Patricia Price, Thomas D. Reid, Sarah Hunt, Geoffrey W.B. Clark, Timothy J. Havard, Malcolm C.A. Puntis, Wyn G.Lewis. Prospective multicentre randomised controlled trial of early enteral nutrition for patients undergoing major upper gastrointestinal surgical resection. School of Medicine, Cardiff University, Cardiff, UK.
13. Hye Un Kim, Jai Bock Chung and Choong Bai Kim. The Comparison between Early Enteral Nutrition and Total Parenteral Nutrition after Total Gastrectomy in Patients with Gastric Cancer: The Randomized Prospective Study. Korean J Gastroenterol Vol. 59 No. 6, 407- 413
14. Weng Yanhong, Zhu Yonglong, Ye Xiaoli, Jiang Meifang, Jiang Mingfang. Effect of early enteral nutrition in support of patient post total gastrectomy. An Hui Medical Journal 2008(29)- 1. ISSN: 1000-0399
15. Chen Sizeng, Lin Yong. Early Enteral Nutrition Support for Post-operative Total Gastrectomy in Elderly Group of Patient. Chinese Journal of Geriatics 2005 (10) ISSN 0254-9026.
16. Deng Xin, Zhao Yi, Wang Qiang. Application of Early Enteral Nutrition for Post-Total Gastrectomy. Chinese Journal of Practical Surgery 2008 (09) ISSN: 1005-2208
17. Liu Bin, Yu DongFeng. Comparison of Early Enteral Nutrition versus Total Parenteral Nutrition for Elder Patient who undergone Total Gastrectomy. Chinese Journal of Postgraduates of Medicine 2006 (14). ISSN: 1673-4904
18. Yuan Zhonghua, Li Junsheng, Zhang Yanan, Chen Weidong, Ju Xintang. Study of comparison between total parenteral nutrtion feeding versus early enteral nutrition feeding for patient undergone post total gastrectomy. Chinese Journal of Bases and Clinics in General Surgery 2010 (04) ISSN: 1007-9424
19. Li Ceng, Chen Guijin, Guo Yulin, Xu Xiao, Guan Yanbin, Wang Yu, Dong Guanglong. Observation of therapeutic effects of Early Enteral Nutrition versus Total Parenteral Nutrition for Total Gastrectomy patient postoperatively
20. Hoon Hur, MD, Sung Geun Kim, MD, Jung Ho Shim MD, Kyo Young Song, MD, Wook Kim, MD, Cho Hyun Park, MD, and Hae Myung Jeon, MD, PhD. Effect of early oral feeding after gastric cancer surgery: A result of randomized clinical trial. Suwon and Seoul, Korea
21. S.Kim, H. Hur, W.Kang, W.Kim, H.Jeon. Effects of early oral feeding on surgical outcomes and recovery after curative surgery for gastric cancer patients: pilot study results. Department of Surgery, St. Mary’s Hospital, College of Medicine, The Catholic University of Korea.
22. Zhang Xiangwen, Liang Huaizhu, Yu Jinning, Zhu Shibin. China Practical Medical Journal May 2009, Vol 4. No 4. Da Lian City Centre Medical Hospital General Surgery Department.
23. Singh N, Sharma B, Sharma M, Sachdev V, Bhardwaj P, Mani K, Joshi YK, Saraya A. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: a noninferiority randomized controlled trial. Pancreas. 2012; 41:153-9. Doi:10.1097/MPA.0b013e318221c4a8.
24. Cleary PD, Greenfield S, Mulley AG, Pauker SG, Schroeder SA, Wexier L, et al. Variations in length of stay and outcomes for six medical and surgical conditions in Massachusetts and California. J Am Med Assoc 1991 Jul 3;266(1):73-9.
25. Greenfield S, Apolone G, McNeil BJ, Cleary P. The importance co-existent disease in the occurrence of postoperative complications and one-year recovery in patients undergoing total hip replacement. Med Care 1993;31: 141-54.
26. J Bauer, S Capra and M Ferguson. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. European Journal of Clinical Nutrition August 2002, Volume 56, Number 8, Pages 779-785
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medical"
The word Medical refers to preventing or treating injuries or illnesses, relating to the study or practice of medicine. Medical care involves caring for a patient and helping them through their journey to recovery.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please: