Specific Care Needs of the Older Person with Dementia
Info: 7365 words (29 pages) Dissertation
Published: 15th Dec 2021

Introduction
This project is about exploring the issues for a person who suffers with the chronic illness Dementia. In this project I will define Dementia and research the different types and illustrate worldwide statistics. I will give an account of the physiological and psychological changes that occur for an older person with Dementia. I will elaborate and explore the different needs in relation to the individuals with dementia. I will research and explore the role of the carer and the multidisciplinary team in assisting a person with dementia. I will examine, explain and give examples of what practices need to be implemented in the professional care of a person with dementia. I will research and explore what care settings are now available for persons with dementia. I will state, explain and give examples of the current approaches towards developing quality services for people with dementia. I will research, explore, and source information for this project from class discussions, class notes, websites and multimedia. I will include a summary and bibliography reference page listing the resources of all information and research for this project.
Q1. What Dementia is and the physiological and psychological changes that occur for the older person with dementia
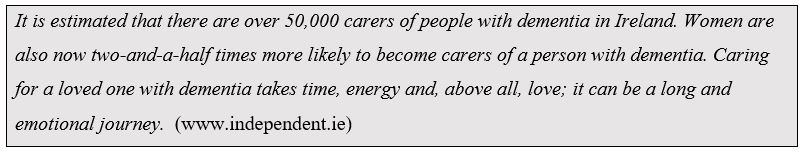
Dementia itself is not a disease it is actually an umbrella term which describes a range of conditions which cause damage and affect the cognitive and sensory parts of the brain. It affects a person’s thinking, the way they understand, feel, speak and behave. Although the majority of people with dementia are over 60 years of age, the condition is not a normal part of old age. Presently in Ireland there are over 55,000 people living with the condition. It’s expected to treble in the next 35 years. Over 4,000 Irish people are diagnosed with the condition every year. 63% of people with dementia live at home.
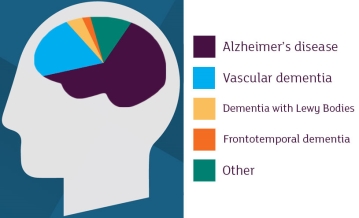
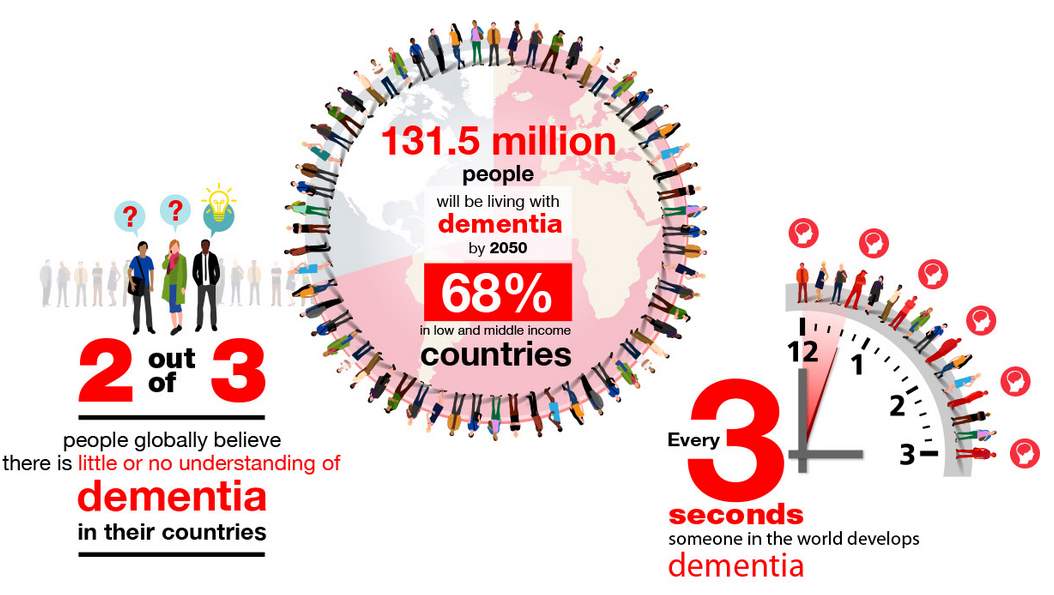
There are different types of dementia that can lead to different experiences and problems for the individual that is diagnosed such as Vascular dementia, Multi-infarct dementia, Lewy body dementia, alcohol-related dementia, Frontal-temporal dementia and Alzheimer’s. Alzheimer's is the most common and well known form of dementia; it is thought to cause over 50% of all cases. It is an incurable, degenerative disease. The early signs are not immediately obvious and are quite subtle. Typically people first seem to notice problems with their memory, difficulty doing everyday tasks, forgetting recent events, misplacing things, appointments, bills etc. The number of people living with dementia worldwide is currently estimated at 47 million, It is projected to increase to 75 million by 2030. The largest increases in dementia expected over the next 20 years are in places like China, India and Sub-Saharan Africa. Dementia is a major global health issue, affecting over 46.8m people worldwide.
Physiological changes that occur for the older person with dementia
As a person gets older there are many physical changes that their body will go through. However, a person with a type of dementia will experience some of these changes differently. They can have difficulty mobilizing and coordinating movements. This condition called Motor Apraxia, can develop into stiff, jerky-like movements, as it progresses, resulting in trips, slips and falls. Another example is the person may not be able to tap fingers in alternation or tinkling fingers smoothly on the edge of the table any more. Very commonly people can have difficulty with dressing themselves (Dressing Apraxia), forgetting the order clothes are worn. Problems associated with earlier signs of types of dementia are such things as difficulty recalling familiar names, words and numbers. Difficulty in finding the right word to identify an object leading to hesitant speech style, this is known as “Anomia”. In "The Case of Anna H." who had anomia, the neurologist/writer Oliver Sacks noted that: "When I showed her some kitchen matches, she recognized them at once, visually, but could not say the word 'match,' saying instead, 'That is to make fire.'" (www.medicinenet.com)
As a person reaches later stages of Alzheimer’s disease, problems can arise regarding eating and swallowing their food. In these stages they may forget how to chew altogether and require tube feeding. Often “food-pocketing” occurs, where they pocket food in their cheeks or under their tongue, which can lead to high risks of choking. The carer may put more emphasis on easy-to-swallow, pureed meals. There are several aids on the market for people with feeding issues, to aid judgement of food and appropriate bite size and to present a prescribed, manageable amount of food to the person.
Agnosia is a term used where the person lose their ability to process sensory information, recognize “familiar” objects, places or faces. They can forget what a particular object is used for. e.g. how to use a knife and fork, comb, using toothpaste to shave instead of shaving foam, mixing up left from right, A language impairment called Aphasia, affects a person’s ability to speak or comprehend or utilise what is being said. They have great difficulty responding and completing sentences. People with aphasia have difficulty putting words together or using normal grammar.
Another Physiological change that impacts on older people with dementia is to experience sleep disturbances. They can become confused as to if its day or night time. Their body’s circadian rhythm (body-clock) is mixed up. They are prone to getting up, wandering around, frequently asking or searching for food. This leads to apathy, irritability, excessive day time napping. This can be very difficult and tiring, not just for them but for the carers too. A decline in personal hygiene can occur, forgetting their clothes are dirty after they are removed, impaired ability to make judgments, neglecting to bathe, wash and take care of their personal hygiene. They will then be dressed in soiled clothing and have unpleasant body odour. Changes in eating habits as people can forget to eat or over eat leading to weight loss, weight gain, obesity, forgetting to swallow (food pocketing). Constipation can be caused due to lack of exercise and reduced mobility, effects of medication, and weakening of bowel muscles. Many people with dementia will experience incontinence, double incontinence, an overactive bladder. Women are prone to more frequent urinary tract infections. Incontinence in older people is associated with reduced mobility, declining cognitive function, decreased bladder capacity, reduced bowel muscle tone, poor nutrition and medication.
Psychological changes that occur for the older person with dementia
A person’s memory is affected, they forget names of objects, people and places and recent events. Procedural memory is a part of the long-term memory that is responsible for knowing how to do everyday things, commonly known as motor skills. People lose the ability to correctly sequence tasks, forgetting some of the steps in tasks they would have always done, e.g., cooking, laying a table, brushing teeth, making a cake, tying laces, and shaving.
People with types of dementia can be confused and be disorientated in time in space, have difficulties recognising people and objects. Their “internal body clock” which enables people to know approximately when it is time to eat or sleep is disrupted due to changes in the brain. Some nursing homes have adopted a plan where the carer team can wear pyjamas, bed clothing on their nightshifts. “Since most residents have dementia in some form, coming across a member of staff at night in ordinary day clothes could be disorientating.” “Staff have been wearing the night attire for several weeks and reported it has had a positive effect in promoting sleep at night, especially with the more restless residents” “When night staff assist residents to bed the residents have asked if the staff are off to bed too. Carers reply with ‘yes, but we are here for you anytime throughout the night if you need us’.” (www.gazettelive.co.uk)
People have diminished social awareness and may be prone to inappropriate behaviours, interrupting conversations, taking food from another, entering other people’s rooms. They lose the ability, without prompting, to start and follow conversations, leading to agitation and confusion. Misplacing things is common, putting objects in wrong places, difficulty finding familiar objects and not being able to remember where to locate things. This can lead to mood swings. They can get easily frustrated by their loss of abilities, and become suspicious and paranoid, suspecting a spouse or partner of infidelity is very common, accusing people of stealing and dishonesty.
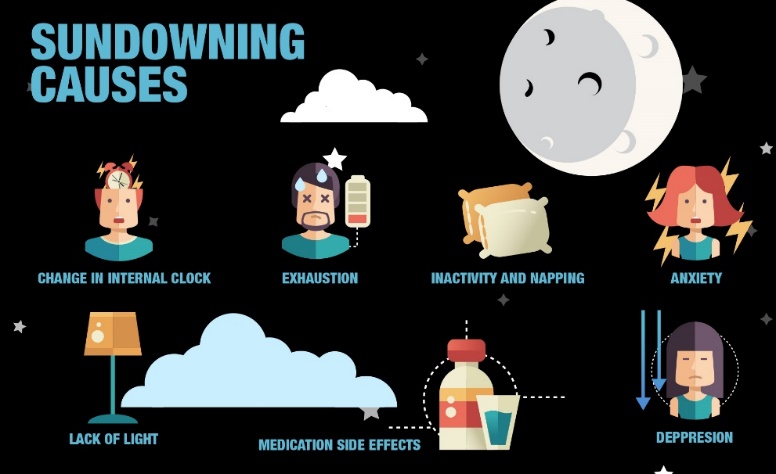
“Sun downing” happens in the late afternoon and going into the early night, where a person with Alzheimer’s and other dementias become confused and agitated, they start to walk and pace continuously “Exit seeking”. This hyperactivity can produce hazards such as slips, trips and falls, wandering, confusion and aggression that may cause serious injuries. Rummaging, also called seeking, happens in mid- to late-stage dementia, e.g. when people with dementia are hungry or accustomed to being busy, but they can no longer communicate, they rummage. They become anxious and agitated so rummage bags or boxes can be used for distraction. They are filled with various safe objects like stuffed animals, playing cards, magazines and photographs. They can ease anxiety for people with dementia but should be always used under strict supervision. “Studies of nursing homes have shown that a high number of harmful incidents occur between 6 and 8 p.m.” (www.kindlycare.com)
Other Psychological changes that occur for the older person are repetitive behaviour, some examples are packing, unpacking bags, making and unmaking beds, moving furniture, rearranging cutlery, Delph, folding and unfolding cloths. The constant questioning over and over again is due to the inability of the individual to retain information, they have forgotten that they have just asked that question, nor do they recall the answer. This is created by the stress, anxiety and fears that are produced due to this loss. e.g. “Where you going”, “Where’s my baby?” etc. Perseveration, repetitive movements and phrases are common. All these behaviours may be caused by discomfort, an expression of emotion and a release of frustration.
Sometimes a person with dementia can lose their inhibitions because of damage to the frontal lobes in the brain, and may behave in ways that others may find embarrassing. This can include being rude, racist, undressing, urinating, inappropriate sexual advances, genital stroking. Some causes include needing the toilet if they are touching themselves, being too hot by undressing, boredom, sexual frustration or wanting to talk to someone. Confabulation can occur, inaccurately recalling events, spontaneously producing false memories. They are not lying; the patients are unaware that their memories are not accurate. Dementia can affect how an individual perceives the world. They may experience hallucinations and start seeing or fearing someone or something that does not exist. Black or dark areas may seem like holes in the ground. A strategy used to discourage wandering is to put a large black mat or rug in front of a door. Some people with dementia will see this as a large hole in the ground, and stay away from the door.
Q2. The persons needs in relation to the condition
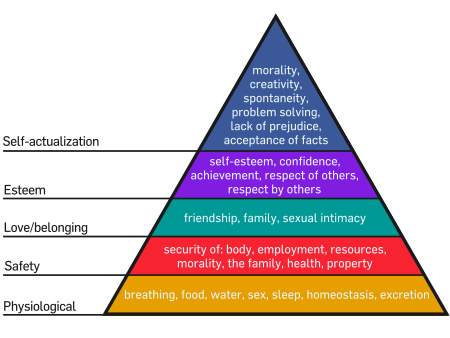
Maslow's hierarchy of needs
This pyramid demonstrates the basic way our bodies prioritise needs. The most basic needs are at the bottom, and the most highly evolved needs are at the top. Our strongest impulse is to survive. There are many different types of specialized needs a person with a form of dementia may need, The following are just some examples:
Physical needs require assistance with mobility if Apraxia is evident, due to the high risk of slips, trips and falls and referred to an occupational therapist for assessment for mobility aids, and to the physiotherapist for physio to maintain mobility, help with language and communication problems for the individual is referred to the SALT (speech and language therapist). SALT’s also assess clients with difficulties swallowing.

Communication is very important with a person with dementia as their ability to verbalise and understand their environment is challenged. It’s important to make eye contact with the person and call the person by their name and to get their attention, speak slowly and clearly check for understanding. Paraphrase and break instructions into small steps, so as they are better able to follow. Gestures are used unconsciously used by every human being, so use gestures and observe body language and their body language. Communication can be aided by sign boards if necessary. The “hand-over-hand method" can gently guide them to the activity at hand while still involving the client.
Routine and structure is extremely important for a person with dementia, as they "thrive on familiarity," as routine helps ground them, and promotes feelings of security, as it is easier to remember what happens during the day, leave things in the same place, adhere labels, pictures on cupboards, so they can locate and identify items more easily. e.g. labelling jars, coffee, salt, visual aids like these help the individual put things away in their proper places. Labels help minimise hesitation and confusion. A person may require assistance with some or all activities of daily living (ADL’s) may be required, depending how advanced their condition is.
If dressing apraxia is present, assistance with dressing will be required, laying out their garments in the order they are put on, or modelling the order helps the client involved. A person’s general and personal hygiene regime can be implemented as poor hygiene can cause skin complaints and infections. Incontinence is very common in dementia, if it is present a regular toileting programme is essential to insure comfort, reduce embarrassment prevent urinary tract infections (UTI’s) occurring, especially in female clients. If soiling occurs, clothing should be changed immediately. The person must should be washed and dried to promote positive self-image, eliminate unpleasant odours and maintain skin integrity.
Social needs are very important for socialisation and maintaining relationships, which are essential for human well-being for a person with dementia, whose memory and understanding is impaired, keeping them socially stimulated and involved is imperative. Encouraging, supporting and assisting a person in the social environment provide stimulation, promotes inclusion, maintain social skills and help prevent isolation and loneliness. “Looking at Maslow’s hierarchy of needs it is recognised that once the lower need is satisfied, a person focuses on satisfying the higher needs of love and belonging, self-esteem and self-actualisation”. (www.dementiapartnerships.org.uk)
Activities are necessary to prevent withdrawal that occur as dementia progresses and should have purpose and meaning. It is important to find out the persons interests, hobbies, former occupation, likes and dislikes. Based on this assessment an individual and unique social plan can be developed. It is important to include the person as much as possible in creating the plan. Activities such as reminisces, sing-songs, pet therapy, doll therapy, bingo, watch family videos, painting, napkin folding and card games can all be beneficial to help divert and distract a person who is “sundowning” or is exhibiting challenging behaviour, these activities also help cognitive function. Certain activities may work better at different times of day.

A person with dementia requires a familiar environment, structure and routine. It is very important that family relationships are maintained and that they are involved in the care of the person. Maintaining the individual at home and in their community is the preferred option and with valuable knowledge and information families can assist the person to stay active and involved in their (ADL’s). If the person is in a care setting / nursing home, staff should communicate to the family the importance of regular contact and give encouragement for them to assist when activities are scheduled. A person may need to be reminded and assisted with activities. It is not important if the activity is not done well. Never judge, other than to appreciate the process and result, what is important is that the person is active and involved. If trying to encourage someone to do an activity it could be worth phrasing things in such a way that the person knows they will be helping you, e.g. “It would be a great help if you could…” ensure they know what a big help they have been, boosting a person’s confidence. People should be allowed to engage at their own pace, not rushed and allowed sufficient time to complete their tasks with adequate lighting and with distractions kept to a minimum. Dementia can cause the older person to withdraw from activities, family and friends, inside is a person who is perhaps struggling to be heard or listened to, which is why looking after their cognitive needs are important. Things of personal value that they have an attraction to, promotes feelings of familiarity, security and comfort.

People who Hallucinate and have delusions may need the help of medication. It is important not to contradict a person about their perception of reality, enter their reality, their world, “build a bridge” to a person’s past, where they are now. A person with dementia can benefit from many therapies e.g. Reminiscence therapy, music therapy, doll therapy, dog therapy and various other sensory stimulants. These therapies are all ways of stimulating and engaging people with dementia, especially when verbal skills and their touch with present realities are diminished. Agitation is reduced and positive changes in mood are promoted.

Emotional needs are important to be supported with people with dementia, who are aware of their loss of ability to remember, communicate and function feels a variety of emotions, anger, grief, frustration and depression. They are facing the loss of their identity, security and independence. They fear the unknown, how the illness will impact on them, how severe the symptoms will be or what will be the length of time it will take the illness to progress after diagnosis. It is important that they and their families should be educated and provided with information on the condition, its expected progression, the impact it has on an individual and all the therapies and treatments available to manage symptoms.
Support groups are available on the illness and people should be encouraged to join them to access support from people with experience of the illness and to share experiences. A person with dementia needs to be always treated with the upmost respect, dignity and patience. It is important to empathise with the person and to imaging what it must be like in “their” shoes it can be very difficult when we have no idea of how the condition can take hold. It is important to preserve identity, treat them as an individual, get to know their life story, their beliefs and values in order to meet their needs, and be very mindful of them. It is important to keep the person involved in their care to the maximum extent possible. Always include them in all decisions about their care. Provide choice, where possible and ask for preferences and opinions they may have. It is essential for care givers to understand the importance of non-verbal communication, using signs and gestures where a person may not be vocal. “According to research, people with dementia receive over 93% of their information about the world through non-verbal gestures” (samvednacare.com)
Carers should never assume that they know what a person wants or needs. Do activities and tasks “with the person”, not to the person. Always see the person, not the illness. This will help the person feel valued and that they matter. It is important to validate their many worries and concerns, to reassure them, to express feelings and do not belittle or dismiss them. It is very important to promote and encourage independence and positive self- image. Do not speak sharply or use pet names (elder speak) .Even though they have lost touch with reality, the person is still an adult and should be treated as such. is important. As the dementia progresses, many people develop behaviours that can be very challenging as a result of changes in the brain. This should always be seen as a form of communication, a person communicating a thought, feeling or discomfort. A person should not be challenged or punished for same also try to remember that these behaviours do not define the person, they are just an effect and part of the disease.
Therapeutic lying, a concept that is occasionally used for deliberately deceiving patients for reasons considered to be in their best interest. There are variations of therapeutic lying when using this approach from telling an innocent lie, to diverting attention to a pleasant memory. Lies that reduce suffering and stress in persons with dementia, who are unable to fully appreciate the cause of distress can be beneficial. Reduce the emotion e.g. sadness anger or anxiety, Assess the situation, and meet the need. This is known as the RAM framework. Older people with dementia still have many intellectual needs. Just because they are advancing in years does not mean they can no longer learn new things as well as become more involved in the activities around them. In recent years day care centres are combined with nursing homes. Research has shown, that when older people and small children who come in contact with each other, thrive. But this was not just about helping the older persons, the children enjoyed the large amount of attention too, young and old had more opportunities and occasions to develop their social and emotional skills.

Other intellectual needs are met by using clear door signs, large clocks, calendars, prompts, jigsaws, memory books. Memory aids are required to keep the person orientated and to reduce confusion. Signs on doors, labels on cupboards, drawers and message boards will maintain their skills for longer. Calendars and large clocks will help preserve cognitive function. Verbal reminders can be given using simple instructions to keep the person involved with their ADL’s. Avoid surprising or frightening the person, try to make eye contact before touching or speaking to them. It is important to never rush a person or take over, allow them to proceed at their own pace. Focus on the persons strengths, promoting feelings of purpose and self- worth. Surround the person with familiar objects such as pictures, ornaments, blankets.
Many people with a dementia condition experience changes and disturbances in their sleep patterns. Researchers and scientific teams do not completely understand why this happens. Those who have difficulty in sleeping tend to wander, be unable to lie still, or keep yelling and calling out. Sleep promotion and sleep routine is important as it is better to keep a person as active as possible and to prevent day napping, this enhances physical and mental well-being. The design of the patient’s room with a dementia condition should not have any type of light during night time, in order to not over stimulate the brain before bedtime. Everyone wants to feel loved or a connection to something, or someone; sometimes both. This is where attachment is very important. Persons living with dementia may lose track of conversation and activities very easily, so being mindful of their feelings of inclusion is essential. Comfort is important as well as having a person’s ADL’s requirements met, it might mean the right to have quiet time when they need it, be warm, clean and dry, hunger satisfied, to have a sense of closeness, and to able to bond with other people.
Q3. The role of the carer and multidisciplinary team in assisting the person with dementia

Carers and the multidisciplinary team (MDT) build a good relationship with the client. Building a relationship requires effective communication with the client and their families in order to provide the best quality care to a person, we must communicate in a manner that allows the client to express their needs and wishes. The individual’s needs and are the most important thing. The Carer / MDT must continually observe the clients condition and report any changes in clients condition. These must be documented and the care plan reviewed and amended as changes occur. When a client who may be confused and disorientated, It is important when caring to go to “their reality”. We must build a bridge in order to connect with them and understand their needs, interests, desires, capabilities and behaviours. e.g. if they were a post man who got up early in the morning, they may still get up very early and it’s useful that you know their history and have an understanding why they do this.
The Carer / MDT must be familiar with, and adhere to the care plan. A care plan summarises what care the individual needs. This aids direction as to how care is to be delivered to an individual. Carers / MDT’s must at all times protect the dignity of the client. Help them to be as self-managing as possible and respect the person’s right to privacy. They must refrain from using “elder speak” and address client by name preserving their identity. They should to the maximum extent involve clients in decisions regarding their care and provide choice with clothing, meals, activities. Being able to do this contributes to an individual’s good mental health, promotes autonomy and helps preserve skills. The Carer / MDT must provide a safe environment for the client. They must ensure aids and equipment are decontaminated, clean and in safe working order. They must adhere to safe working practices and thorough infection control polices e.g. hand hygiene, segregation of laundry, sharps disposal.
Multi-disciplinary teamwork is an essential and must work with the families, as they will require support from the moment of diagnosis and encouraging them to be involved in the persons care. They provide support and information to help alleviate worries and concerns and to comfort them. Communication within the MDT team is essential, both written and verbal. The MDT team must share information and co-operate with each other to provide quality care to clients. They assist clients with ADL’s, always getting the clients attention. Before commencing a task, they must explain to the client what they are about to do and ask for their consent. They assist the client only when necessary in order to maintain and promote independence and positive self- image. Carers and MDT teams working with Down’s Syndrome who also have dementia, should receive training in how to relate to people with a mental handicap. should have the skills and competencies to deal with both conditions and to work with the mental handicap services.
Practices that need to be implemented
The person-centred care approach (PCA) which was developed in the UK by Professor Thomas Kitwood, needs to be taken which is involving tailoring a person's care to their abilities, interests, history and personality. This ensures the individual remains the focus – not the illness. Management of challenging behaviour is very important; it should be seen as a form of communication by the person to express an physiological or psychological unmet need. This behaviour needs to be understood, When managing actively listen, and understanding the person’s emotions it should trigger the question, “Why is this happening in this person now?”
Never argue or verbally punish the person instead use diversion and distraction techniques instead. Training of staff with Management of Actual & Potential Aggression (MAPA) policies and skills need to be implemented. MAPA’s training covers verbal de-escalation techniques and how to professionally respond to strikes and holds in a calm way keeping everyone safe. There are various care settings for people with dementia such as nursing homes, respite care, home care, day centres, residential care units and acute hospitals (short term).
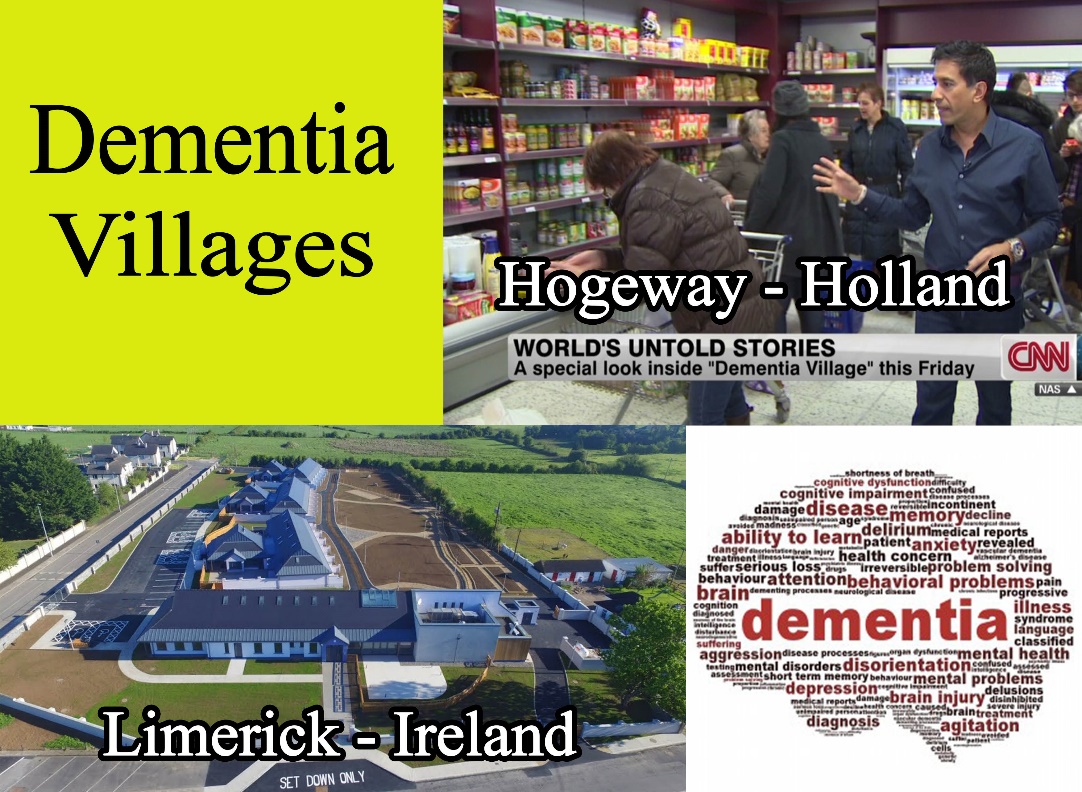
In the future, it is hoped that there will be a new concept of dementia specific units after the success of a purpose built cutting-edge elderly-care facility in a small village called Hogewey in the Netherlands. More attention to the design and scale of residential care settings and facilities for people with dementia has been a much neglected area in Ireland, However in the heart of a village called Bruff, County Limerick, work is currently in progress on the Countries first purpose built dementia community developed around a similar model. The community and care hub will comprise of 18 homes, each with a living room, bathroom, and private garden. They will offer a range of amenities including a café, gym, beauty salon, men’s sheds, and several gardens for all to enjoy. It is due to officially open Autumn 2017.
Q4. The current approaches towards developing quality services for people with dementia

In 2014 the government published the National Dementia Strategy. It identified areas of development to ensure future services for people with dementia would be designed and delivered to a high standard promoting public awareness and providing education and information on dementia is a key step in dementia care. This is necessary to Easing the stigma of the condition and widely publicise services available. Highlighting the risk factors for dementia is needed, such as poor diet, cholesterol, smoking, excess alcohol consumption, genetics and lack of physical activity. Early diagnosis is essential to ensure prompt interventions. The establishment of memory clinic across the country is required to facilitate early and accurate diagnosis. Ongoing staff development and training for all staff caring for people with dementia. Is vital to always ensure the maximum quality of care for clients. The development of community based services is required and supported by MDT’s in order to enable people to remain in their homes and community for as long as possible.
It is recommended that more support and education for family members is necessary in order for them to continue to care for their family member, to reduce them being stressed and leading to “burn out” The Establishment of dementia specific units is considered necessary in the delivery of quality care. Purpose built units, staffed by people with training in dementia care are necessary to meet the very specific and individual needs of a person with dementia. Many people with dementia are admitted to acute hospitals. It is recognized that the busy environment and lack of staff time and awareness regarding dementia imparts on the care received.

The implementation of initiatives to train staff in acute hospitals .The work of “Dementia Champions” is essential for managing the care of individuals in these settings. Dementia champions are the advocates for individuals with dementia and have excellent knowledge and skills in the care of people with the illness, they are a great source of information and support for their co-workers.
In 1999, a multi-professional group of researchers were formed from Ireland and other European countries, Called Interdem who collaborate together in research on and publicise, early quality interventions in Dementia. This just one of many of many teams of professionals and expert researchers who continue, to getting closer to one day discovering how they may effectively prevent and treat dementia. Provision of quality services are improving with the aid of better awareness, education and professional training.
Summary
In summary, I have defined what dementia is. I explored the issues for a person who suffers with the chronic illness Dementia. I have researched and named some of the different types of dementia and illustrated the current worldwide statistics on the condition. I have given an account of the physiological and psychological changes that occur for an older person with dementia. I have elaborated and explored the different needs in relation to a person with dementia. I have researched and explored the roles of the carer and the multidisciplinary team in assisting an individual with dementia. I have examined, explained and given examples of what practices need to be implemented in the professional care of a person with dementia. I have researched and discovered what care settings are available for persons with dementia. I have stated, explained and given examples of the current approaches towards developing quality services for people with dementia. I have researched, explored and sourced information for this project from class notes, websites and multimedia. In conclusion, this project was extremely interesting. The amount of people with dementia is increasing rapidly worldwide. People working with dementia patients need to have professional training and better understanding of the illness for their needs. The media and organisations involved with the support of dementia aid, are producing high quality information online and in printed material form, raising awareness of dementia and challenge the stigma that surrounds it. There is no cure at present, which justifies Carers and MDT’s upskilling and a worldwide approach regarding research and social interventions, aiming to minimize the impact of dementia.
Bibliography
alzheimer.ie. (2017). Types of Dementia. Available: https://www.alzheimer.ie/About-Dementia/What-is-Dementia/Types.aspx. Last accessed 08.11.17.
alzheimer-europe.org. (2009). Main characteristics. Available: http://www.alzheimer-europe.org/Dementia/Alzheimer-s-disease/Main-characteristics-of-Alzheimer-s-disease/Physical-changes/(language)/eng-GB#fragment1. Last accessed 7.11.17.
alzheimer-europe.org. (2017). Disorientation. Available: http://www.alzheimer-europe.org/Living-with-dementia/Caring-for-someone-with-dementia/Memory-and-Communication/Disorientation. Last accessed 06.11.2017.
alzheimer-europe.org. (2017). Sexually inappropriate behaviour. Available: http://www.alzheimer-europe.org/Living-with-dementia/Caring-for-someone-with-dementia/Changes-in-behaviour/Sexually-inappropriate-behaviour. Last accessed 05.11.2017. alzheimers.org.uk. (2017). Behavioural difficulties. Available: https://www.alzheimers.org.uk/info/20029/daily_living/10/eating_and_drinking/7. Last accessed 10.11.17.
alzheimersresearchuk.org. (2017). Behavioural and psychological changes can occur before memory problems in dementia. Available: https://www.alzheimersresearchuk.org/behavioural-and-psychological-changes-can-occur-before-memory-problems-in-dementia/. Last accessed 09.11.2017.
aphasiaireland.ie. (2017). What is Aphasia?. Available: http://aphasiaireland.ie/?page_id=335. Last accessed 09.11.17.
Botek,A M. (2017). Why a Daily Routine is Helpful for People with Dementia. Available: https://www.agingcare.com/articles/daily-routine-for-people-with-dementia-156855.htm. Last accessed 07.11.2017.
Class and Tutor notes – Creative Training 2017 dementiaguide.com. (2017). Physical Complaints . Available: https://www.dementiaguide.com/symptomlibrary/physicalchanges/?pageContent=physical_complaints. Last accessed 07.11.17.
dementiapartnerships.org.uk. (2009). Psychological and social needs. Available: http://www.dementiapartnerships.org.uk/archive/workforce/learning-pathway/step-3/3-psycho-social-needs/. Last accessed 07.11.2017.
freealzheimers-support.com. (2007). Inability to chew is Symptom of Late Stage dementia. Available: www.free-alzheimers-support.com. Last accessed 09.11.17.
Guillot,T. (2017). Why is a Teesside care home making staff come to work in their pyjamas?. Available: http://www.gazettelive.co.uk/news/teesside-news/teesside-care-home-staff-making-13365444. Last accessed 07.11.2017.
hospicefoundation.ie. (2009). Loss and Grief in Dementia. Available: http://hospicefoundation.ie/wp-content/uploads/2016/07/Final-Guidance-Document-3-Loss-Grief.pdf. Last accessed 08.11.2017.
Irish Independent. (2016). 15 facts about dementia. Available: https://www.independent.ie/life/health-wellbeing/health-features/15-facts-about-dementia-35054668.html. Last accessed 08.11.17.
James, I. (2017). Meet need(RAM) framework . In: Ian Andre James Understanding Behaviour in Dementia that Challenge. 2nd ed. LONDON: Jessica Kingsley. p111. Leiguarda,R. (2009). Learn more about Apraxia. Available: http://www.sciencedirect.com/topics/neuroscience/apraxia. Last accessed 09.11.17.
media.bupa.com. (2017). Alf always delivers. Available: http://media.bupa.com.au/alf-always-delivers/. Last accessed 03.11.2017.
medicinenet.com. (2017). Medical Definition of Anomia. Available: https://www.medicinenet.com/script/main/art.asp?articlekey=21580. Last accessed 09.11.17.
memorylossonline.com. (2006). Glossary Confabulation. Available: http://www.memorylossonline.com/glossary/confabulation.html. Last accessed 10.11.2017.
SAMVEDNA. (2016). Verbal and non-verbal communication tips for dementia caregivers. Available: http://samvednacare.com/blog/2016/08/26/verbal-and-non-verbal-communication-tips-for-dementia-caregivers/. Last accessed 11.11.2017.
Shmid,J . (2009). Why is Activity Important?. Available: http://www.best-alzheimers-products.com/activities-for-alzheimers.html. Last accessed 05.11.2017.
Spencer-Scott,P. (2017). Dementia and Hygiene. Available: https://www.caring.com/articles/dementia-alzheimers-hygiene-problems. Last accessed 02.11.2017.
Sperber, M MD. (2015). Therapeutic Lying: A Contradiction in Terms. Available: http://www.psychiatrictimes.com/forensic-psychiatry/therapeutic-lying-contradiction-terms. Last accessed 10.11.2017.
Steel, T. (2016). Dementia Training: Tom Kitwood's Flower of Emotional Needs. Available: https://www.searchcarejobs.com/blog/dementia-training-tom-kitwoods-flower-emotional-needs. Last accessed 11.11.2017.
thecaresupport.com. (2012). Repetitive behaviors and the frustration they present to the dementia caregiver. Available: https://thecaresupport.com/repetitive-behaviors-and-the-frustration-they-present-to-the-dementia-caregiver/. Last accessed 09.11.2017
Thomason, C. (2012). Benefits of cognitive stimulation for people with dementia. Available: https://www.nursingtimes.net/clinical-archive/neurology/benefits-of-cognitive-stimulation-for-people-with-dementia/5051328.article. Last accessed 04.11.2017.
unforgettable.org. (2017). 5 reasons dementia affects sleep. Available: https://www.unforgettable.org/blog/dementia-and-sleep-problems/. Last accessed 07.11.17.
unforgettable.org. (2017). 5 reasons dementia affects sleep. Available: https://www.unforgettable.org/blog/dementia-and-sleep-problems/. Last accessed 07.11.17.
Wick,J. (2016). How to Communicate Effectively with Dementia Patients. Available: http://contemporaryclinic.pharmacytimes.com/chronic-care/how-to-communicate-effectively-with-dementia-patients. Last accessed 08.11.17.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Alzheimers"
Alzheimer’s disease is a neurodegenerative disease that causes a progressive decline in brain function, affecting memory, language, orientation, and reasoning. Symptoms usually begin mild and get progressively worse.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




