Pathophysiology and Common Complications of Obesity
Info: 9017 words (36 pages) Dissertation
Published: 9th Dec 2019
Tagged: PhysiologyNutrition
- Investigated Disease Process
Obesity is the state of having and storing excessive fat in the tissues of the body and having a Body Mass Index of 30 or higher; it is associated with several chronic medical conditions, such as heart disease, high blood pressure, hyperlipidemia, diabetes, and some cancers, all conditions that are prevalent in this writer’s community.
Obesity is a growing concern nationwide. In North Carolina, about 65% of adults are overweight, and 28% are obese. Only 27.5% of adults in North Carolina report an intake of 3 or more servings of fruits and vegetables a day, and 26.4% of NC adults reported no physical activity in over a month. Furthermore, around a third of adults in NC report drinking at least one sugar-sweetened serving of soda per day. (Centers for Disease Control [CDC], 2012)
Thirty-six percent of all adults in Edgecombe County are obese, compared with a statewide rate of 30%. (County Health Rankings and Roadmaps website, 2018) As a result, there are higher-than-average rates of type II diabetes, hypertension, cardiovascular disease, and cancer. (Capps et al., 2013) Limited access to healthy foods and a higher-than-average per capita number of fast food restaurants contribute to the poor health of the population. Derrick Haskins, Health Promotion Coordinator for the Edgecombe County Health Department states, “Edgecombe County is greatly affected by obesity because this is where a perfect storm of risk factors collide”. He calls Edgecombe County an “obesogenic” society and explains that this means that it is easier to be obese than not obese here. (D. Haskins, personal communication, June 20, 2013) Due to the low population density and the fact that many poor residents live in rural areas, access to parks and recreation opportunities is a concern. Easy access to healthy food is lacking for poor consumers. For example, the farmers market in the county seat of Tarboro is rarely open due to the lack of participation and community support. The local grocery stores carry very few organic selections, and the idea that healthy food doesn’t taste good is pervasive. Countyhealthreankings.org rates Edgecombe County 97h out of 100 counties in North Carolina in overall health, and in the category called “Health Behaviors”, they rank Edgecombe County as 95th. (County Health Rankings and Roadmaps website, 2018)
A1. Pathophysiology
Obesity may be the most talked-about disease process in the history of healthcare, and explanations of its pathophysiology range from the very simple to the very complex. Simply, the layperson may understand obesity as a condition in which excess energy (calories) consumed is converted to fat and stored in the cells of the body for later use. The scientific and medical communities know that there are many more factors at play in addition to the matters of fat storage and energy metabolism, and that obesity is a central cause of disease conditions such as type II diabetes, hyperlipidemia, atherosclerosis, and hypertension. Nearly two-thirds of the American population is overweight or obese, so it is no wonder that the incidence of these chronic illnesses has increased over the last century as well…so much so, that many experts now consider obesity an epidemic.
There are many causes of the obesity epidemic, and if you ask several different experts, you may get several different opinions on what they are. Environment surely plays a part; over the past century, industrial farming practices have largely wiped out hunger and famine from American society. At the same time, the age of technology has made people more sedentary. Many people no longer must do hard physical labor to make a living, and our leisure time is often spent in front of a television or computer. There has also been an increase in the use of medications that disrupt metabolism and cause weight gain. There are also genetic factors to consider; the New England Journal of Medicine discusses eleven monogenic forms of obesity. (Heymsfield & Wadden, 2017) An example of one of these genetic forms of obesity includes a deficiency of melanocortin-r and leptin receptors, which affects neural circuits that regulate energy homeostasis.
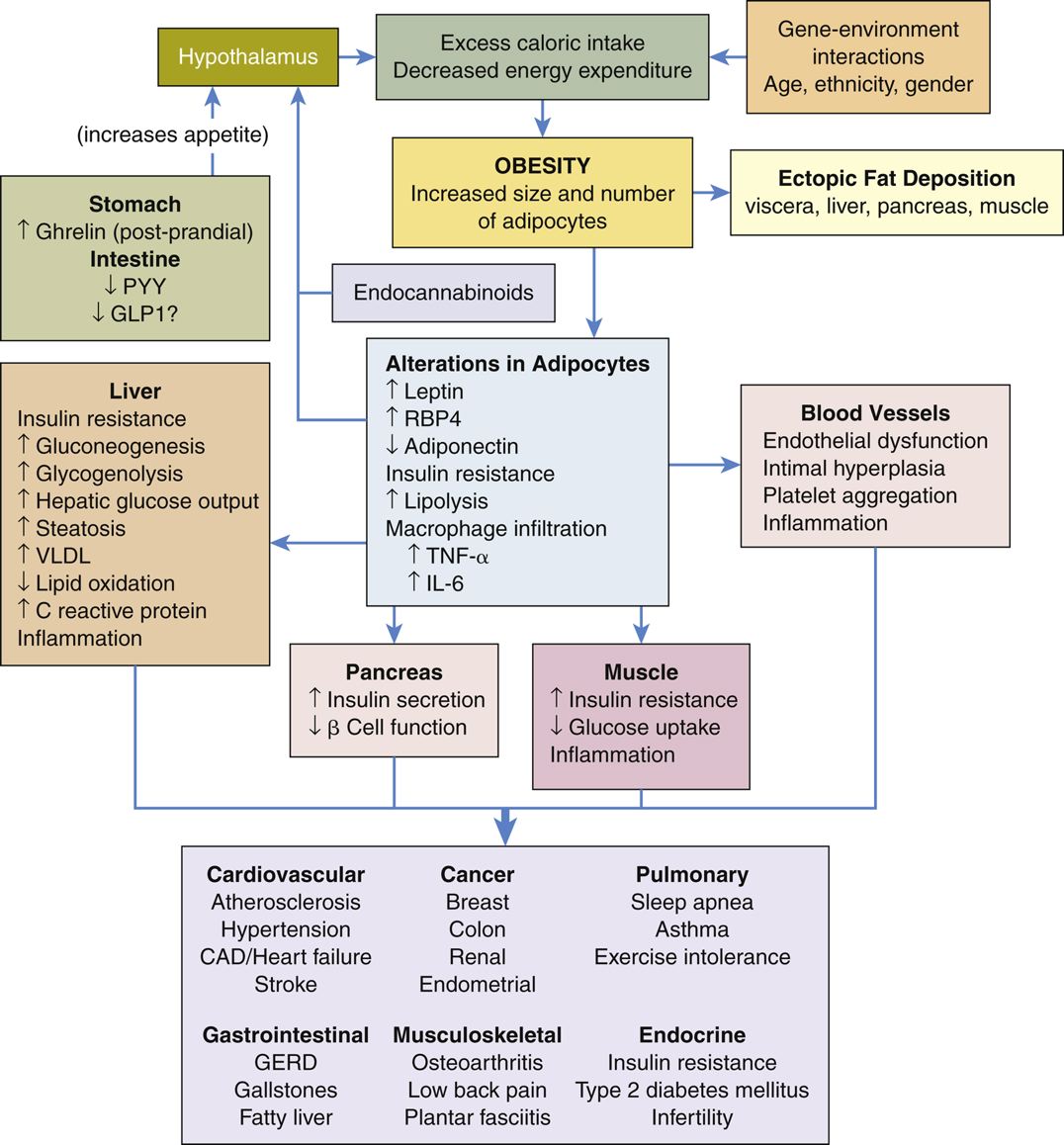
Whether due to environmental, genetic, or other factors, obesity is caused when there is a dysregulation of energy expenditures vs. food intake. The hypothalamus contains neuropeptide hormones that control energy balance by regulating energy expenditure, and cells within adipose tissue (fat), the stomach, pancreas, and other organs also contain mechanisms which affect energy metabolism. The brain also plays a part, providing sensory input (taste and smell) and cognitive processes (such as cravings and disordered eating) that affect energy intake and expenditure. Substances called cytokines are secreted from adipocytes; these cytokines promote systemic and local states of inflammation and have been implicated in the pathogenesis of type 2 diabetes, cardiovascular disease, certain cancers, osteoarthritis, asthma, sleep apnea, and nonalcoholic fatty liver disease.
When food intake is reduced, or physical activity is increased, a negative energy balance occurs. This causes a chain of adaptive events as the body tries to preserve vital functions, including the storage of excess energy as glycogen and fat for later use. These events use different psychological and metabolic processes to reduce resting energy expenditures and conserve calories. When this occurs, there is sometimes a rebound increase in appetite, which leads to a high relapse rate in obese people who have lost a bit of weight. This explains why diets rarely succeed in the long run. Although the reasons and causes remain unclear, it is highly hypothesized that people who are no longer obese are not metabolically or physiologically the same as people who were never obese, as they have a high likelihood of gaining the weight back. This supports the concept of obesity as a chronic disease that requires vigilant monitoring and management.
Excess body fat generally develops over an extended period time when there is a chronic positive energy balance. The body stores excess energy as fat for later use, even if the calories are from carbohydrates (this is called lipogenesis and is made possible by the conversion of acetyl-CoA into fatty acids in the liver). Excess lipids, including triglycerides, are deposited in the adipose tissue of the body, and other tissues also become enlarged, such as the liver, skeletal muscle, and other internal organs. Thus, an obese person not only has more body fat than a non-obese person, but also more lean mass and a higher resting metabolic rate. The obese person also has a higher cardiac output and blood pressure.
Most fat cells in subcutaneous adipose tissue are white due to containing triglycerides and cholesterol ester. These white fat cells secrete hormones such as leptin and adiponectin, which regulate hunger. Brown adipocytes are deposited in visceral adipose tissue, and this tissue is significant in an obese person. This visceral adiposity is linked to many of the metabolic and mechanical health concerns that accompany obesity. For example, fat surrounding the kidney compress them and cause hypertension. Excess pharyngeal soft tissue may block the airway during sleep and is associated with sleep apnea. Excess body weight puts extra strain on joints and is a risk factor for osteoarthritis. Excessive visceral fat can cause increased pressure within the abdomen and cause reflux disease. Excessive adipose tissue causes excessive secretion of proinflammatory adipokines, which leads to a chronic low-grade systemic inflammation in many obese people. The hydrolysis that occurs in fat cells releases free fatty acids, which is transported to sites around the body in the bloodstream. Elevated levels of these free fatty acids found in obese people contribute to insulin resistance.
Even moderate weight loss, which is defined as a 5-10% reduction in weight, has been proven to cause significant improvements in some chronic disorders and related risk factors. A 5% weight loss causes an improved insulin response by improving pancreatic beta-cell function, for example. In one study, patients lost an average of 8.6% of their body weights, and were observed to have improvements in blood pressure, triglyceride levels, and hemoglobin A1C. The responses to weight loss were graded; those with greater weight loss experience greater health improvements. (Heymsfield & Wadden, 2017)
Pathophysiology and Common Complications of Obesity
A2. Standard of Practice
The state of North Carolina has several initiatives in place to address the health crisis that is obesity. Eat Smart Move More NC is a state initiative that promotes healthy eating and exercise opportunities in workplaces, churches, schools, and communities in the state. This includes the church-specific initiative of Faithful Families Eating Smart and Moving More, community grants, worksite wellness initiatives, and a healthy environment initiative. There is also the North Carolina Sustainable Local Food Advisory Council, which works to build local food economies that provide citizens with access to fresh and nutritious foods. The 21st Century Farmers’ Markets Program aims to increase food stamp usage at local farmers markets, thus giving low-income families better access to fresh food. (CDC, 2012) A local non-profit organization, The Down East Partnership for Children has several initiatives in place to improve nutrition in schools, educate children on healthy diets, and provide exercise opportunities for local children.
Medical management of obesity consists of three areas; behavioral modification, pharmacological therapy, and bariatric surgery. Most primary care providers in the author’s community follow the clinical guidelines of the American Heart Association, American College of Cardiology, and The Obesity Society when addressing and treating obesity in their patients. These clinical guidelines are summarized below:
- Identify patients who need to lose weight by measuring body mass index (BMI) and waist circumference. Advise patients that the greater the BMI or waist circumference, the higher the risk of developing cardiovascular disease and diabetes.
- Counsel overweight and obese adults that even a modest weight loss of 5% may decrease their mortality risk and improve their health.
- Prescribe a weight reduction diet as part of comprehensive lifestyle change, using one of these suggestions as a guide: 1200-1500 kcal/day for women and 1500-1800 kcal/day for men, 500-750 kcal/day energy deficit, or use one of the evidence-based diets that restrict certain food types (such as low-carb or low-fat) to create an energy deficit and foster weight loss. Consider referring to a clinical nutritionist for education and coaching.
- Prescribe lifestyle intervention and counseling. Refer patients to a comprehensive lifestyle program to assist patients with adhering to diet and exercise. These programs can be offered online or in-person, individually or in groups.
- Recommend bariatric surgery for select obese patients. Weigh the benefits and risks, considering operative risks, obesity-related comorbidities, age, BMI, psychosocial and behavioral factors, and risk of long-term complications from obesity vs. surgery.
(National Guideline Clearinghouse [NGC], 2014)
A2a. Pharmacological Treatments
While the AHA et al. doesn’t include pharmacological therapies in their recommendations for the treatment of obesity, several new medications have been approved by the FDA for this purpose in the past five years. The North Carolina Medical Board position statement on the treatment of obesity states “It is the position of the North Carolina Medical Board that the cornerstones of the treatment of obesity are diet (caloric control) and exercise. Medications and surgery should only be used to treat obesity when the benefits outweigh the risks of the chosen modality.” (North Carolina Medical Board website, 2017)
One drug, Orlistat/Xenical, was approved in 1999 and is still on the market, but other drugs that have been used for obesity in the past have been removed from the market due to severe side effects and risks. Orlistat works by inhibiting the absorption of fat from the GI tract, thereby decreasing the number of calories absorbed by fatty foods. This reduction in caloric absorption causes weight loss, which may limit comorbidities related to obesity. Side effects include severe gastrointestinal upset if too much fat is ingested. A low dose of Orlistat called Alli is available over-the-counter in the United States. Because Orlistat blocks fat absorption, people who take it may become deficient in fat-soluble nutrients such as Vitamins D, E, and beta carotene, but these deficiencies are easily treated with vitamins and supplements. Orlistat is currently not widely prescribed in North Carolina, but Alli is available over-the-counter.
In 2012, the FDA approved a combination of phentermine and topiramate, called Qsymia, for the long-term treatment of obesity. Phentermine works to suppress appetite and was a part of the controversial drug Fen-Phen (Fenfluramine/phentermine) that was widely prescribed in the ‘90s. In 1997, Fenfluramine was found to cause dangerous and sometimes fatal pulmonary hypertension in some patients and was withdrawn from the market. Phentermine is combined with topiramate, which is an FDA-approved medicine for epilepsy. Topiramate has been shown to cause taste aversion and therefore causes reduced appetite and caloric intake. Decreased appetite and taste aversion can assist with compliance with a reduced-calorie diet.
In 2012 the FDA approved Lorcaserin (Belviq) as a long-term treatment for adult obesity. It is a selective serotonin receptor agonist that reduces appetite by binding to receptors on neurons in the hypothalamus. Decreased appetite helps patients to comply with a reduced-calorie diet. Because of its class, caution must be taken with patients who are on selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, or Saint John’s Wort, as to prevent serotonin syndrome from occurring.
Bupropion/Naltrexone (Contrave) is a combination of a popular antidepressant (brand name Wellbutrin) and an opioid receptor antagonist (brand name Narcan). This drug was FDA-approved in 2014. Bupropion has been shown to cause weight loss as opposed to other antidepressants, many of which are known to cause weight gain. Bupropion inhibits the reuptake of dopamine and norepinephrine, which promotes activation of the central melanocortin pathways. Naltrexone diminishes the auto-inhibitory feedback loop on neurons activated by bupropion, and this allows for sustained weight loss. Contrave reduces hunger and helps to control cravings, which helps patients to comply with a reduced-calorie diet. This drug must be prescribed with caution to patients who are on MAO inhibitors, antidepressants, or opioid or opioid agonists.
Liraglutide 3.0 (Saxenda) was FDA-approved in 2014 and is a GLP-1 receptor agonist. In doses up to 1.8 mg, it has been used to treat type 2 diabetes under the brand name Victoza. As Saxenda, patients take 3 mg per day. Effects include delayed gastric emptying and suppressed appetite, which helps patients to comply with a reduced-calorie diet. This medication is contraindicated in patients with a personal or family history of thyroid cancer, since animal studies indicate it may be associated with that condition. (Kumar & Arrone, 2017)
In the author’s state, physicians are prohibited from prescribing non-FDA-approved medications for weight loss such as HCG by the North Carolina Medical Board. (North Carolina Medical Board website, 2017) Furthermore, they prohibit using FDA-approved medications like those listed above for controlling weight in people who are not obese. As previously stated, the North Carolina Medical Board advises that pharmacological treatments for obesity should not be prescribed until diet and exercise efforts have been exhausted, and the benefits of the drugs outweigh the risks. The list of drugs that are FDA-approved for weight loss are limited, and one weight loss center lists Saxenda, Belviq, Contrave, and Qsymia among the medications that they may prescribe for their patients. (Essential Weight Loss website, 2018) Blue Cross Blue Shield of North Carolina, the largest insurer in the state, only has utilization management criteria in place for Belviq, Contrave, and Qsymia, and plan members only qualify to have these drugs covered by the plan if they have a BMI of >30, or >27 in the presence of at least one weight-related comorbid condition. (Blue Cross Blue Shield of North Carolina [BCBSNC], 2016) These three drugs have been shown to affect the management of obesity in the following ways:
- In randomized controlled studies, Qsymia has been shown to cause a 7.5% decrease in body weight over 2 years when compared to placebos.
- In randomized controlled studies, patients taking Belviq had >5% weight loss over a year and patients who continued Belviq beyond one year had greater success at keeping the weight off than patients in placebo groups.
- Four double-blind controlled trials show that Contrave, along w/ lifestyle change, caused a 6.1% loss of body weight in study participants.
- Though not covered by the largest insurer in the state, randomized controlled study participants lost an average of 6.2% body weight over a year on 3 mg daily of Saxenda. (Kumar & Arrone, 2017)
As little as a 5% reduction in weight has been shown to reduce the risk of comorbidities, so these effects on obesity in the state are significant.
A2b. Clinical Guidelines
The clinical guidelines for assessment, diagnosis, and treatment of obesity, as set forth by the American Heart Association, American College of Cardiology, and The Obesity Society, are summarized below:
- Identify patients who need to lose weight by measuring body mass index (BMI) and waist circumference. Advise patients that the greater the BMI or waist circumference, the higher the risk of developing cardiovascular disease and diabetes.
- Counsel overweight and obese adults that even a modest weight loss of 5% may decrease their mortality risk and improve their health.
- Prescribe a weight reduction diet as part of comprehensive lifestyle change, using one of these suggestions as a guide: 1200-1500 kcal/day for women and 1500-1800 kcal/day for men, 500-750 kcal/day energy deficit, or use one of the evidence-based diets that restrict certain food types (such as low-carb or low-fat) to create an energy deficit and foster weight loss. Consider referring to a clinical nutritionist for education and coaching.
- Prescribe lifestyle intervention and counseling. Refer patients to a comprehensive lifestyle program to assist patients with adhering to diet and exercise. These programs can be offered online or in-person, individually or in groups.
- Recommend bariatric surgery for select obese patients. Weigh the benefits and risks, considering operative risks, obesity-related comorbidities, age, BMI, psychosocial and behavioral factors, and risk of long-term complications from obesity vs. surgery.
(National Guideline Clearinghouse [NGC], 2014)
In addition to the above recommendations, the Endocrine Society (an international organization) recommends FDA-approved weight loss medication to enhance compliance to diet and exercise programs in obese individuals. (Apovian et al., 2015)
A2c. Standard Practice of Disease Management
North Carolina has a plan to address the obesity epidemic called Eat Smart Move More NC. It’s vision statement says, “All North Carolinians should have the opportunity to make healthy choices for eating and physical activity that lead to healthy weight.” (“North Carolina’s Plan to Address Obesity,” 2013, p. 2) Eat Smart Move More NC lists core behaviors that it believes are essential to improving the rate of obesity in the state:
- Increase physical activity
- Increase consumption of fruits and vegetables
- Decrease consumption of sugar-sweetened beverages
- Reduce consumption of energy-dense foods
- Decrease screen time (television, computer, smart phone etc.)
- Increase breastfeeding initiation, duration, and exclusivity
In Edgecombe County, 66% of adults are overweight or obese, compared to the statewide rate of 63%. Per clinical guidelines, medical management of obesity consists of three areas; behavioral modification, pharmacological therapy, and bariatric surgery. Most primary care providers in the author’s community follow the clinical guidelines of the American Heart Association, American College of Cardiology, and The Obesity Society when addressing and treating obesity in their patients, but there are also local community organizations that are striving to follow the objectives of Eat Smart Move More NC by improving the core behaviors listed above.
- The Edgecombe County-based Down East Partnership for Children has the Healthy Kids Collaborative initiative in place to improve nutrition in schools, educate children on healthy diets, and provide exercise opportunities for local children. (The Down East Partnership for Children website, 2018)
- The Edgecombe County Health Department has a chronic disease self-management program that aims to improve self-management skills of obesity-related conditions such as diabetes, chronic hypertension, and heart disease. The program provides education on nutrition and healthy eating and is aligned with Eat Smart Move More Weigh Less principles. (“2014 Edgecombe State of the County Health Report,” 2015)
- The Edgecombe County Health Department is also in planning the planning stages for a Healthy Youth Initiative project, and work with the local hospital and Nash County agencies to organize the Twin Counties Heart Walk in 2014.
- A grant from the Centers for Disease Control (CDC) has allowed for the placement of a Program Associate in the county Cooperative Extension office to coordinate and deliver Health Matters programming to specifically address the issues of overweight and obesity in Edgecombe County. (2018 Edgecombe County plan of work, 2018)
- The local hospital uses nursing admission assessment templates in Epic for inpatient, outpatient, and emergency patients that routinely screen for obesity by assessing the patient’s height and weight and calculates BMI. If BMI is over 30, the care plan templates automatically prompt nurses to include weight management interventions such as diet education in the patient’s care plan. (E. Glover, personal communication, July 2, 2018)
Despite these local initiatives, the obesity rate remains one of the highest in the state. Local providers are hindered in following standard practice for managing obesity in their patients by:
- High rate of patients on Medicaid, which does not cover pharmaceutical treatments for obesity, bariatric surgery, health coaching, or exercise classes due to low budgets.
- High rate of people living in poverty, which necessitates the need for people to buy “cheap” food, and poor access to fresh and organic fruits and vegetables for much of the year.
- A culture of “home cooking” among the county’s long-time residents, which includes using excessive amounts of salt and fat in cooking.
- Low budgets of the public school system, which limits programs to provide healthy meals for the county’s children at school or educate them on good nutrition.
- Few free or inexpensive opportunities for organized physical activity and recreation in the county. Exercise and outdoor recreation is simply not a part of the local culture.
A3. Managed Disease Process
The long-term effects of obesity develop gradually over time and may differ from one person to another. Patients with obesity present with varying levels of wellness and disease. One person may visit her doctor asking for help losing weight, although she has a normal blood pressure and A1C. Another patient may not seek treatment for obesity until after he has had a heart attack. The goal of obesity treatment is to get to a healthy weight and stay there. Lifestyle changes are the safest ways to treat obesity, as surgery and pharmacological interventions carry a lot more risk and generally don’t address the behavioral aspects of the disease.
Dietary changes and exercise are the most effective ways to lose weight, and unfortunately a person is largely on their own when it comes to making the needed changes, since providers, educators, dieticians, and coaches are not with a person when they are making their day-to-day decisions. Providers should assess readiness to change before prescribing a lifestyle management program; lifestyle change requires an emotional commitment since not only does the person need to lose the weight, they also need to maintain their weight loss. Maintenance has shown to be the most difficult part of beating obesity. Clinicians should provide resources such as education, coaching, dietician intervention, and access to support groups for people who are ready to change their lifestyles and lose weight. Readiness to change may be the single most influential factor for a provider to consider when prescribing weight reduction interventions, as it greatly influences treatment adherence and effectiveness.
Most people know that a healthy diet and regular physical activity are essential steps that a person should take to protect themselves from chronic disease, but knowledge alone is not enough to protect a person from the effects of obesity. Before surgical or pharmaceutical intervention is warranted, a patient must first exhaust all efforts to change their diet and activity level and develop healthy habits; in fact, most insurance plans will not cover surgery or pharmaceutical weight loss aids without a provider first showing that all other efforts to lose weight have failed.
Since obesity causes serious chronic illness, life expectancy and health outcomes certainly improve when a person successfully manages their obesity by losing a modest amount of weight. A meta-analysis performed by researchers from the National Institutes of Health (NIH), found that obese adults have a lower life expectancy of up to 14 years due to the risks of diabetes, stroke, cancers, heart disease, and liver disease. (“NIH study finds extreme obesity may shorten life expectancy,” 2014) Individuals who successfully manage their obesity by losing weight may decrease their chances of chronic illness, therefore increasing life expectancy significantly. A weight loss of even 5% can improve metabolic function in obese patients. One study showed that participants who lost 5% of their body weight had not only decreased visceral body fat, but also decreased levels of glucose, insulin, leptin, and triglycerides in the plasma. Metabolically, this translated to an improved response to insulin and a decreased risk of complications from diabetes and heart disease. (“Benefits of moderate weight loss,” 2016)
A3a. Disparities
Due to the rising cost of healthy food, transportation issues, and poor access to health care, it would make sense that obesity-related health problems would be more prevalent among the most poverty-stricken segment of the population. The low-income residents of Edgecombe County of all ages have a greater incidence of obesity than the higher-earning population. There is a high level of stress among this population related to family problems, financial woes, and health issues. Countyhealthrankings.org states that 32% of the population in Edgecombe County has poor social support. There is limited access to stress reduction techniques such as yoga classes, meditation classes, support groups, and exercise clubs. Therefore, people often resort to excessive eating and drinking to relieve stress.
Many of the low-income residents of Edgecombe County live in its extensive rural areas and have inadequate transportation to healthy food and recreation opportunities. Most of Edgecombe County is considered a “food desert”.
Forty percent of children in Edgecombe County live in poverty, in comparison to 25% statewide. Twenty-nine percent of children in Edgecombe County are overweight or obese before kindergarten (compared to 16% statewide in North Carolina), and the problem is growing. (Robert Wood Johnson Foundation [RWJF], 2013) Rural areas across the country share the same disparities as Edgecombe County due to lack of financial and educational resource. A 2012 study published in the Journal of Rural Health found that 40% of adults in rural areas nationwide were obese, compared with 33% of adults in rural areas. (Befort, 2012)
A person who is successfully managing their obesity, in theory, will not remain obese. It makes sense that a person with adequate financial resources will be more successful at losing weight, for all the reasons listed above, and because they may have access to coaches, dieticians, over-the-counter supplements, and a general lack of financial stress than a person who is a recipient of state-funded healthcare such as Medicaid.
To demonstrate these points, consider this comparison; Wake County, which is only 60 miles west of Edgecombe County, is the wealthiest county in North Carolina with a median household income of $66,579, compared to $33,892 for Edgecombe. (USA.com website, 2018) The obesity rate for adults in Wake County is 23%, compared to 36% in Edgecombe. The disparity is clear; adults in Wake County overall have higher incomes which provide better access to good health insurance coverage, healthy food, physical activity opportunities, social support, and behavioral resources. These differences allow for better public health and lower obesity rates.
Obesity is not an epidemic that is confined to the United States, and the United States is not the most obese nation on Earth; in fact, it is number four on the list. The small island of Nauru in the Pacific has the distinction of being the most obese nation on earth, with 97% of its population being overweight and 72% being obese. Incidentally, it also has the highest rate of type II diabetes in the world. Nauru experienced an economic boon in the 1970’s and 80’s, and most residents no longer had to work. At this time, Western foods began to be imported onto the island, replacing the standard diet of fresh-caught fish and fruit. (Nishiyama, 2012) The other two top-three obese nations, the Cook Islands and Tonga, are also South Pacific islands, and have high obesity rates for very similar reasons: remote access to health care, sedentary lifestyles, and imported food. Pacific islanders are genetically predisposed to having larger builds, and when exposed to Western foods and no exercise, it is no wonder that obesity runs rampant in this area of the world.
In comparison, Japan has one of the lowest obesity rates in the world, despite being an industrialized nation. The obesity rate in Japan is just under 4%. Many factors may contribute to this disparity; the Japanese diet is high in vegetables, fish and rice, and chopsticks make it harder to eat too quickly, allowing a person to become full on less food. Food prices are also higher in Japan, which further deters over-eating. The Japanese generally walk more than citizens in other countries because the cost of owning a vehicle is much more than the cost of public transportation, and public transportation in Japan is convenient and efficient. The Japanese island of Okinawa, which is like Nauru in that it is an isolated island, has long been thought to have the healthiest people on earth due to fresh air, healthy diet of mostly fish and vegetables, and lack of access to Western food and modern conveniences. (Senauer, 2006)
A4. Managed Disease Factors
Several factors may influence how successful a patient is with managing obesity.
- Financial resources – A patient who has the financial resources to buy healthy, organic food, including fresh fruits and vegetables, will certainly have better success in managing their weight and preventing chronic disease. Financial resources may also afford a patient access to health coaches, dieticians, nutritional supplements, and memberships to fitness clubs, all of which are excellent tools to help a person manage or lose weight.
- Excellent health insurance coverage – Commercial or employer-sponsored insurance plans sometimes offer free access to health coaches and dieticians (in fact, this author is a disease management nurse for a large health insurance company and spends a large percentage of working hours coaching plan members on losing weight and improving diet and exercise). A good health insurance plan may also cover expenses such as dietician visits, health club memberships, or pharmacological or surgical interventions for weight loss when the benefits of said interventions are shown to outweigh the risks.
- Access to Care – Some patients will have better access to more provider options and resources just by living in an urban area with a lot of services offered. Reliable transportation also plays a role in ensuring good access to healthcare services that are useful in managing obesity.
- Readiness to change – As mentioned previously, this may be the single most important factor in influencing a patient’s adherence to a weight loss plan and is more likely to ensure that their lifestyle changes become new habits which will allow them to maintain weight loss. While attending a health coaching program at Duke Integrative Medicine, this author learned the stages of change; precontemplation, contemplation, preparation, action, and maintenance. A person in precontemplation is unlikely to make lasting change, as they are likely unwilling, unaware, or uninterested in doing so. At the other end of the continuum, a person at the maintenance stage has been successful at making the change and is in the process of maintaining the new behaviors. Most people will cycle back and forth through the stages until finally (hopefully) settling in the maintenance stage permanently.
A4a. Unmanaged Disease Factors
The absence of the above-mentioned factors may lead to unmanaged obesity, which could cause a cascade of physiological changes that end in chronic conditions such as diabetes, hypertension, cardiovascular disease, stroke, and even cancer.
- A lack of financial resources may prevent a person from buying high-quality, healthy fresh food, attending support groups, fitness clubs, or even from getting nutritional or emotional counseling which would help them to lose weight.
- A person without good health insurance coverage may not be able to access coaches and dieticians, health educators, or pharmaceutical or surgical interventions, as Medicare and Medicaid generally don’t cover these things. Even worse, a person with no health coverage at all may have little to no way to pay for the long-term effects of obesity.
- A patient with poor access to care, whether it be because they live in a rural area with a shortage of providers and resources, or because they don’t have reliable transportation, will have a more difficult time managing their obesity and losing weight. These people may also have trouble getting to a place where they can buy quality food or may live in a “food desert”.
- Finally, a person who is not ready to make lasting lifestyle changes is not going to be successful at managing their obesity. A person in precontemplation is unlikely to make lasting change, as they are likely unwilling, unaware, or uninterested in doing so. Even patients who are in contemplation or preparation may have much difficulty managing their obesity if they also lack one of the other factors listed above.
An obese person is likely to appear large for their frame, and will, by definition, have a body-mass index of over 30%. Even after weight loss, a previously-obese person may have sagging skin and breasts which cause lasting problems. Long-term obesity may cause other physical effects such as arthritis and chronic pain, diabetes, hypertension, sleep apnea, and skin disturbances. Obesity carries emotional costs as well; obese people are at an increased risk of anxiety and depression, low self-esteem, and self-consciousness.
- Patients, Families, and Populations
Obesity is prevalent in today’s modern society, and it is affecting the way people live, work, socialize and play. Because obesity may cause physical effects such as arthritis and chronic pain, diabetes, hypertension, sleep apnea, and skin disturbances, an obese person may miss more work days due to sickness or disability from obesity-related complications. An obese person is more likely to have chronic pain and poor cardiovascular endurance, which may impact the types of work he is able to do. Thus, the effects of obesity on a person’s work can have long term financial implications. Clearly, for the same reasons that it impacts work, obesity can cause a person to miss out on many opportunities for play and leisure due to physical limitations and illness. An obese person may opt to stay home rather than participate in activities and events, which will also negatively impact their social life. Poor health, financial hardship, and social isolation may therefore also cause relationships to be strained. Obese people are at an increased risk of anxiety and depression, low self-esteem, and self-consciousness, which may further impact their relationships and social life.
Since the obesity rate in this writer’s community is nearly 40%, obesity is a major problem that impacts the financial and emotional status of most of its residents, whether directly or indirectly. Obese parents are likely to pass their poor health habits down to their children, so the problem perpetuates itself despite many community efforts to improve the health of residents. A local non-profit organization, The Down East Partnership for Children has several initiatives in place to improve nutrition in schools, educate children on healthy diets, and provide exercise opportunities for local children; nevertheless, childhood obesity in this community continues to be on the rise.
B1. Costs
Obesity has been associated with increasing incidence of health conditions such as diabetes, high blood pressure, cardiovascular disease, cancer, arthritis, and depression, which causes it to be the biggest driver of preventable healthcare spending in the United States. These financial costs affect obese individuals and their families, as well as all American taxpayers, since nearly one in five, or over 70 million Americans are covered by Medicaid. (Medicaid.gov, 2018) Estimates for obesity-related healthcare spending range from $147 billion to over $200 billion per year. (The State of Obesity, 2018) In addition to higher healthcare utilization, obese people are increasingly being required to pay higher health insurance premiums. As stated above, obesity is also associated with increased job absenteeism and lower job productivity, which cause further financial implications for obese people.
Locally, the financial impact of obesity is astronomical. In 2007, over $4.7 million of Medicaid expenditures alone were spent on overweight and obesity-related health problems. (Eat Smart Move More NC, 2007) This places a tremendous strain on the taxpayers of Edgecombe County, as municipal budgets are already strained.
- Best Practices Promotion
This author’s current organization is a large for-profit health insurance company which insures over 7 million people in 14 states. The organization has a robust care management/coaching program for it’s plan members, and claims data is used to identify members who have chronic illnesses or are at-risk for ongoing health issues. Care managers collect health information from members and perform education, but much of what they do with members is personalized goal-setting and lifestyle management.
Best practices for the management of obesity are largely focused on promoting healthy eating and physical activity. Initiatives that target education, utilization of available resources, and support for lasting lifestyle change would do much to encourage and support members to manage and reverse their obesity, which would improve and prevent obesity-related complications from diabetes, cardiovascular illness, cancer, and musculoskeletal injuries.
C1. Implementation Plan
The following initiatives could help the organization to promote best practices in obesity management.
- Targeted health coaching and motivational interviewing training for nurse care managers. Most of the nurse care managers that the organization hires are seasoned nurses with acute care, home health, and long-term care experience. Having such an experienced nursing staff ensures that the care management program can serve members with a wide range of disease states. However, nurses are generally trained to be educators and not health coaches. Lifestyle change requires meaningful goal-setting, client empowerment, and barrier identification; people don’t change just because someone tells them to do so. A coach differs from an educator in that a coach uses techniques to lead a person to identify what is important to them, and helps them to set meaningful and attainable goals and to take steps to reach those goals using SMART interventions (Specific, measurable, attainable, realistic, and timely). The American Holistic Nurses Association (AHNA) (http://ahna.org) offers a nurse coach certification that has established minimum competency standards for coaching practice by nurses. The organization’s initiative should require AHNA-approved courses to be administered to all nurse care managers and nurse coaches who will be assisting members with lifestyle change and chronic disease management and should offer incentives for nurses who want to pursue the AHNA certification.
- Offer incentives for members to encourage them to consume more fruits and vegetables, engage in more physical activity, and actively participate in lifestyle management/care management programs. The initiative would include vouchers for farmers markets, paid gym memberships, reduced copays and premiums for insurance products, and a rewards program in which a member would earn points for attending personal training sessions and participating in the organization’s lifestyle management program. These points would be redeemable for gift cards to various retailers.
- Offer incentives for providers for performing obesity screening and interventions to treat obesity, particularly for family medicine practitioners who see patients across their entire lifespans. These interventions would include counseling on diet and exercise, short-term use of medications, referrals to dietitians or behavioral therapy, and in some cases, referrals for weight loss surgery. Providers should also be rewarded for being local advocates for healthy lifestyles. Incentives for these providers can be streamlined claims processing for obesity-related interventions, public recognition (such as rewarding them with a healthy-lifestyles designation), and financial incentives for achieving improved outcomes in obese patients. When health plans and providers work together to influence lifestyle choices of the people they serve, lasting change can be achieved.
C2. Evaluation Method
To measure the success of the initiatives mentioned above, the organization will continue to use claims-based data and reporting, as it currently has success with using this data to identify members with certain health risks, high utilization of healthcare money, and potential risk for hospital admissions.
- To measure the success of the health coaching training for nurse care managers, data will be captured from the Healthy Returns Systems (HRS), which is the documentation system for care management. This data will include member weight and BMI, successfully completed care plan goals, and active engagement of member in goal-setting and follow-up calls. Each obese member that is engaged in the care management program will be automatically added to a report based on BMI, and monthly reports and graphs will be generated for each care manager’s members to show their success in coaching their members towards positive health outcomes and weight loss. Another measurement of this intervention will be a report showing how many nurses are certified in nurse coaching after the end of the first year of the initiative.
- Data will be captured to show whether vouchers for farmers market produce or gym memberships have been redeemed. Data will also be collected to show the utilization of the personal trainer incentive, and HRS data will be collected to show how the offering of these incentives affects member participation in the care management program over time. If there is a general upward trend in membership over the course of a year that can be visualized on a graph, the member incentives will be considered to be a successful initiative.
- Claims data will be analyzed to show how many providers are screening for obesity and actively treating it with the interventions mentioned above. This data will be compiled into monthly reports, and a graph for the first year of the initiative should trend upwards to demonstrate success of the initiative. Improved patient outcomes of the providers who are taking advantage of these incentives will also be demonstrated by a reduction in utilization of healthcare dollars towards obesity-related illnesses.
References
2014 Edgecombe County State of the County Health Report. (2015). Retrieved from http://www.edgecombecountync.gov/Departments/Health%20Department/Environmental%20Health/2014%20sotch%20report%20edgecombe%20county%20final.pdf
2018 Edgecombe County plan of work. (2018). Retrieved from https://newton.ces.ncsu.edu/copow_cws/print.php?county_id=33
Apovian, C., Aronne, L., Bessesen, D., McDonnell, M., Murad, M. H., Pagatto, U., … Still, C. (2015, February 2015). Pharmacological management of obesity: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology and Metabolism, 100(2), 342-362. https://doi.org/10.1210/jc.2014-3415
Befort, C. (2012, May 31, 2012). Prevalence of Obesity Among Adults from Rural and Urban Areas of the United States: Findings from NHANES (2005‐2008). The Journal of Rural Health, 28, 392-397. https://doi.org/10.1111/j.1748-0361.2012.00411.x
Benefits of moderate weight loss in people with obesity. (2016). Retrieved from https://www.nih.gov/news-events/nih-research-matters/benefits-moderate-weight-loss-people-obesity
Blue Cross Blue Shield of North Carolina. (2016). Bupropion/Naltrexone (Contrave®1) Lorcaserin (Belviq®1, Belviq XR®1) Phentermine/Topiramate ER (Qsymia®1) utilization management criteria. Retrieved from https://www.bluecrossnc.com/sites/default/files/document/attachment/services/public/pdfs/formulary/weightloss_criteria_um.pdf
Capps, M., Cherry, M., Lancaster, M., Love, Z., Raines, J., Waggy, M., & Vitiello, K. (Eds.). (2013). Edgecombe county community health assessment. Retrieved from Edgecombe County, North Carolina website: http://www.edgecombecountync.gov/Departments/Health%20Department/Environmental%20Health/edgecombe%20county%20cha%20final%20report%20(3).pdf
Centers for Disease Control. (2012). North Carolina State Nutrition, Physical Activity, and Obesity Profile. Retrieved from http://www.cdc.gov/obesity/stateprograms/fundedstates/pdf/north-carolina-state-profile.pdf
County Health Rankings and Roadmaps website. (2018). http://www.countyhealthrankings.org
Eat Smart Move More NC. (2007). Edgecombe County: Eating Smart and Moving More. Retrieved from Eat Smart Move More NC website: https://www.eatsmartmovemorenc.com/CountyProfiles/Texts/Edgecombe%20County.pdf
Essential Weight Loss website. (2018). https://www.essentialweightloss.com
Heymsfield, S., & Wadden, T. (2017, January 19, 2017). Mechanisms, Pathophysiology, and Management of Obesity. The New England Journal of Medicine, 376, 254-266. https://doi.org/10.1056/NEJMra1514009
Kumar, R., & Arrone, L. (2017). Pharmacologic Treatment of Obesity. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279038/
McCance, K., & Huether, S. (2014). Pathophysiology: The Biologic Basis for Disease in Adults and Children (7 ed.). Retrieved from https://wgu.vitalsource.com
Medicaid.gov website. (2018). https://www.medicaid.gov/
National Guideline Clearinghouse (NGC). (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Retrieved from https://www.guideline.gov/summaries/summary/48339/2013-ahaacctos-guideline-for-the-management-of-overweight-and-obesity-in-adults-a-report-of-the-american-college-of-cardiologyamerican-heart-association-task-force-on-practice-guidelines-and-the-obesity-society?q=obesity
NIH study finds extreme obesity may shorten life expectancy up to 14 years. (2014). Retrieved from https://www.nih.gov/news-events/news-releases/nih-study-finds-extreme-obesity-may-shorten-life-expectancy-14-years
Nishiyama, T. (2012). Nauru: An island plagued by obesity and diabetes. Retrieved from https://web.archive.org/web/20140528121809/http://ajw.asahi.com/article/globe/feature/obesity/AJ201205270051
North Carolina Medical Board website. (2017). https://www.ncmedboard.org/
North Carolina’s plan to address obesity: healthy weight and healthy communities. (2013). Retrieved from https://www.eatsmartmovemorenc.com/ESMMPlan/Texts/NC%20Obesity%20Prevention%20Plan%202013-2020_LowRes_FINAL.pdf
Robert Wood Johnson Foundation. (2013). Nash and Edgecombe Counties, NC. Retrieved from http://www.healthykidshealthycommunities.org/communities/nash-and-edgecombe-counties-nc
Senauer, B. (2006). Why Is the Obesity Rate So Low in Japan and High in the U.S.? Some Possible Economic Explanations. Working Papers 14321. University of Minnesota, The Food Industry Center.
The Down East Partnership for Children website. (2018). http://depc.org/
The State of Obesity website. (2018). https://stateofobesity.org/
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Nutrition"
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:



