Mental Health and Substance Abuse Care Coordination Practicum
Info: 9195 words (37 pages) Dissertation
Published: 9th Dec 2019
Tagged: HealthMental Health
Critical Reflection: Mental Health and Substance Abuse Care Coordination Practicum
Table of Contents
Abstract……………………………………………………………3
Executive Summary……………………………………………………5
Practicum Experience Details…………………………………………….5
Location and Organization………………………………………..5
Mentorship…………………………………………………..6
Reflections on Practicum Experience Research…………………………………6
High Emergency Rooms Visits…………………………………….6
Hospital Readmissions…………………………………………..7
Healthcare Reform……………………………………………..8
Healthcare Costs Impacting the System……………………………….9
Affordable Care Act……………………………………………10
Development of Care Coordination Programs………………………….10
Care Coordination Programs……………………………………..11
Qualifications to be Enrolled……………………………………..12
Qualifications to Operate………………………………………..13
Critical Reflection……………………………………………..14
Theory and Concepts………………………………………………….15
Department Overview…………………………………………..15
Purpose and Scope of UBA Program………………………………..15
UBA Program and Goals………………………………………..16
UBA’s Role within the Structure…………………………………..18
UBA Staffing Models…………………………………………..18
Patient Access Center…………………………………………..18
Covered Services……………………………………………..19
Integration of IT………………………………………………21
UBA Success Data…………………………………………….23
Case Study………………………………………………….24
Critical Reflection……………………………………………..28
Changes in Practice and Conclusion……………………………………….29
References…………………………………………………………30
Abstract
This paper is based on the effectiveness of care coordination for mental health and substance abuse patients, as well as a critical reflection study of Montefiore’s University Behavioral Associates program. Healthcare costs are on the rise and improved care coordination must be developed in order to connect the healthcare care system to improve patient outcomes. Many mental health or substance abuse illnesses are often not addressed or detected properly leading to increased emergency room and inpatient admissions. The establishment of an effective care coordination program can lead to improved education, effective detection, and preventable re-admissions. Recommendations are presented for achieving high-quality care coordination for mental health and substance abuse disorders through the use of evidence-based quality improvement theories and concepts.
Executive Summary
The United States is facing a dilemma within the healthcare industry that is leading to devastating consequences in our populations health standards, costs and quality of care. The issues are caused by specific components within communities that correlate to several health-related conditions. A major contributing factor is a gap in care with patients exhibiting mental health and substance abuse disorders. In 2012, nearly one-fourth of adults in the United States
experienced some form of mental or substance use disorder (Heslin and Weiss, 2015). Healthcare organizations have taken notice, and are implementing programs to address these patient populations, and determining better ways to serve these patients that will lead to improved patient outcomes and quality of care.
Practicum Experience Details
Location and Organization
The type of organization I have chosen for the practicum option is a healthcare organization known as Montefiore’s University Behavioral Associates (UBA), located in Yonkers, New York. UBA is a division within Montefiore Health System, and manages the delivery of high-quality behavioral health services including clinical services at all levels of mental health and substance abuse care (Montefiore.org, 2016). The type of work I will focus on, is the care management outreach effort UBA performs for high risk mental and substance abuse populations in and around the area of New York. I have analyzed the current program within UBA known as Health Homes and researched how effective the program has been for patient outcomes, as well as determining if the model is sustainable for a new healthcare delivery system.
Mentorship
The Director of the Health Home program, Nelsy Hernandez, has served in a mentorship role throughout the practicum. Nelsy has been part of the initial development of the program and has worked with the organization for 20 years. Her experience and insight were vital to gain a greater perspective of the industry as well as a detailed review of the care coordination processes. The practicum project is an important aspect and a relevant topic in the field of healthcare. The following sections will describe the practicum research and experience in greater detail.
Reflections on the Practicum Experience
High Emergency Room Visits
A major factor influencing the rise in healthcare deficiencies are attributed to frequent visits to the emergency room leading to increased inpatient admissions. In a study conducted by LaCalle and Rabin (2010), it was discovered that patients frequenting the emergency room four or more instances per year accounted for 21%-28% of all emergency room visits. These types of frequent visits create an environment that debilitates the hospital and overutilizes vital resources within the emergency room.
The frequent utilization has shown commonality with the type of patients visiting more frequently than the average patient population. The high emergency room utilization patients, exhibit some form of mental health and substance abuse disorder coupled with homelessness, are uninsured and are often at low socio-economic levels (Bodenmann et al., 2014). In many instances the ED visit could have been avoidable and were often non-emergent. But with lack of resource and patient education, this patient population had few other alternatives to receive proper care.
Wiess et al., 2016, conducted a study to determine specific characteristics of the mental health and substance abuse population that frequented the emergency room; the findings are summarized below:
- The rate of emergency department (ED) visits per 100,000 population related to mental and substance use disorders (M/SUDs) increased substantially between 2006 and 2013. The increase over these 7 years was higher for mental disorders (55.5 percent for depression, anxiety or stress reactions and 52.0 percent for psychoses or bipolar disorders) than for substance use disorders (37.0 percent).
- The most rapid increases in the population rate of ED visits involving M/SUDs from 2006 to 2013 by age and sex were as follows:
- SUDs: women aged 45-64 years (50.2 percent increase)
- Depression, anxiety, or stress reactions: men aged 45-64 years (64.5 percent increase)
- Psychoses or bipolar disorders: men and women aged 18-44 years (56.7 and 61.6 percent increase, respectively) and men aged 45-64 years (59.2 percent increase)
- Between 2006 and 2013, increases in the population rate of ED visits involving M/SUDs were largest among those in the lowest income communities, with increases of 40.8 percent (SUDs) to 79.4 percent (depression, anxiety or stress reactions).
Hospital Re-admissions
Without adequate care coordination, hospitals are experiencing high readmission rates, especially with mental health and substance abuse disorder patients. This causes increased costs, reduction in resources and leads to negative health outcomes. Hospitals are now accountable for ensuring that their quality of care is improved and hospital readmission within 30 days of discharge usually represents a negative clinical outcome for patients with mental disorders (Heslin and Weiss, 2015).
In a study conducted by Feng et al (2017), it was discovered that the rate of mental health related readmissions (8.0%) was significantly higher than that for non-mental health diagnoses (6.2%, p<0.001). And of those readmitted within 30 days with a mental health diagnosis almost all (98.4%) were readmitted for a primary mental health diagnosis. Edelman (2016), identified four contributing factors that have led to readmissions:
- Premature discharge from hospital.
- Failure to relay important information to outpatient health care professionals.
- Lack of coordination when patient is discharged.
- Emergency department decision-making to admit a patient who may not have required an inpatient stay.
Healthcare Reform
Specific healthcare reform had to be developed in order to identify care gaps and improve the quality of the healthcare system. Many of the mental health and substance abuse disorders have the ability to be managed more effectively in an outpatient setting versus an emergency room or inpatient hospitalization. Case reviews found that the readmissions of 269 of 1000 patients (26.9%) were potentially preventable. More than half of these readmissions (140 of 269 cases, 52.0%) were determined to be potentially preventable because of “gaps in care during the initial inpatient stay (Edelman, 2016).” The new challenge facing healthcare is answering the question of how can the system adapt to managing patient populations more effectively in an outpatient setting?
Healthcare Costs Impacting the System
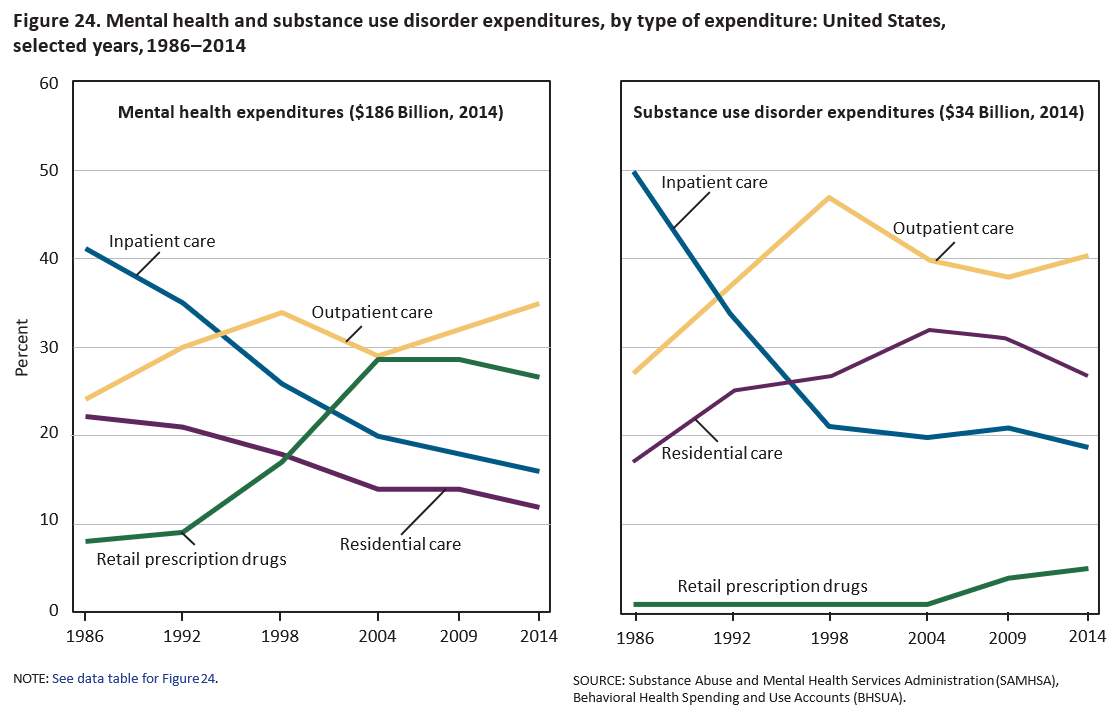
Mental health and substance abuse disorders are attributing to rising healthcare costs and over utilization of healthcare resources. The Center for Disease Control (2016) estimates that mental health and substance abuse expenditures combined, between 1986-2014, accounted for $220 billion dollars. Without proper reform in place, these costs will continue to rise.
Prior to 2014, one-third of those currently covered in the individual market have no coverage for substance use disorder services and 20 percent had no coverage for mental health services, including outpatient therapy visits and inpatient crisis intervention and stabilization (ASPE, 2016). Without adequate coverage, patients with mental health and substance abuse disorders had nowhere else to turn but the emergency rooms.
In a 2008, a survey of 328 emergency room (ER) medical directors, the American College of Emergency Physicians found that roughly 80 percent believed that their hospitals “boarded” psychiatric patients (Alakeson, et al., 2010). The emergency rooms are not equipped to handle mental health and substance abuse disorders often resulting in diminished care, repeat visits and readmissions.
Affordable Care Act
In 2014, The Affordable Care Act was enacted to expand coverage to patients with mental health and substance abuse disorders. The ASPE (2016) reports that it will expand coverage in three ways:
- Including mental health and substance use disorder benefits in the Essential Health Benefits
- Applying federal parity protections to mental health and substance use disorder benefits in the individual and small group markets
- Providing more Americans with access to quality health care that includes coverage for mental health and substance use disorder services.
Development of Care Coordination Programs
In response to the changing landscape of healthcare and the new healthcare reform act, a new process was developed and is known as the care coordination program. Care management is a criterion of goals that are set to assist patients and their support systems in managing medical and behavioral conditions to reduce readmission, improve patients’ functional health status, enhance coordination of care, eliminate duplication of services, and reduce the need for expensive medical services (Bodenheimer and Berry-Millett, 2009). When considering the impact that mental health and substance abuse patients have on the system, it is crucial for healthcare platforms to develop outreach efforts to better manage this patient population. Case management for psychosocial problems, homelessness, and substance abuse among frequent users may decrease emergency department use while improving patient care (Behr and Diaz, 2016).
The institute of Medicine Committee (2006) identified key areas of care coordination to address the mental health and substance abuse care management strategy:
- A shared understanding of goals and roles—Collaboration is enhanced by a shared understanding of an agreed-upon collective goal (Gittell et al., 2000) and clarity regarding each clinician’s role.
- Effective communication—Multiple studies have identified effective communication as a key feature of collaboration (Baggs et al., 1999)
- Shared decision making—In shared decision making, problems and strategies are openly discussed (Baggs et al., 1999) and consensus is often used to arrive at a decision.
Care Coordination Programs
There are three distinct types of care coordination: Inpatient care management, transitions of care coordination and Health Homes. The services that each type performs includes connecting individuals to screenings, following patients post-screening, and assisting patients through the course of treatment (Dohan & Schrag, 2005). It is important to understand how each type of care coordination functions in order to identify how mental health and substance abuse patients enter the outreach phases. The following is a summary outline by UBA:
Inpatient Care Coordination
When a patient enters the healthcare system through the emergency department and presents any type of mental health or substance abuse disorder, many hospitals have adopted a generalized process to move the patient through the appropriate plan of care. A physician first evaluates the patient and identifies the health issues. If a mental health or substance abuse disorder is identified a social worker is called in to further assist the patient. At this stage a psychiatrist is also consulted to determine if the patient will be discharged or admitted.
If a patient is discharged from the ED they are referred to outpatient mental health and the health home program is then discussed with the patient. If the patient agrees to follow up with a heath home provider, the patent signs a release and is given the appropriate contact information. If the patient is admitted, they are followed by an inpatient care team including the physician, psychiatrist and social worker. Once the patient is discharged, the same process is followed.
Transition of Care
During the discharge period, a care manager follows up with the patient within 24-48 hours to review the plan of care, follow up appointments, financial issues, transportation barriers and perform a medication reconciliation. If the patient meets the criteria for Health Homes, they are given further information regarding the program. This is crucial step in the care coordination process.
Health Homes
Under New York State’s approach to health home implementation , a health home provider is the central point for directing patient-centered care and is accountable for reducing avoidable health care costs, specifically preventable hospital admissions/readmissions and avoidable emergency room visits. This process provides timely post discharge follow-up, and improving patient outcomes by addressing primary medical, specialist and behavioral health care through direct provision. In addition this also involves thorough contractual arrangements with appropriate service providers, of comprehensive, integrated services.
General Qualifications to be Enrolled in a Health Home Program
According to the New York State Department of Health, the following guidelines must be met in order to qualify for services under the health home program:
- Two or more chronic conditions (e.g., Substance Use Disorder, Asthma, Diabetes*) OR
- One single qualifying chronic condition: HIV/AIDS or
- Serious Mental Illness (SMI) (Adults) or
- Serious Emotional Disturbance (SED) or Complex Trauma (Children)
General Qualifications to Operate as a Health Home
According to the New York State Department of Health, the following guidelines must be met in order to operate as a Health Home:
1. Health home providers/plans must be enrolled (or be eligible for enrollment) in the NYS Medicaid program and agree to comply with all Medicaid program requirements.
2. Health home providers can either directly provide, or subcontract for the provision of, health home services. The health home provider remains responsible for all health home program requirements, including services performed by the subcontractor.
3. Care coordination and integration of heath care services will be provided to all health home enrollees by an interdisciplinary team of providers, where each individual’s care is under the direction of a dedicated care manager who is accountable for assuring access to medical and behavioral health care services and community social supports as defined in the enrollee care plan.
4. Hospitals that are part of a health home network must have procedures in place for referring any eligible individual with chronic conditions who seek or need treatment in a hospital emergency department to a DOH designated health home provider.
5. Health home providers must meet the following core health home requirements in the manner described below. Health home providers must provide written documentation that clearly demonstrates how the requirements are being met.
Critical Reflection of Care Coordination Research
Researching into the field of care coordination has brought many forms of critical reflection on the current state of healthcare. Leadership and diversification will be an instrumental foundation into the success of any program that is developed and centered on patient population health management. Healthcare reform has changed the landscape of healthcare and new challenges will continue to arise.
Frameworks
Leadership. Transformation leadership is a style of leadership that incorporates both leaders and followers working together towards a common goal. This framework can assist in the care coordination concept as there are many differing teams involved in managing patient care. Another style of leadership that will impact the success of care coordination is servant leadership. A servant leader aspires to serve the community and people they belong to with a higher-level goal of inclusion for all. Being a servant leader brings a well-balanced approach to organizational design and establishes a strong sense of purpose with the team.
Diversification. Healthcare systems must create a diversification strategy framework into the business model in order to sustain the rapid changes in healthcare. Diversification strategy enables a company to enter new markets and incorporate new services and ideas. Diversification is key to healthcare systems and enables a healthcare organization to spread their services to a multitude of patient segments thus lowering risk.
Theory and Concepts
Integration of Montefiore’s University Behavioral Associates-Departmental Study
University Behavioral Associates (UBA) is a managed behavioral health organization committed to providing the highest quality management services for behavioral health care. UBA is the behavioral care management division of the Care Management Organization (CMO) and provides staff and systems support to the Montefiore Behavioral Care IPA (MBCIPA). UBA’s mission is to help providers maintain control over the system of care, ensure patient access to high quality behavioral health care, collaborate with providers in utilization management, maximize resources available for patient care, and minimize administrative costs. UBA is committed to assisting the MBCIPA while effectively managing the behavioral care service needs of patients. As part of that commitment UBA adheres to the following guidelines:
- Members have timely and easy access to mental health/chemical dependency services, which are provided by qualified professionals.
- A full range of mental health and substance abuse treatment services are available.
- Mental health/chemical dependency services are well coordinated with medical care.
- Prevention and early intervention are considered key for assuring optimal mental health of members.
Purpose and Scope of the UBA Behavioral Care Program
UBA’s purpose is to ensure that the behavioral health care provided to covered
members arecoordinated, appropriate, effective and efficient. Program activities are designed
to reviewutilization through a variety of control and oversight mechanisms. These mechanisms
include,but are not limited to:
- Establishing a referral process that ensures appropriateness whilepreserving access.
- Preauthorizing inpatient admissions and certain outpatient services
- Conducting concurrent review of admissions and continued hospital stays.
- Promoting and evaluating the appropriate use of emergency services.
- Providing for continuity of care through proper discharge planning and case management services.
Appropriate links between behavioral care and other aspects of medical care are an
important aspect of the behavioral care program. Effective utilization management is designed to promote the delivery of quality care, manage resources effectively, and to ensure that equal,
consistent and effective care is provided to all members across the network.
Behavioral Care Program Goals
The Goal of the program is to provide access on a 24-hour, 365-days-per-year basis to
appropriate levels and typesof Behavioral care services for members with behavioral care
problems. This includes the 24-houravailability of a psychiatrist to provide medical and
behavioral care management decisions on acase-specific basis.
- To develop and promote behavioral management standards of quality care and service.
- To ensure that behavioral health care services which are delivered to individual members are medically necessary and consistent with the diagnosis and level of care required.
- To ensure documentation of behavioral care management decisions and protocols utilized in the patient management record.
- To facilitate the coordination of behavioral care services with primary care physicians and other medical specialty services.
- To monitor utilization practice patterns of participating physicians, hospitals and ancillary service providers.
- To educate members, physicians, hospitals, and other ancillary health care providers about the goal for providing quality, cost effective management of health care and to inform about specific plan requirements.
- To ensure that health care services are provided by network providers unless out-of-network care is authorized by the UBA Behavioral Management Department
- To coordinate thorough and timely investigations and responses to member and provider inquiries and complaints which are associated with utilization issues.
UBA’s Role within the Care Management Organization Structure
UBA is responsible for utilization management on all CMO contracts. Behavioral care management is a subspecialty area of medical management and requires personnel trained in behavioral care for management and oversight. UBA is held to a very specific set of regulatory and health plan standards. These standards require collaboration with medical management and it is the goal of the CMO and UBA to work in collaboration on cases that require co-management.
UBA Staffing Model
In order to operate at an optimum level, the UBA team is comprised of a variety of roles
that work in a cross functional manner. This type of staffing model allows for enhanced patient care and experience for both the patients and providers needing access to the program. The staffing model is outlined below:
Utilization Management Care Coordinator. This part of the team deals with all the initial phone calls that come through by patients and providers. They play an essential role in the process as they are the first point of contact. In their process they draft an initial screening in order to determine if the patient either meets the requirements of care and where to delegate the case. They also answer questions and field provider messages as needed
Accountable Care Managers (ACM). There were a total of 11 ACM’s and each had approximately 60 patients they managed and worked exclusively with Health Home patients. There was an internal system in place to monitor each care coordinator to ensure they were meeting the goals of outreaching the patients.
Clinical Case Manager (LCSW). The clinical case managers are responsible for managing high risk cases and are also utilized as clinical consultants for the health home team. They play as a pivotal factor in ensuring patients receive quality clinical outcomes.
Operations Manager. Is responsible for the overall effectiveness of the UBA program and often deals with the IT component of the department to ensure smooth operations. The Ops Manager works closely with the health home team to ensure that compliance metrics are being met. In instances where the measures are not met, the Ops Manger would have one on one meetings to identify any barriers.
Project Manager. The project manager deals typically with all the payers to ensure that the program is meeting the necessary compliance requirements. The project manager also coordinates various meetings with other CMO departments regarding process improvements and IT updates. This is a key role within the department and allows information to flow smoothly.
UBA’s Patient Access
One of the primary differences in UBA’s behavioral care management is the fact
that members have direct access to mental health referrals 24 hours a day through a special toll
free line. Members, or others acting on their behalf, who request care do not require any referral from their primary care doctors to access a referral to a mental health or substance abuse provider. This establishes a direct link to services in an immediate and timely manner. Appropriate staffing is necessary to meet the demands of the patient population and UBA is committed to ensuring that quality standards are in place.
The clinical referral line sets the foundation of its service. The UBA staff determines what type of care may be needed at the time of a call and facilitates a referral to an appropriate mental health provider for the member. This referral process includes emergent, urgent and routine levels of care. The following information provides more specific and detailed information about the way in which the behavioral care division of the CMO operates.
Covered Behavioral Care Services
Covered services are specific to each health plan’s requirements. General behavioral care services include triage, evaluations, outreach, emergency care, individual psychotherapy, group psychotherapy, couples therapy, family therapy, psychiatric medication management, inpatient care, routine outpatient, intensive outpatient case management, complex case management and intensive case management. Specific health plans may also include partial hospitalization, detoxification, chemical dependency rehabilitation, ECT (both inpatient and outpatient ECT) and acute home care. A patient may be referred or self-referred for emergency care without pre-authorization. Medicaid members are entitled to self-refer to a provider of their choice of one mental health and one chemical dependency visit during each 12-month period.
Services excluded from mental health and chemical dependency coverage are: custodial care; treatment of mental retardation; weight reduction; acupuncture and acupressure; cognitive therapy for medical conditions; all services provided by primary care physicians; all laboratory tests and radiological services (unless bundled into a single per diem charge); transportation needed for medical reasons (covered under the medical benefit); biofeedback for medical conditions (part of medical benefit unless recommended by mental health provider); methadone maintenance; psychological testing requested by school system or to fulfill legal evaluation, or required by an employer or for vocational purposes (e.g., law enforcement) or to assess mental health and developmental disabilities; neuropsychological testing (may be part of medical benefit); treatment for military related disorders covered by government facilities.
Services for members with comorbid medical and behavioral diagnoses are determined based on place of service. The primary diagnosis that is causing the patient to remain in the current setting represents a general principle for determining behavioral health vs. medical benefit status. These cases are often comanaged by the medical management team and the behavioral care team.
Behavioral health services are based on medical necessity, which is defined as having a diagnosable DSM-V or ICD-10 disorder with sufficient impairment or likelihood of developing a disorder. While potential broader applicability exists, the following interim health home provider standards focus on serving the enrollees with behavioral health and/or chronic medical conditions and have not been specifically tailored for meeting the needs of the developmentally disabled or long-term care patient populations.
Integration of Information Technology to Enhance UBA’s Program
UBA utilizes information technology in order to properly track outreach efforts by the team. They built an internal customized productivity report that tracks all phases of the outreach process. According to the New York State Department of Health BAHN website, there are specific billing aspects that must be tracked.
Standards for Outreach
There is a 3-month billing period to outreach and enroll members in Health Home.
Health Home partners must demonstrate progressive and escalating efforts to engage the member. Mandatory minimum requirements for Outreach must be met; additional activities do not replace minimum requirements.
- Month 1 – Beneficiary Letter, Phone Call or face-to-face. (Note: if letter is not mailed it must be hand-delivered to member during face-to-face encounter; entered in portal as type of contact ‘mail’).
- Month 2 – Beneficiary Phone Call, and if unable to make direct contact, a phone call to Collateral Contact. Contact can also be face-to-face, but does not replace the mandatory phone call requirement.
- Month 3 – Face-to-face contact or a successful phone call.
The member’s outreach status is then pended for the next three months. The Health Home may continue their efforts to engage and enroll the member in months four through six; however, those efforts are not billable unless the member enrolls in the Health Home program during that period of time. At the end of the ‘off’ cycle, a new billable ‘on’ outreach cycle begins.
Example of 3-month on/off outreach cycle
Member assigned to BAHN Health Home on July 12 “On” outreach cycle:
- Month 1 (July): Mail Letter and Phone Call
- Month 2 (August): Phone Call and Collateral Contact if unable to make direct contact in month 1
- Month 3 (September): Face-to-face contact in the home or community if not successful in month 2
- If enrollment occurs, cycle ends
- If enrollment does not occur, member enters ‘off’ outreach cycle
‘Off’ outreach cycle:
- October to December: Can continue to outreach, but cannot bill unless enrollment occurs
- If enrollment occurs, outreach cycle ends
- If enrollment does not occur, member enters billable ‘on’ outreach cycle again (January to March)
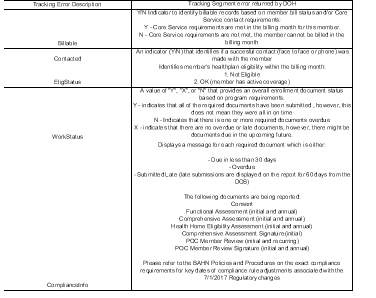
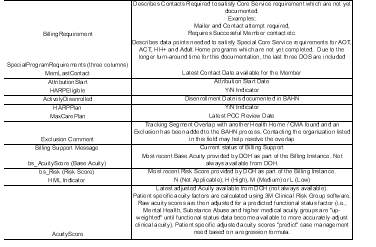
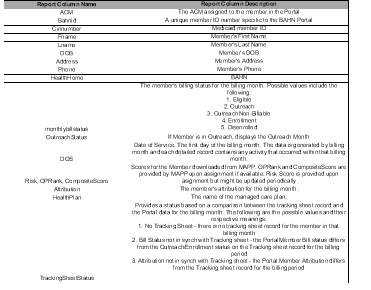
By utilizing the below customized report, UBA is able to track all of this information in real time to ensure compliance and standards are at an optimal level.
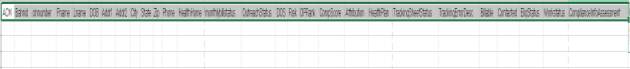
The following gives a breakdown of each column that is represented by the care coordinators.
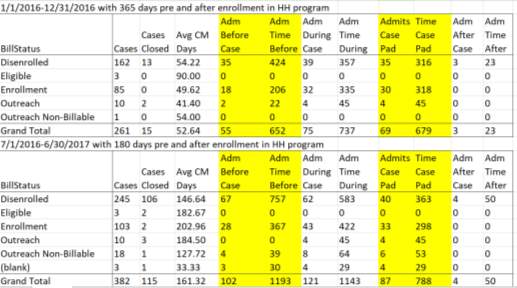
Data on UBA’s Success in Reducing Readmissions
The ultimate goal of care coordination is to reduce readmissions through effective outreach efforts. The UBA program has been extremely successful in managing their mental health and substance abuse patients. Through a concerted effort and communication plan the transition of ED and inpatient admissions improved drastically. The chart below showcases UBA’s success in both 2016 and 2017.
Case Study
In order to demonstrate how members benefit from the health home program, a case study was included to show how the process is handled by the Health Home team.
2017-Summary of UBA Health Home member with a positive outcome due to the involvement of her Accountable Care Manager. Identifying information of member has been changed due to HIPPA regulations.
- Ms. Jane Doe
- DOB 00/00/1960 (56) female
- Diagnosis: Bi-polar
- Providers/community agencies involved in Ms. Doe Case
- UBA Health Home Case Manager
- UBA Health Home Clinical Supervisor
- UBA Health Home Assistant Program Director
- Psychiatrist
- Primary therapist
- APS case worker
- APS supervisor
- APS director
- Guardian Ad Litem
- Legal Aid Hotline: 1-800-649-9125
- 311 City of NY compliant
- Montefiore Medical Director- Glebe Clinic
- Executive Secretary at MMC Glebe Ave clinic
- Bronx Works Assistant Program Director
- SEPS (Special Exit and Prevention Supplement Program)
- NYC Marshall’s office
Ms. Doe is 54y.o. single mom who lives with her adult son in The Bronx. She is over $20,000 in arrears of rent. APS was court ordered to manage her finances as far back as 7/2016. She was evicted on 9/2016, but with the assistance of her psychiatrist strongly suggestive letter detailing Ms. Doe’s mental health status and how it is not safe to evict her, the judge re-instated her back into her home. At this time Ms. Doe was appointed an ad litem guardian to represent her during her housing court proceedings
On 4/17/17, Ms. Doe was notified over the phone by her court appointed ad litem guardian Mr. Smith of the Marshall’s notice of eviction scheduled for 4/19/17. Ms. Doe has not received an actual eviction notice. Ms. Doe is facing eviction despite having APS manage her finances. Mr. Smith has continued to advocate for Ms. Doe throughout court, but with the lack of APS update he could do no more.
Ms. Doe has had her primary therapist Mr. Joseph Brown and her psychiatrist contacted APS, without success. Numbers called were invalid and numerous messages were left unanswered. With the assistance of my direct clinical supervisor and UBA HH Assistant Program Director, it was suggested for me to call Legal Aid hotline 1-800-649-9125 for assistance with member housing emergency. It was also suggested for me to place a complaint to 311 on APS regarding their lack of action on Ms. Doe’s case. I called 311 and a Service request number was provided. It was also advised that my clinical supervisor call and open a new case within APS for negligence of Ms. Doe’s financial matters. My clinical supervisor followed up with APS and obtained a new APS reference. Mr. Smith submitted to the courts the 3rd order to show caused which was denied because there was not enough defensed for her case. The SEPS rent supplement program application which was thought to have been submitted and in process, had not been submitted. When asked who can assist with eviction prevention, Mr. Smith informed of APS Office of Legal Administration who would be able to intercede eviction at court. No confirmation of APS contacting OLA or if it was suggested to Ms. Doe’s APS team in Mr. Smith court summary report to APS.
On 4/18/17, Clinical Supervisor called APS supervisor Ms. Calwell to inquire of eviction prevention. Ms. Calwell called Bronx Works and arranged for Ms. Doe to meet with Mr. Vegas. He will assist Ms. Doe with submitting a SEPs application and will provide a new order to show cause for court submission. Mr. Smith informed me that member will need lease, proof of income and last court stipulation. Ms. Doe does not have any court documentation and I will coordinate with Mr. Smith to have latest court stipulations emailed to Mr. Vegas.
Ms. Doe agreed to apply in person at Bronx Works.
She reports she was able to find the rest of the required documents. However, member was then told she needed to apply and be approved for SEPS (NYC Special Exit and Prevention Supplement Program) before Bronx Works would be able to apply for the One Shot Deal and bring member’s arrear current. Ms. Doe proceeded to encounter multiple barriers with obtaining full submission of SEPS application; such as continuous particular and non-existent documents. Since member resides in a Mitchell-Llama cooperative, she was required to submit a W-9 from the building management as well as a stock certificate for her cooperative apartment.
May/June 2017- ACM was met with resistance from building management for requested documents, was told W-9 are not provided to agencies and stock certificates no longer exist and have not been issued for many years. I was able to obtained documents with similar information as requested by SEPS and submitted to SEPS. Meanwhile Mr. Smith had requested several more Order to Show Cause on behalf of member at court. Member was encountering barriers with transportation to adhere to mental health appointments.
6/12/17- SEPS application was submitted; SEPS requested member’s HRA Public Assistance case status change from “AP” to “SI”. HRA reported member’s Public Assistance case was closed. SEPS requests DRIE (Disability Rent Increase Exemption Program) letter which member is an applicant. 6/16/17- eviction was postponed for 7/11/17 court date. 6/20/17- Mr. Smith was notified by City Marshall of member’s eviction. APS was informed of member’s eviction and the urgency to change member’s Public Assistance case status. APS Ms. Calwell informed member’s status will be changed within the matter of days.
6/21/17- During ACM call with Ms. Doe, she was noted to be intoxicated while babysitting. Mental health providers were notified and Mobile Crisis was sent to her home. Ms. Doe had an overnight stay at a local hospital and discharged home with f/u with her mental health providers. 7/5/17- ACM consulted with UBA management for safety options if eviction occurs. 7/11/17- Mr. Smith was informed by the court that they will no longer be granted member Order to Show Cause. By 7/25/17, an approval for payment will need to be submitted to the court or member will be evicted. Mr. Smith stated he will not be able to intervene anymore.
ACM Inquired if APS will be able to intervene with their legal department, he confirmed that is still a possibility but was not sure if they will do one or if it will be approved.
7/13/17- Ms. Doe public assistance case status was changed for AP, and therefore SEPS was able to proceed with their application. 7/19/17- ACM received approval notice from SEPS. Member was approved for $1,120.61 supplemental monthly renter’s assistance, and $24,561.61rental arrears grant.
Critical Reflection on Theories and Concepts
The departmental practicum experience with University Behavioral Associates has demonstrated that a vast array of resources is needed to make the program successful. Many theories of practice need to be incorporated in order for a program such as UBA, to sustain the high rate of patients entering into health home platforms. UBA has been able to address many of the theoretical applications that are relevant in the field of care coordination.
Analysis Concepts
Return on Investment. This concept is listed first as it plays a pivotal factor when healthcare organizations transition to new service lines. The care coordination program is a costly initiative and must be analyzed carefully.
Market Segmentation Analysis. Market segment analysis allows a healthcare organization to accurately analyze which patient population would best suit the organizations strategy.
Theoretical Concepts
Contingency Theory. Contingency theory is based on the idea that there is not a definitive answer to organizational structure but rather based on the individual company. Contingency theory is crucial to understand as each healthcare organization varies and it is important to customize structure that works for the specific healthcare delivery model.
Organizational Concepts
Organizational Culture. During the practicum experience, the organizational culture was a key success factor for UBA and the healthcare system. Organizational culture refers to the makeup of the team and how the team identifies with the company.
The Hawthorne Effect. The Hawthorne effect outlines the importance that social factors play on team members. The Hawthorne effect enables a company to put systems in place that can lead to positive outcomes in healthcare programs.
Performance Improvement Concepts
SWOT Analysis. A SWOT analysis stands for Strengths, weaknesses, opportunities and threats. An efficient way to plan for a care coordination program is through the use of the analysis and identifying any major gaps in order to mitigate risks.
Lean Six Sigma Methodology. UBA was able to utilize Lean Six Sigma is a methodology to eliminate waste and increase efficiency within the care coordination process.
