Health Needs Assessment for London Local Council
Info: 9490 words (38 pages) Dissertation
Published: 9th Dec 2019
Tagged: HealthPublic Health
This is a Health Needs Assessment(HNA) for a Local council in a London Borough X. For confidentiality purposes, all names and places will remain anonymous as required by the nursing and midwifery council (NMC, 2015). As a specialist community public health nursing (SCPHN) student, a HNA is going to be undertaken for this organisation where I am on placement. The purpose of this HNA is to explore social-economic factors, to understand the prevalence of health conditions within the organisation and how they impact on the community, to compare the figures with those of the other boroughs and national figures at large and to promote and protect the health of the employees and reduce inequalities. The project will also explore at how the health conditions can be improved to reduce sickness absence from work, it will also gather and analyse data to identify all the health needs and then focus on one key health need. HNA is an essential tool to inform commissioning and service planning, which critically provide evidence on how to reduce inequalities on a population as highlighted by (Cavanagh and Chadwick,2005). This shall be done through identifying broader determinants of health and points of intervention, drivers or root causes of health issues, then implementing interventions including health promotion and disease prevention programs. Local policies and guidelines, frameworks, legislations, Public health priorities, national statistics and initiatives will be explored and discussed. Implications for professional practice will be discussed, recommendations and supporting actions will be put in place
1627800
The public health Outcomes framework set by the Government highlights a comprehensive scope to improve and protect health during a life span and reduce inequalities (DOH, 2016). Borough X is one of the most cultural diverse areas in England. It has a population of approximately 206,500 which makes it the 7th smallest population in London. A significant population growth and changes in composition has been noted over the years, the population has increased by more than one quarter (26%) between 2001 and 2016 from 163,900 to 206,500 residents, an increase of 42,600 people. This is a greater percentage change than England which is (12%) or London (23%). Residents of Borough X continue to face significant health challenges. There are high rates of smoking, inactivity, overweight and obesity. 1 in 5 (19%) smokes, 1 in 3(32%) are inactive and 1 in 2(71%) are overweight or obese. This explains the main causes of deaths in Borough X coronary heart disease, stroke and cancer, it is important to raise awareness of the common risk factors of these ailments which are derived from bad lifestyle choices as observed by Association of Public Health Observatories (APHO,2013). The life expectancy for both men and women are the lowest in England. The average mortality rate for Borough X as compared to England is 225.3 from preventable causes and for England is 184.5, 106.7 from cardiovascular disease and 74.6 for England, 169.6 from cancer and 138.8 for England and 54.3 from respiratory disease and 33.1 for England (Marmot Indicators for Local Authorities in England,2015). More than 1in 4 residents are under 15 and almost 1 in 10 are 65+ this is available in the report by Joint Strategic Needs Assessment (JSNA,2017). The representation of other ethnic groups has also changed across the 17 wards of this Borough. The black African population has increased from 4% in 2001 to 15% in 2011 and is now estimated at 17%. 1n 2017, other white category from Eastern European countries has increased from 3% in 2001 to 8% in 2011 and to an estimate of 11%
1627800
in 2017, the population group of Indian, Pakistani, and Bangladeshi ethnicity combined they counted to 5% in 2001 and 12% in 2011 and are estimated to make 17% of the population in 2017 (JSNA, 2017).
The health of the people in Borough X is varied compared to the England average. About 29% of children live in low income families. This is the most deprived Borough according to the index of multiple deprivation(IMD) it is the twelfth highest IMD score in England based on 326 local authorities and third highest IMD score in London (ONS,2017). There are several indicators within the Borough that are below or worse than the rest of England such as: Statutory homeless was 7.5% compared to England which is 0.9%, children in low income families are 28.4% and England is 18.6%, long term unemployment is 6.0% compared to 4.6%, violent crimes is 23.1% and England is 13.5%. (PHE, 2016). According to the Joint Strategic Needs Assessment which was conducted in 2017 for this local authority led by the director of Public Health. The aim was to provide a shared evidence -based consensus about key local health and wellbeing outcomes and reduce health inequalities. Health inequalities within different areas of the Borough is an issue, it is a case of the affluent versus the needy. Government Policies such as the white paper saving Lives: Our healthier nation 1999 and Tackling Health Inequalities: 10 Years On 2009, vowed to tackle health inequalities, but the struggle is real, to eradicate these differences in health outcomes in the communities is proving hard. Tackling Health Inequalities:10 Years On, it is a report reviewing the developments in health inequalities from November 1998 when the Acheson report on health inequalities was published to November 2008 (DOH,2009). Health inequalities seems to be
1627800
complex issue 2 decades later nothing much has changed; drastic strategies need to be put in place.
The Joint Strategic Needs Assessment (2017) highlighted key priorities such as give every child the best in life, create fair employment and good work, ensure a health standard of living for all, create health and safe community. The aim is to achieve best possible outcomes and facilitating fairness and social justice to families and children. There is a significant number of children living in low income families in Borough X about 28.8 as compared to England 6.6. This leads to poverty because some families cannot afford the cost of living and are depending on means-tested benefits. Poverty can have a major effect on the health of families which can impact on their mental health wellbeing (JSNA,2017). There is a need to ensure that these children have a good start in life and are supported in developing healthy life styles (Marmot et al. ,2010). To combat poverty all the many interconnecting risk factors need to be overcome. According to the (DOH,2009) UK has the highest number of children living in unemployed households than virtually any other EU country. Correlation is not causation, although unemployment may be a factor for living in poverty there may be other reasons such as homeless, lone parent families, low income, poor education and overcrowding which can affect health in many ways. Overcrowding in a house hold poses the risk of air borne disease such as tuberculosis, which is highly contagious and there seems to be a rise of this in Borough X.
On the statistical data provided by the business analyst of the organisation as of December 2016, the total number of employees were 3566 excluding those who work in schools. In total
1627800
the organisation has over 7000 employees to serve its community. See Appendix 1; The breakdown of the organisation’s employees in percentages (3566). Of these employees 1413(39,62%) work part time. The Organisation has an in-house occupational health service (OH). The service offers a full OH remit providing health surveillance, new starter medicals, sickness absence management, immunisations and vaccinations. The OH team is made up of an occupational health physician(OHP), a physiotherapist, a counsellor, an occupational health advisor(OHA) and the administration team. The OH services are accredited with the SEQOHS award (safe, effective, quality, occupational health standards) and that means their service provision are up to the recommended standards. They work in collaboration with the Human resources department which aims to support managers and employees with issues that affects their wellbeing and performance at work. Hubley and Coperman, (2008) highlighted that work places influence our health in many ways, for instance; the presence of harmful substances, exposure to chemicals, dust, vibrating tools, unhealthy environments and many more. Likewise, toxic work environment can be corrosive to employees’ mental health.
On the contrary, work places can also positively influence the health of the employees in many ways. There is strong evidence base showing that work is generally good for the physical, mental health and well-being. This was reinforced by (Waddell,2006) work meets important psychosocial needs especially in societies where employment is the norm and it is central to individual identity, social roles and social status. Hence the provision of occupational health services at work place to minimise or prevent these occupational health
1627800
induced diseases or disorders. Health and safety at work 1974, plays a major role in occupational health field. Work place accidents, illness and incidence are preventable if health and safety is managed accordingly. Occupational health professionals help to improve and maintain health and wellbeing at work (Smedley et al. ,2013), Which is one of the essential ideologies of occupational health professionals to have an in-depth knowledge and skill on how to promote health and wellbeing at work. Health and safety at work Act 1974 made it clear that it is the responsibility of the employer to protect the health, safety and welfare of their employees (HSE,2008). Providing information and resources helps to improve people’s skills, capabilities and it gives them control over their own wellbeing (NICE, 2005). Healthcare initiatives within the work place must be to safeguard the health of the workforce, the business and the wider community’(Oakley,2008). This was also supported by (Black,2008) a healthy work place is designed to improve the health of those at work, so that everyone with the potential to work has the support they need to do so.
The feasibility of this project depends on both motivation and resources such as skills, budget constraints and time. The health needs assessment will provide information to map a way forward and will help to shape the organisation’s services according to the population needs. This was supported by Watkins and Cousins (2010) a detailed HNA is the foundation upon which commissioning of services will be constructed. The above was supported by (Hooper,2002), by reinforcing that, a HNA will help with resources allocation, agreed priorities, improvement of health and reduction of inequalities such as early child development and education, employment and working conditions.
1627800
As defined by Cavanagh and Chadwick (2005:3) Health needs assessment is a ‘systemic method for reviewing the health issues facing a population, leading to agreed priorities and resources allocation that will improve health and reduce inequalities’. It is an approach that ensures services and resources are used to improve the health of the population in the most efficient way. Harris (1997, p.15) also described HNA as a system that reviews ‘the potential for alleviation of any health-related issue against current services provision resulting in a shared rationale, priority setting and a plan for change’ and emphasised that, it is crucial to identify the need, the problem, the factors affecting its distribution and impact on people, who has the problem and what can be done to alleviate it. Based on this ideology if outcomes are to be achieved a broader knowledge and understanding of the targeted population must be obtained. This suggest the importance to understand the epidemiology needs as it will be used to identify the level of need within the population as indicated by incidence and prevalence of disease, and data to estimate the size and composition of the population (PHE,2017). It is fundamental to understand incidence and prevalence of diseases when conducting a health needs assessment because that will contribute in decision making when calculating the number of new cases observed in the case of incidence or the number of cases present in a population in the case of prevalence (PHE, 2017).
The Framework used has been adapted from (Tones and Tilford, 2001) workplace health assessment which covers the following; Organisation, Demographic data, physical Environment, Nature of work and Health and safety and Occupational health promotion. This will be a significant change from reactive service-driven assessments to a proactive and
1627800
needs-led assessment with the goal to improve the employees’ health needs. Assessments should be conducted in a needs-led rather than service-led manner (Worth, 2001). similarly, (Parry-Jones and Soulsby, 2001) highlighted that, needs-led assessment is the cornerstone of high quality care. This was also complemented by (Green and Tones, 2010) by highlighting that a need-led approach will improve the health of the targeted population and reduce inequalities. Some reports have highlighted inequalities including the Black report (1980), Dahlgren and Whitehead’s study (1991) this shows the gravity of the issue at hand and the need to act urgently. Through profiling health needs within the organisation key health issues are going to be identified. Some of the information that is going to help to achieve this; is by analysing the available sickness and absence data, annual reports, morbidity, health checks and social service profiles, employee assistance programme usage, occupational health data, demographic characteristics such as age, gender, occupational group, working hours and ethnicity. If collected and used appropriately data can give guidance to professionals in practice to help with decision making (Oakley, 2008). This will provide a foundation of the development plan for the organisation to influence developmental changes in the community.
According to the data compiled by the OH department from September 2016 – September 2017, some health issues have been identified such as stress at 30.1% which is higher compared to the neighbouring borough which has 18.4%, mental health issues at 18.0% and the neighbouring Borough which is 10.5%, musculoskeletal disorders(MSDs) 21% as to 22.5% for the neighbouring Borough, diabetes, cancer, coronary heart disease, obesity at 25% and
1627800 occupational injuries. Which is reflected by high mortality rates across the Borough in the community, if the mortality rates in the most deprived areas in the Borough were to reduce, life expectancy would increase for both men and women. Stress claimed the highest figures of cases recorded and MSDs was second on the list. There were some changes within the organisation which put a lot of pressure on the employees resulting in high sickness rates and absences from work. These were change of management, working hours, reshuffling of teams and area of working. Stress needs to be managed properly as it can affect individuals but also has a huge negative impact on the organisation because of low productivity and increased cost (ONS, 2017). There has been a dramatic increase in reports of stress in 2017 especially with teachers and office workers. It is clearly outlined by the statistic figures that stress has affected a significant number of employees between 2016 and 2017 and its impact is reflected on the sickness absence records and number of management referral cases. Mental health and musculoskeletal disorders are the two leading causes of sickness absence (PHE, 2017).
In the organisation they have a robust sickness and absence management system, managed between the occupational health department, line managers and the HR. However, according to the statistics provided; ‘to date in Great Britain work -related musculoskeletal disorders remains an ill health related condition that places significant burdens on employers and employees, accounting for 39% of all work- related ill health’ (HSE,2017). The organisation has a huge workforce from different work areas. There are office workers, school workers, caretakers, catering service, security service, gardener waste, refuse collection and adult social care to name but a few. The organisation has a health and safety team in place and it
1627800
fosters organisational structure that supports risk assessment. They also have injuries and dangerous occurrences reporting procedures and all other legislative and policies as required by the Health and Safety at Work Act 1974.
This project will focus on work- related stress as it is the main key health need for the population. Bearing in mind that there is work-related stress and social- related stress they both have impact on the employee’s health and work. In view of the above as occupational health professionals the social issues cannot be ignored when considering work and how it might affect the health of the employees. As stipulated by the Health and safety Executive Occupational health providers ought to work with individuals who are experiencing problems associated with work-related stress and helping them either to remain at work or return to work successfully. Work-related stress can aggravate an existing mental health problem. Making it more difficult to control. If stress reaches a point where it has triggered an existing mental health problem, it becomes hard to separate one from the other (DOH, 2003). Work-related stress accounts for the highest cause of sickness absence and productivity loss. Work-related stress has affected both male and female employees of all ages from as young as 20yrs old. In 2016, there were about 25,5% cases and in 2017 the number went up to 30.1%. Compared to the other two neighbouring Boroughs. The figures were also compared with the local hospitals and it is overwhelming that work- related stress is the leading cause of most sickness absences in both public and private organisations.
1627800
Correspondingly in a case study carried by (Hussey et al.,2012) where general practitioners(GPs) where reporting cases of work-related ill-health via an online web form. It was concluded that work-related sickness absence affected both private and public sectors though public-sector employees incurred more frequent sickness absence. In modern society health problems among the working population has a significant socio-economic impact (Nicholson,2017). This was acknowledged by (Waddell, 2006) by adding that, employment and social economic status are the main drivers of social gradients in physical, mental health and mortality. The most groups affected in the organisation were those working in catering, building cleaning, refuse collection, office workers and schools services respectively this information was from the organisation’s business analyst.
The information and data on Sickness absence records, management referrals and reviews plus the available statistics on Public Health England and other sources such as National Statistics Office (2017) helped with the selection of the key health need. Mental health illness is one of the main priorities on Public Health England to educate, give awareness and advocacy against stigma. Also, the HNA selection criteria was used which is in the Five Step Approach Frame work by (Cavanagh and Chadwick, 2005). The following were considered which is impact, changeability, acceptability and resource feasibility. And this has helped to narrow down the population on which stress had severe impact on office workers and school teachers.
1627800
Stress has been defined as, having trouble coping for whatsoever reason (MHF,2016). (Oxford dictionary) defined stress as, a state of mental or emotional strain or tension resulting from adverse or demanding circumstances, Health and Safety Executive defined stress as, the adverse reaction people have to excessive pressure or other types of demand placed on them, and the British Occupational Health Research Foundation, (BOHRF,2005) defined stress as a non-specific response of the body to any demand upon it, which results in symptoms such as rise in blood pressure, release of hormones, quickness of breath tightness of muscles, perspiration and increased cardiac activity. Stress can be conceptualised as a process involving an interaction between the individual and the environment that includes a stimulus or stressor, intervening variables and a response. As described by BOHRF (2005 stress is not necessarily negative, and some stress keep us motivated and alert. Conversely too much stress can trigger problems with mental and physical health particularly over a prolonged period. Long-term exposure to work stress has been linked to an increase risk of depression, musculoskeletal disorder and other debilitating disease (BOHRF, 2005). There is a strong correlation between high job stress, demands and symptoms of anxiety and depression.
Absence from work cost the UK economy about £14,9 billion of workplace illness and injury between 2015/16 (HSE,2016). Health and Safety Executive (2016) strongly stressed out that, about 82% in Great Britain accounts for both ill health and days lost from work related ill health. The Mental Health Foundation also reported that 12million adults consult their GP each year due to mental illness, much of it is stress related(MHF,2014). Minor illness remains the most common cause of short-term absence, followed by stress, acute medical conditions
1627800
and mental ill health continue to be the most common causes of long-term causes, but the most common causes of long-term causes are stress (53%), acute medical conditions (53%), mental health (49%), musculoskeletal injuries (44%) and back pain (35%) (CIPD, 2016). Mental health is the greatest single cause of disability as outlined in the ‘Green Paper Improving Lives’(DOH,2016).
The Health and Safety Executive (2016), emphasised that every organisation has got a duty to manage sickness absence effectively and ensuring that health and safety of employees is maintained always as reasonable as practicable. To monitor sickness and absence the Bradford Score is the tool mostly used by employers. It is used as a summary measure of sickness absence which combines information on both frequency and length of sickness- absence. When the employee exceeds the limit of 150 days in a period of 12months it then triggers. It is the duty of occupational health nurses to promote health and wellbeing (Black, 2008). That was argued by (Boorman, 2009) that staff health and wellbeing is not just the responsibility of Occupational Health Advisors, it is the responsibility of every single member of staff. As a result, employees must take reasonable care of their own health and safety and the safety of others as outlined in section 7 of the Health and Safety at Work (HSWA) etc Act 1974. Prevention of illness, promotion of wellbeing and early intervention is very important. If stress is not recognised early and left for too long can lead to health issues such as depression, anxiety, hypertension or stroke. On the social side of things might lead to long-term unemployment, poverty, low income, housing issues that may lead to homelessness in the community thereby putting pressure on the taxpayer, and these are some of the
1627800
indicators that are below standard pointed out in Borough X. The Public Health Outcomes Framework 2016-2019 their vision is to improve and protect the nation’s health. They have set 2 outcomes which are; to increase health life expectancy and reduce the differences in life expectancy and health life expectancy between communities(DOH,2016).
It is the role of the OHA to establish the real cause of sickness and identifying what reasonable adjustments can be made to allow the employees to return to work safely. This was supported by the Faculty of Occupational Medicine(FOM,2012) helping employees to stay in employment or facilitating a well-managed return to work in a supportive environment can be an important stepping stone to recovery from mental illness. Literature reviewed that, sedentary work, shift work, long working hours, increased job demands, and work-related stress have been associated with increased alcohol consumption, reduced exercise and unhealthy diet (Tsiga, et al., 2015).
The Office of National Statistics (2017) pointed out that stress can be a huge detrimental to health if attention is not given. Issues raised by the employees within the organisation were due to work pressures e.g. staff shortages, too much work and not enough time to do things, lack of support from colleagues and managers, organisational changes, role uncertainty and targets to be met. Employees were facing difficult situation that even if they don’t feel well they were forced to be at work. Nieuwenhuijsen (et al., 2010) highlighted that, trends such as increased work pace, higher skilled jobs and the increased information and communication
1627800
technology have been placing increasingly high demands on the mental functions of workers. Pindek and Spector (2016) reviewed that, organizational constraints at work usually inhibit or fail to support an individual’s performance therefore have negative effects on their wellbeing, further contrasted with several other stressors organisational constraints are the strongest correlate of anxiety, anger, depression and frustration.
Evidence also shows that productivity can be reduced through the lower level of performance of employees who are at work but experiencing stress or mental health problem, this is known as presenteeism (NICE, 2009). There is significant evidence to suggest that health behaviours may not only be product of individual choice but are also influenced by workplace characteristics (Tsiga et al.,2015). Statistics from Chartered Institute of Personnel and Development (CIPD, 2016) acknowledged that, nearly three quarters (72%) of employers reported they have observed presenteeism -people coming to work unwell in their organisations. Johns (2010) also defined presenteeism as showing up for work when ill. It can damage quality of working life, and lead to impressions of in competencies. On the other hand, while systemic reviews concluded that presenteeism is equally as burden to the employers, the exact amount loss cannot be determined because there is no measurement for it. Office of National Statistics (ONS, 2017) reviewed that, a recent report estimated that impaired work efficiency associated with mental health problems cost £15.1 billion a year, which is almost twice the estimated annual cost of absenteeism (8.4 billion). The overall median cost of absence per employee is estimated to be £554. The constrains faced by some managers, were not understanding the policy for example when to refer employees,
1627800
difficulties in complying with the policy to provide effective support and consoling because of tensions between these and other aspects of their work roles. It is important for managers to acknowledge their leadership, strengths, weaknesses and appreciate personal knowledge gaps to enable the best use of their qualities (leadership academy, 2011).
Promoting mental wellbeing of employees can yield economic benefits for the business or organisation, in terms of increased commitment and job satisfaction, staff retention and performance (NICE, 2009). More generally the relationship between work and health must be placed in a broader social context, work often brings a sense of identity fulfilment and self-worth (Hayes, 2002). Cases surrounding work-related stress have become of increased interest in recent years. Occupational health nurses are key part of the public health work force, they can recognise changes within society and in the work place, participating in healthy workplace developments(DOH,2003). Society depends on a healthy workforce and that protecting mental health is central to employee’s wellbeing. Occupational health nurse’s early interventions in work place is of high importance, it is a good practice when considering work place situations especially where poor working relationships need to be addressed (FOM,2012
In the organisation they do have a sickness absence management and health and safety procedures, were by the employees get to be referred by their managers to the Occupational Health department due to short or long-term illnesses. The Organisation has a policy on how
1627800
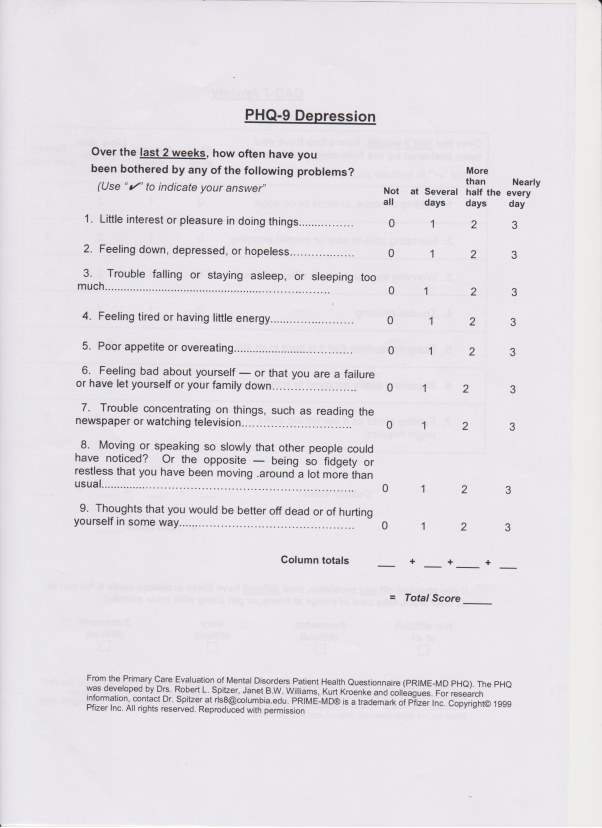
to prevent and manage stress which managers are advised to follow. OHA will give advice to employees, consider work demands or workload, the current capability of the employee, if they have control of what they do and to what extent? The managers are being encouraged to follow the stress risk assessment as outlined by the Health and Safety Executive Stress standards. Then they consider what support is available from the work place and if there are any adjustment that can be put in place or refer them to the Occupational Health Physician, physiotherapist or counsellor within the department if need be or signposting to other external health services such as GPs, Employment Assistance Programmes(EAP) which in confidence they cover issues like, work-life balance, workplace pressure, managing change, emotional wellbeing, life events etc. The is evidence from most of the stress cases recorded in the Occupational Health department are escalating to depression and anxiety causing long-term sickness. Currently the OH team do not use any screening tool for depression or anxiety. To improve practice and safeguard the health of the employees an intervention is going to be introduced.
Change is not always welcomed by everyone, it doesn’t happen overnight, and it is a process. Change can be defined as an attempt to alter or replace existing knowledge, skills, attitudes, norms and styles of individuals and groups (Wright, 1997). I discussed with my practice teacher about my proposal to introduce assessment tools for depression and anxiety PHQ-9 and GAD-7. There are several models and theories of change which have been developed over the years such as Appreciative Inquiry which is a relatively new approach for initiating or managing organisational change. It is a frame work developed for initiating or managing
1627800
change that focuses on positive personal and organisational attributes that may fuel change (Dematteo and Reeves, 2011). This model seeks to engage stakeholders in self-determined change. For this project the (Lewin model, 1958) is going to be used because it is simple and practical for understanding the change process. The change theory is made of three major concepts; driving forces, restraining forces and equilibrium. The driving forces facilitates change and the restraining forces hinders change and seek to maintain the status quo, whilst the equilibrium state that’s when neither the driving forces nor the restraining forces caused no change. Change can be stressful for individuals that might result in feeling resentful due to fear of the unknown or not understanding the change. The Lewin model is divided into 3 stages the unfreezing, change and refreezing. It is very important when initiating change to communicate with all the stakeholders involved so they may understand from the beginning. Rogers (2003) made it clear that when messages about the new change communicated within the organization this may bring uncertainty. It was important to identify the balance of power, know the key players involved in decision making and ways to influence those who might be against change. I had to consult my practice teacher she has been with the organisation long enough to know most of the stakeholders. Batras (et al.,2014), advocates that understanding the organisational dynamics and processes is very crucial for the development and success of health promotion initiatives. My practice teacher agreed and helped me to contact the people who would help me with the change. Focus of change efforts were to identify influential factors and selecting the strategies that can be applied to promote change. Acknowledging the systems, policies and guidelines that are already in place, the plan is more on improving what is already in place. This was the unfreezing stage where I had to create the case for
1627800
change give an awareness of the current existing issue at hand which was stress due to work-related pressures.
The immediate stakeholders were the OH staff and other staff such as line managers and HR advisors for schools, children services and public realm. To introduce change email were sent to other stakeholders for a briefing meeting. The meeting was held in the OH department and my proposal was to introduce assessment tools for depression and anxiety, I briefed them about the screening tools and warned them, that could have meant more paper work, and the administration staff needed to give more time allowance when booking appointments for the screening tool to be used. According to research evidence training in occupational health medicine may help to inform policy decisions targeting work-related stress exposures. I had to explain that, the additional paperwork were just two simple questionnaires one with 7 questions and the other one with 9 questions they are not diagnostic tools, but they will help us to identify those who are stressed and are susceptible to escalate into anxiety or depression. Then we would be able to signpost them for counselling services, to see the OHP or Senior OHA, their GPs and other external services for early intervention see appendix 2&3 for more information. PHQ-9 and GAD-7 are easy to use and can rapidly identify those who should be referred on for further evaluation to reduce sickness absence due to work- related stress. Stress is not a disease or illness but is a state which can increase the risk of many illnesses or disease particularly anxiety and depression, hence the introduction of the screening tool for early detection and intervention. Health and Safety Executive, (2017) also add on that there is a convincing evidence that prolonged periods of stress including work-
1627800
related stress is strongly linked to causation of anxiety and depression. Untreated mental health problems such as anxiety and depression, can lead to problems at work such as sickness absence, high staff turnover, poor interpersonal relationships, under performance and accidents which results in significant cost to the organisation (Miller, 1997). The rationale behind the introduction of the screening tools is to prevent, reduce and early detection of those who are prone to anxiety and depression for early intervention. Health and Safety Executive (2017) supports the view that preventive risk- assessment based approach would be more effective than case-based in achieving a National reduction in work-related stress.
The PHQ-9 and GAD-7 have proved to be very useful tools. In a research study by the Applied Health Science (2011) it was concluded that psychometric properties were generally strong in terms of internal consistency, convergent and validity. This is from a study they were assessing several screening tools for the validity in measuring severity of depression. A study conducted by Kroennke et al. (2001) reviewed that PHQ-9 is a reliable and valid measure of depression, the Test-retest reliability was excellent. GAD-7 has been found to be valid and efficient tool for screening and assessing severity of anxiety in clinical practice (Spitzer, 2006). After the presentation I gave about the proposal surprisingly it was welcomed by the OH team, line managers, HR advisors.
Now that everyone is aware of the change, the next step is to implement it. Health and Safety Executive, (2005) made it clear that when introducing a change in the organisation employees
1627800
must be provided with timely information to enable them to understand the reason for the proposed changes. Leadership academy (2011) emphasised that, group or collaborative change is thought to be more effective and successful than individual change. In Lewin’s theories of change he mentioned that, group decision making is powerful with respect to bringing about lasting behavioural change among group members. Parkins (2009) acknowledged that, communication is the key during this stage to inform staff about the imminent change, the rationale behind it and how it will benefit the employees. Education, training, communication and support are very crucial to execute the planned change (Parkins, 2009). We had another session with the OH staff only running through the paperwork again to make sure every member they have understood what was expected of them. We agreed that would do quarterly updates to make sure the change was beneficial. The first quarter proved to be a success from the massive positive feedback I got verbally and through evaluation forms, that there were easy and straight forward to use, and everyone was happy to implement the change. Hayes (2002) elaborated that, organisational change is typically associated with some degree of individual change, which is often the outcome of an informal and natural process of learning and development.
The final stage of refreezing was to make sure that OH staff were not going back to the old system and forget to use the tools or just to avoid because of extra paperwork, which will hinder the process of change. The culture of the organization determines its actions, as it is formed over time through shared experiences within groups, hence to embed change it needs to become cultural to yield positive outcomes (Schein, 2010) This stage reinforcement and
1627800
stability are the keys to sustain change. Efforts must be made to guarantee the change is not lost but needs to be cemented in the organisation to reduce work-related stress and sickness absence (Hayes, 2002). The expected outcomes of this initiative were to reduce determinants of stress, recognise early signs and symptoms of anxiety and depression and seek for early intervention. The HR gave us feedback that there was a significant drop on the number of sickness absence due to work-related stress. From the evaluation audit carried out the screening tools are proving to be beneficial, but change doesn’t happen overnight it is an ongoing process therefore, outcomes shall be monitored and reviewed continuously.
1627800
Reference List
Association of Public Health Observatories (2013) Health impact of physical inactivity.
Batras, D., Duff, C. and Smith, BJ. (2014) Organizational change theory: implications for health promotion practice. Oxford, University Press.
Black, C. (2008) Working for a Healthier Tomorrow. London, www.workingforhealth.gov.uk
Boorman, s. (2009) NHS Health and Wellbeing Review Interim Report. DOH.
Cavanagh, s. and Chadwick, K. (2005) The five steps of health needs assessment: Summary:
Health needs assessment at a glance.
Chartered Institute of Personnel Development (2016) Absence Management Survey. cipd.co.uk/absence management survey. cipd.co.uk [accessed on 20.01.2018]
Council for Work and Health (2016) Planning the future: Implications for occupational health; delivery and training. www.councilforworkandhealth.org.uk[Accessed: 22. January 2018]
Dahlgren, G and Whitehead, M. (1991) Policies and Strategies to promote social equality in health. Stockholm Institute of Future Studies.
Dematteo, D. and Reeves, S. (2011) A critical examination of the role of appreciative inquiry within an Interprofessional education initiative. Journal of Interprofessional care. (25), pp.203-208.
Department of Health (2003) A guide for Occupational Health Nurses: Taking a Public Health Approach in the Workplace. DOH.
Department of Health (2016) Improving Lives: The work, Health and Disability. Green Paper. London. The Statutory Office.
Department of Health (2016) Public Health Outcomes Framework 2016-2019. At a glance. www.gov.uk. [Accessed: 22. January 2018]
Faculty of Occupational Medicine (2012) Common work-related health problems: Guidance for health professional in primary care.
Green, J. and Tones, K. (2010) Health Promotion Planning and Strategies. 2nd edition
Sage Publications Ltd.
Harris, A. (1997) Needs to know: A guide to needs assessment for primary care.
Churchill Livingstone.
Hayes, J. (2002) Theory and practice of change management. Palgrave. Macmillian.
Health and Safety Regulation: a short guide (2003) Available at: www.hse.gov.uk[Accessed: 04 November 2017]
Health and Safety Executive (2016) Work Related Stress, Depression or Anxiety Statistics in Great Britain. www.hse.gov.uk [Accessed: 20 January 2018]
Health and Safety Executive (2017) Tackling Work-related stress using the management standard approach. A step by step book. Hse.gov.uk [Accessed: 31 May 2018]
1627800
Health Needs Assessment (2005) available at: www.nice.org,uk [Accessed: 29 October 2017]
Healthy Working futures (2017) Work place Health Needs assessment. Available at: www.gov.uk PHE Publications [Accessed: 27 October 2017]
Hubley, J. and Copeman, J. (2008) Practical Health Promotion. Polity Press, Cambridge UK
Johns, G. (2010) Presenteeism in the work place: A review and research agenda journal of organisational behaviour (31), pp. 519-542.
Kroenke, K., Spitzer, RL. and Williams, JB. (2001) The PHQ-9 Validity of a Brief Depression Severity Measure. Ge. Inter Med. 16(9) pp. 606-613.
Marmot Review (2010) Fair, Society, Health Lives. www.healthierlives.phe.org.uk. [Accessed: 19 January 2018]
Marmot Indicators for Local Authorities in England (2015)www.intituteofhealthequity.org. [Accessed: 19. January 2018]
Mental Health Foundation (2014) Mental Health Statistics. www.mentalhealth.org.uk [Accessed: 20. January 2018]
Mental Health Foundation (2016) Added Value: Mental Health as a Workplace Asset Report. Unum.co.uk [Accessed: 22. January 2018]
Miller, DM. (1997) Improving mental health in the work place. Occupational Medicine. (47), pp. 463-467.
National Institute for Health and Clinical Excellence (2009) Mental wellbeing at work, London.www.nice.org.uk [Accessed: 20. January 2018]
Nicholson, PJ. (2017) Occupational Health: the value proposition. Society of Occupational Medicine(SOM) London.
Nieuwenhijsen,K. Bruinvels,D. and Frings-Dresen,M.(2010) Psychosocial work environment and stress-related disorders, a systematic review. Occupational Medicine. (60), pp.277-286
NHS Leadership Academy (2011) Leadership Framework. www.leadershipacademy.nhs.uk/developing-yourleadership-skills/-framework/managing-services-overview/managingperformance [Accessed: 3 February 2018]
Nursing and Midwifery Council (2015) The Code of Professional Conduct. Available at: www.nmc.org.uk [Accessed: 10 November 2017]
Oakley, K. (2008) Occupational Health Nursing. John Wiley and Sons Ltd
Office of National Statistics (2017) Stress Policy Available at: https://www.ons.gov.uk
[Accessed: 8 November 2017]
Oxford Dictionary. en.oxforddictionaries.com [Accessed: 24 November 2018]
Parkins, P. (2009) Managing change in health care: Using action research. SAGE. London.
Parry-Jones, B. and Soulsby, J.(2001) Health and Social Care in the Community: Needs- assessment the challenges and reality. Blackwell Science Ltd.
Pindek, S and Spector, PE. (2016) Organizational constraints: a metanalysis of a major stressor. 30 (1), pp.7-25. Routledge Taylor and Francis Group.
Public Health England (2016) Health profile 2016. Available at: www.healthprofiles.info [Accessed: 09 November 2017]
Rogers, E.M(2003) Diffusion of innovations, 5th edition Free, Press, New York. NY
1627800
Schein,E.H.(2010) Organizational culture and leadership. Jossey-Bass, San Francisco,CA
Skokan, J.Nielsen, K. Borg,V. and Guzman, J.(2010) The impact of leaders on employee stress and effective wellbeing: A systematic review of three decades of empirical research. Work and stress. (24) pp.107-139
Smedley, J. Finlay, D. and Sadhra, S. (2013) Oxford Handbook of Occupational Health. 2nd edition. Oxford University.
Spitzer, RL., Kroenke, K. and Williams, JB. (2006) A Brief Measuring for Assessing Generalised Anxiety and Depression. The GAD-7. Arch Inter Med 166(10), pp.1092-1097. Doi: 10.100/archinter.16610.1092.
Tsiga, E. Panagopoulou,E. and D,. Niakas (2015) Health Promotion across Occupational Groups. One size does not fit all. Occupational Medicine. (65), pp.552-557
Tones, K. and Tilford, S. (2001) Health Promotion: Effectiveness, efficiency and equality. 3rd Edition Cheltenham, Nelson Thornes Ltd.
Waddell, G. and Burton, K. (2006) IS WORK GOOD FOR YOUR HEALTH AND WELL-BEING? The Stationery Office. London.
Watkins, D. and Cousins, J. (2010) Public Health and Community Nursing: Frameworks for Practice. Bailliere, Tindal, Elsevier, London.
Willson, F. and Mabhala, M. (2009) Key Concepts in Public Health. SAGE Publication. London
WHO (2001) The role of the Occupational Health Nurse in Workplace Health Management. WHO reginal office For Europe, Copenhagen.
Worth, A. (2001) Assessment of needs for older people by district nurses and social workers: a changing Culture. Journal of Interprofessional Care. (15) 3. University of Edinburgh, Scotland Uk.
Work-related Musculoskeletal Disorders(WRMSDS) Statistics (2017) Available at: www.hse.gov.uk [Accessed: 04 November 2017]
Wright, SG. (1997) Changing nursing practice. Edward Arnold. London.
APPENDEX 1
| Workforce Summary | |||||||
| Gender | |||||||
| Female | Full-time | Part-time | |||||
| 2,167(60.77%) | 1.002(28.10%) | 1,165(32.67%) | |||||
| Male | Full-time | Part-time | |||||
| 1,399(39.23%) | 1,151(32.28%) | 248(6.95%) | |||||
| Disability | |||||||
| Disabled | Not disabled | Not disclosed | |||||
| 152(4.26%) | 2,250(63.09%) | 1,164(32.64%) | |||||
| Ethnicity | |||||||
| Asian/Asian British | Black/black British | Chinese | |||||
| 207(5.80%) | 532(14.92%) | 13(0.36%) | |||||
| White | Mixed | Other | |||||
| 2,553(71.59%) | 62(1.74%) | 183(5.13%) | |||||
| Not disclosed | |||||||
| 16(0.45%) | |||||||
| Age | |||||||
| 16-19 | 20-29 | 30-39 | |||||
| 75(2.10%) | 452(12.67%) | 669(18.76%) | |||||
| 40-49 | 50-59 | 60-65 | |||||
| 954(26.75%) | 1,029(28.86%) | 301(8.44%) | |||||
| 66-74 | 75+ | ||||||
| 80(2.24%) | 6(0.17%) | ||||||
Appendix 2&3


Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Public Health"
Public health concerns the wellbeing and health of the general public as a whole. Through organised efforts, public health bodies look to inform the choices of society to help protect from threats to their health and prolong and improve the quality of life.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