Changes in Practice and Conclusion
Care coordination has proven to be an effective way to manage high risk patient populations that frequent the emergency rooms leading to potentially avoidable in-patient stays. The mental health and substance abuse population has contributed to a high rate of these types of visits that has been a major problem facing healthcare across the nation. Programs such as UBA’s care coordination platform has been effective in managing these cases leading to positive patient outcomes as well as lowering the cost of healthcare.
There are many more challenges to find solutions for, but streamlining and reducing inpatient readmissions through outreach coordination is the future of healthcare. Organizational culture will be the key factor in determining how successful the programs will be. The team needs to fully buy into the mission, scope and goal of the program as well as have an empathetic skillset to manage the mental health and substance abuse patient populations. If the organization is not fully committed to providing adequate resources such as staffing, training and education, the programs will never be realized to the full potential.
References
- Alakeson, V., Pande, N., & Ludwig, M. (2010). A Plan to Reduce Emergency Room ‘Boarding’
Of Psychiatric Patients. Health Affairs, 29(9), 1637-1642. doi:10.1377/hlthaff.2009.0336
- ASPE. (2016, June 16). Affordable Care Act Expands Mental Health and Substance Use Disorder
Benefits and Federal Parity Protections for 62 Million Americans. Retrieved from
- Baggs, J. G., Schmitt, M. H., Mushlin, A. I., Mitchell, P. H., Eldredge, D. H., Oakes, D., &
Hutson, A. D. (1999). Association between nurse-physician collaboration and patient
outcomes in three intensive care units. Critical Care Medicine, 27(9), 1991-1998.
doi:10.1097/00003246-199909000-00045
- Behr, J. G., & Diaz, R. (2016). Emergency Department Frequent Utilization for Non-Emergent
Presentments: Results from a Regional Urban Trauma Center Study. PLoS ONE, 11(1),
e0147116. http://doi.org/10.1371/journal.pone.0147116
- Bodenmann, P., Velonaki, V.-S., Ruggeri, O., Hugli, O., Burnand, B., Wasserfallen, J.-B., …
Daeppen, J.-B. (2014). Case Management for Frequent Users of the Emergency
Department: Study Protocol of a Randomized Controlled Trial. BMC Health Services
Research, 14, 264. http://doi.org/10.1186/1472-6963-14-264
by improving care for patients needing costly services. NEJM, 361, 1521-1523
- Center for Disease Control. (2016). Health, United States, 2016. Retrieved from National Center
for Health Statistics website: https://www.cdc.gov/nchs/data/hus/hus16.pdf
- Dohan, D., & Schrag, D. (2005). Using Navigators to Improve Care of Underserved Patients.
Cancer, 104(4), 848-855. doi:10.1002/cncr.21214
- Edelman, T. (2016). Reducing Hospital Readmissions by Addressing the Causes || Center for
Medicare Advocacy. Retrieved from http://www.medicareadvocacy.org/reducing-hospital-readmissions-by-addressing-the-causes/
- Feng, J. Y., Toomey, S. L., Zaslavsky, A. M., Nakamura, M. M., & Schuster, M. A. (2017).
Readmission After Pediatric Mental Health Admissions. Pediatrics, 140(6), e20171571.
doi:10.1542/peds.2017-1571
- Gittell, J. H., Fairfield, K. M., Bierbaum, B., Head, W., Jackson, R., Kelly, M., … Zuckerman, J.
(2000). Impact of Relational Coordination on Quality of Care, Postoperative Pain and
Functioning, and Length of Stay. Medical Care, 38(8), 807-819. doi:10.1097/00005650-
200008000-00005.
- Heslin, K., & Weiss, A. (2015). Hospital Re-admissions Involving Psychiatric Disorders. Retrieved
- Institute of Medicine (US) Committee on Crossing the Quality Chasm (2006): Adaptation to
Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental
and Substance-Use Conditions: Quality Chasm Series. Washington (DC): National
Academies Press (US); Coordinating Care for Better Mental, Substance-Use, and General
Health. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19833/.
- LaCalle, E., & Rabin, E. (2010). Frequent Users of Emergency Departments: The Myths, the Data,
and the Policy Implications. Annals of Emergency Medicine, 56(1), 42-48.
doi:10.1016/j.annemergmed.2010.01.032
- Montefiore.org. (2016). Psychiatry and Behavioral Sciences – University Behavioral Associates
New York City – Montefiore Medical Center. Retrieved from
http://www.montefiore.org/psychiatry-services-university-behavioral-associates
- New York State Department of Health. (2016). Health Home Program-Updated Billing Guidance.
Retrieved from
- New York State Department of Health. (2017). Medicaid Health Homes –
Comprehensive Care Management. Retrieved from
https://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/
- Weiss, A., Barrett, M., Heslin, K., & Stocks, C. (2016). Trends in Emergency Department Visits
Involving Mental and Substance Use Disorders. Agency for Healthcare Research and
Quality. Retrieved from
https://www.hcupus.ahrq.gov/reports/statbriefs/sb216MentalSubstance-Use-Disorder-ED-Visit-Trends.pdf
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Mental Health"
Mental Health relates to the emotional and psychological state that an individual is in. Mental Health can have a positive or negative impact on our behaviour, decision-making, and actions, as well as our general health and well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




