Relationship Between Pregnancy, Childbirth and IPV
Info: 38563 words (154 pages) Dissertation
Published: 16th Dec 2019
Chapter 1
Introduction |
The chapter introduces the social and health problem of intimate partner violence (hereafter referred to as IPV[1]), highlights gaps in the research on IPV around the time of pregnancy in Bangladesh, and outlines the aims of the current research. It also provides a layout of the dissertation.
1.1 Contextualizing the problem
Pregnancy has been described as a life-changing event for women, introducing a range of new trials and tribulations. On the one hand, pregnancy is often a time of happiness and expectancy characterized by maternal optimism, emotional uplifts and growing social support (DiPietro, Hilton, Hawkins, Costigan, & Pressman, 2002; Ogbonnaya, Kupper, Martin, Macy, & Bledsoe-Mansori, 2013). Culturally, pregnancy is often viewed as a time of happiness and expectancy in women’s lives, with the welcoming of the next generation and growing anticipation of the joys a new child will bring to the family. However, pregnancy can also be a stressful and anxiety-provoking life event (Bondas & Eriksson, 2001) since it is a major life transition (Bost, Cox, Burchinal, & Payne, 2002) and, for some women, poses a maturational crisis they are ill-prepared for (Bondas & Eriksson, 2001). Regrettably, pregnancy can also introduce an increased risk for experiencing intimate partner violence (IPV) for millions of women of reproductive age worldwide (Chang et al., 2005; Devries et al., 2010; Garcia-Moreno & Watts, 2011; James, Brody, & Hamilton, 2013; Kendall-Tackett, 2007). IPV is the most frequent form of violence against women and includes acts of physical, sexual and psychological coercion as well as controlling behaviours by a current or former intimate partner or husband (World Health Organization (WHO) & Pan American Health Organization (PAHO), 2012).
Home is often considered as a haven for women and children, where there is physical and psychological safety, trust and care (Fisher et al., 2013). However, partner violence is a complete contravention of this and makes what should be a place of safety, an environment characterized by threat (Dobash & Dobash, 1979). It occurs among all socioeconomic, religious, cultural backgrounds, heterosexual or same-sex couples, and perpetration can be bidirectional (Campbell et al., 2002; Ellsberg, 2006; Krug, Dahlberg, Mercy, Zwi, & Lozano, 2002; Watts & Zimmerman, 2002). While estimates vary widely, population-based studies indicate that anywhere from 15–71% of women experience IPV worldwide (Ellsberg & Heise, 2005; Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006). A recent meta-analysis that included studies from the US as well as other developed and developing countries, established the prevalence of IPV during pregnancy to be between 4.8% and 63.4% (James, Brody, & Hamilton, 2013). Although, there is no conclusive evidence that women who are pregnant are at greater risk for IPV victimisation (Campbell, Garcia-Moreno, & Sharps, 2004; Devries et al., 2010; Macy, Martin, Kupper, Casanueva, & Guo, 2007; Martin, Mackie, Kupper, Buescher, & Moracco, 2001; Saltzman, Johnson, Gilbert, & Goodwin, 2003), evidence suggests that a significant number of women are exposed to IPV at this vulnerable period, which in turn, jeopardise their lives (Devries et al., 2010; James, Brody, & Hamilton, 2013; Taillieu & Brownridge, 2010).
IPV has a multidimensional radiating impact on women’s lives; it affects women’s physical, sexual, mental and reproductive health (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; Plichta, 2004; Trabold, Waldrop, Nochajski, & Cerulli, 2013), and well-being (Krantz, 2002; Riger, Raja, & Camacho, 2002). IPV damages women’s capacities to pursue education and work (McCloskey et al., 2007; Nurius et al., 2003) resulting in increased risk of poverty, divorce and unemployment (Byrne, Resnick, Kilpatrick, Best, & Saunders, 1999; Salomon, Bassuk, & Browne, 1999). It causes more deaths and incapacity among women of reproductive age than cancer, traffic accidents and malaria combined (Gomez-Beloz, Williams, Sanchez, & Lam, 2009). Along with physical and emotional impacts, victims of IPV have also lost a total of approximately 8 million days of paid work yearly, equivalent to 32,000 full-time jobs due to IPV in the US (National Center for Injury Prevention and Control, 2003). Each year IPV costs the US economy $12.6 billion (WHO, 2004) and the Australian economy $13.6 billion (Australian Bureau of Statistics (ABS), 2013). Homicide is the most extreme consequence of IPV (WHO, 2011). IPV during pregnancy poses a grave risk to two lives – mothers and unborn babies.
IPV during pregnancy is a crucial public health risk and has implications for the health and welfare of the mother, the developing fetus and the newborn during gestation, birth and postpartum (Cha & Masho, 2014; de Jager, Skouteris, Broadbent, Amir, & Mellor, 2013; Islam, Baird, Mazerolle, & Broidy, 2017; Kendall-Tackett, 2007; Lau & Chan, 2007; Leneghan, Gillen, & Sinclair, 2012; Liou, Wang, & Cheng, 2014; Trabold, Waldrop, Nochajski, & Cerulli, 2013). Established direct health consequences of IPV during pregnancy include increased risk of unwanted pregnancy, preterm birth, miscarriage (Shah & Shah, 2010), low birth weight (Bonomi et al., 2006; Dillon, Hussain, Loxton, & Rahman, 2013), emotional distress, depression, anxiety, posttraumatic stress disorder and low self-esteem (Howard, Oram, Galley, Trevillion, & Feder, 2013; Yoshihama, Horrocks, & Kamano, 2009). Indirect health consequences include substance abuse (Datner, Wiebe, Brensinger, & Nelson, 2007; Lipsky, Holt, Easterling, & Critchlow, 2005; Sarkar, 2008), constrained access to antenatal care (Bailey & Daugherty, 2007; Cha & Masho, 2014), insufficient weight gain during pregnancy (McFarlane, Campbell, Sharps, & Watson, 2002; Shadigian & Bauer, 2004), disturbances in maternal-child bonding (Janssen et al., 2003; Sharps, Laughon, & Giangrande, 2007; Trabold, Waldrop, Nochajski, & Cerulli, 2013) and early cessation of exclusive breastfeeding (Islam, Baird, Mazerolle, & Broidy, 2017; Taveras et al., 2003). IPV-related homicide is the leading cause of maternal mortality (Chang, Berg, Saltzman, & Herndon, 2005; Cheng & Horon, 2010), accounting for 13% to 24% of all deaths among pregnant women (Plichta, 2004). Once considered a family matter, IPV is now increasingly recognized as a social problem, a critical global health concern (WHO & PAHO, 2012) and a fundamental human rights issue (Amnesty International, 2004; WHO, 2006) due to its deleterious consequences on women.
Because IPV generally occurs in private, many instances of IPV are rarely reported (Flury, Nyberg, & Riecher-Rössler, 2010; Keeling & Mason, 2011), and victims often fear that reporting will increase their risk of potential harm. Additionally, women consider the trade-offs between suffering from IPV and tarnishing their social reputation, which contributes to the low reporting of IPV (Khatun & Rahman, 2012). However, in the past two decades, there has been a dramatic increase in the scope and breadth of research interest in IPV across various disciplines, including criminology, psychology, public health, social work and sociology (Loue, 2001). It is a problem beyond criminal justice, impacting health, legal, economic, education, development, and human rights as well (Malyadri, 2013). After decades of global feminist activism, international institutions now recognize the significance of violence against women (Cook & Kaya, 2010). In 1993, the United Nations began a major initiative targeting violence against women (Johnson, Ollus, & Nevala, 2007), and the WHO now defines violence against women as a serious threat to women’s health, and has been running a major research initiative (Ellsberg & Heise, 2005) in an attempt to address the devastating effects of IPV worldwide.
Although our understanding regarding the risks of IPV during pregnancy is progressing, notable gaps remain. Currently, most of the research on the prevalence, correlates and consequences of IPV during pregnancy and postpartum period have been thoroughly examined in high-income countries (Annan, 2008; Brown, McDonald, & Krastev, 2008), although IPV during pregnancy is commonly occurred in low-and-middle-income countries (27.7%–32%) compared with high-income countries (12%–13.3%) (Devries et al., 2010; James, Brody, & Hamilton, 2013). Limited research has explored these issues in low-income countries including Bangladesh (Fisher et al., 2012; Nasir & Hyder, 2003; Taillieu & Brownridge, 2010). According to Taillieu and Brownridge (2010), IPV during pregnancy in low-income countries is a relatively new area of investigation, and thus, less is known about factors contributing to violence during pregnancy and following childbirth in developing nations. The majority of research has focussed primarily on physical and/or sexual IPV (Howard, Oram, Galley, Trevillion, & Feder, 2013; Scribano, Stevens, & Kaizar, 2013; WHO, 2011). Little is known about the prevalence and correlates of sexual and psychological IPV during pregnancy, although sexual and psychological IPV around the time of pregnancy are proven to have detrimental consequences for women and their children (Chan et al., 2011; Taillieu & Brownridge, 2010; WHO, 2011). Given the potentially profound effects that IPV during pregnancy can have on the physical and mental wellbeing of women and their children, we also need to understand the impact of IPV on pregnant women’s health seeking behaviour in developing countries (Koski, Stephenson, & Koenig, 2011). Comprehensive research focusing on IPV and women’s mental health is scarce (Hegarty, 2011), and it is unclear how the experience of IPV before, during and after pregnancy affects women’s psychological health during the postpartum period (Reichenheim, Moraes, Lopes, & Lobato, 2014). Additionally, IPV during pregnancy may compromise women’s exclusive breastfeeding (EBF, only breast milk until 6 months of age, and thereafter its complementation with safe foods until the child reaches ≥ 2 years) efforts, which can further compromise the health of their newborn. Few studies have examined the influence of IPV on the continuation of EBF (Kendall-Tackett, 2007; Lau & Chan, 2007; Moraes, Oliveira, Reichenheim, & Azevedo, 2011), and therefore the association is poorly understood in the literature (Henderson, Evans, Straton, Priest, & Hagan, 2003).
In summary, there are significant gaps in the knowledge and understanding of IPV around the time of pregnancy, and the influence of different forms of IPV before, during and after pregnancy on maternal health service utilization, maternal mental health, and breastfeeding practices especially in low- and middle-income countries including Bangladesh. To improve the health of expectant mothers and their infants, it is important to investigate the potential correlates for, the co-occurring nature and patterns and the consequences of IPV around the time of pregnancy (Brownridge et al., 2011).
1.2 Setting the context: Bangladesh
1.2.1 Overview of Bangladesh
The people’s republic of Bangladesh is a developing country located in South Asia. With over 160 million people in a 147,570 km2 land mass, it is world’s eighth-most populous country, and one of the most densely-populated (~1,077/ km2) nations in the world (GOB, 2016). The per-capita income is estimated at US$1,466 for the fiscal year 2016 compared to the world average of US$14,301 (GOB, 2016). Eighty-three percent of the population lives on less than US$2 per day, 25% on less than US$1 per day, and 31.5% of people live below the international poverty line of a per capita income of US$ 1.25 per day (United Nations Development Programme (UNDP), 2015). Adult literacy rate (15+ years) for both sexes is 63.6% and male-female ratio is 100.3:100 (GOB, 2016). In 2015, among 188 countries, Bangladesh ranked 142nd position in the Human Development Index, and 111th position in the Gender Inequality Index (UNDP, 2015). The low ranking in the gender inequality index implies that there is significant inequality in income and education between males and females in the society of Bangladesh.
1.2.2 Prevalence of IPV in Bangladesh
Bangladesh has the highest prevalence of sexual and physical IPV among South Asian countries, and it ranks second in the World Bank top 15 countries with the highest global prevalence of physical IPV (Solotaroff & Pande, 2014). The WHO multi-country study states that the lifetime prevalence of physical IPV in Bangladesh ranges from 40%–42%, the sexual IPV ranges from 37–50% and either physical or sexual IPV or both ranges from 53–62% (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006). The Bangladesh Demographic and Health Survey (BDHS)-2007 reports 48% of ever-married women have experienced physical IPV (NIPORT et al., 2009). Other studies from Bangladesh have reported the past year or current prevalence of physical IPV to be between 16–52% (Dalal, Rahman, & Jansson, 2009; Kabir, Nasreen, & Edhborg, 2014; Sambisa et al., 2010), sexual IPV between 11–65% (Bangladesh Bureau of Statistics (BBS), 2013; Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; Kabir, Nasreen, & Edhborg, 2014; Naved, 2013), and psychological IPV between 24–84% (Dalal, Rahman, & Jansson, 2009; Kabir, Nasreen, & Edhborg, 2014).
A number of Bangladeshi studies have documented the prevalence of IPV in general, however, a few of them also inquired about its presence during pregnancy. These studies indicated a range of 10–22% of the ever-pregnant women experienced physical IPV (Åsling‐Monemi, Tabassum Naved, & Persson, 2008; Bates, Schuler, Islam, & Islam, 2004; Kabir, Nasreen, & Edhborg, 2014; Naved & Persson, 2008), 10–21% experienced sexual IPV (Hadi, 2000; Kamal, 2013) and 38% experienced psychological IPV during pregnancy (Bhuiya, Sharmin, & Hanifi, 2003). Regardless of the varied prevalence rates across studies, what is abundantly clear is that violence against women in Bangladesh is widespread so much so that the UNICEF defines IPV in Bangladesh as one of the most blatant manifestations of gender asymmetry (United Nations Children’s Fund (UNICEF), 2011).
1.2.3 Rationale for IPV study in Bangladesh
Maternal and child health has traditionally been considered an important indicator of the health progress and the overall social and economic well-being of a country (Abedin, Islam, & Hossain, 2008). Although considerable progress has been made in reducing maternal mortality globally, Bangladesh remains a leader in maternal mortality, with a ratio of 170 per 100,000 live births in 2013 (WHO, 2014a). It is well recognised that low use of prenatal care (Jasinski, 2004), limited postnatal care (Chakraborty, Islam, Chowdhury, Bari, & Akhter, 2003; Chaudhury, 2008; Kidney et al., 2009), and low birth assistance and attendance by a medically trained professional (Choudhury, Hanifi, Rasheed, & Bhuiya, 2000; Ronsmans et al., 2009) contributes to high maternal and child mortality. Research has begun to investigate the influence of other psychosocial risk factors on maternal and child health.
In South Asian countries including Bangladesh, family planning, major infectious diseases and malnutrition have been on the top of the public health priorities (Hosain, Chatterjee, Ara, & Islam, 2007). IPV has not been acknowledged as a significant public health concern in South Asian nations, and this is especially true in Bangladesh, and thus, it has never received considerable attention at the policy level or in the planning of health frameworks and research (Salam, Alim, & Noguchi, 2006). A study conducted by Afsana, Rashid, Thurston, & BRAC (2005) reviewed existing health policies and plans, interviewed policy makers, service providers and women, and identified some of the challenges and gaps in addressing violence against women in the health policy of Bangladesh. These include (1) absence of government’s concrete policies to address domestic violence and associated health issues; (2) lack of understanding or sensitivity to the issue of IPV and how it affects women’s health; (3) insufficient and weak laws in tackling IPV; (4) inadequate safety and security of victims and individuals working with the abused women; (5) lack of shelter homes; (6) inadequate support for counselling; and (7) lack of adequate training and awareness of health care providers, police, lawyers and other relevant service providers. Without a clear knowledge and understanding of IPV during pregnancy, health care providers, social workers and other service providers are underprepared for the challenges of treating IPV victims.
Despite the increase in the prevalence rate of IPV in Bangladesh, at present, there is little information on IPV during pregnancy and following childbirth. Almost all the research so far has been conducted in the U.S and other developed countries that are not representative of or generalizable to women of Bangladesh. A growing number of studies have been undertaken in Bangladesh to explore significant correlates and consequences of IPV victimization, however, most studies have only considered women of reproductive age in general, and have not investigated the experience of IPV during pregnancy. Only a single study conducted by Naved and Persson (2008) focuses on pregnant women’s experiences on physical IPV only. Except for the single study by Rahman et al. (2012) which ascertained the effect of physical and sexual IPV (did not examine psychological IPV ) on maternal health services utilization using the BDHS-2007 data, no other studies in Bangladesh have specifically examined the impact of IPV during pregnancy on the receipt of prenatal care. At present, there are very few studies in Bangladesh that have examined the prevalence of psychological or sexual IPV during pregnancy nor are there studies that have examined physical, sexual or psychological IPV during the postpartum period. Currently, there are no studies that have focused on maternal exposure to IPV during and after pregnancy, which is independently associated with postpartum depression. Furthermore, no studies in Bangladesh have investigated the effect of IPV during pregnancy on mother’s exclusive breastfeeding efforts.
Addressing the abovementioned gaps, the present study examines IPV victimization during pregnancy. It also explores the influence of IPV around the time of pregnancy on the timing of entry into prenatal care, experiencing postpartum depression and exclusive breastfeeding among women in Bangladesh.
1.3 Purpose of the study
According to Taillieu and Brownridge (2010) research on IPV during pregnancy lacks a guiding theoretical framework. There is also a global gap in the understanding of the relationship between pregnancy, childbirth and IPV. The study aims to fill some of the important gaps in the empirical evidence to help explain the prevalence, correlates and consequences of different forms of IPV before, during and after pregnancy. Currently, our understanding of the influence of IPV during pregnancy on exclusive breastfeeding practices is very limited and therefore, it is envisaged that the findings from this study will help to permeate the theoretical gap in this area. Policy makers should have a comprehensive understanding of how gender inequity increases the risk of IPV and affects the health of women and children. The research findings from this study will have implications in formulating policy and programs for IPV prevention strategies as well as maternal and child health improvement in Bangladesh and in other similar settings. Furthermore, findings from the research will also inform culturally specific educational programs on IPV for healthcare professionals, social workers, and for the women themselves in Bangladesh and other developing countries.
Pregnancy is one of the few times when almost all women need to visit health care settings on several occasions, thereby providing an opportunity for health professionals to identify IPV by routine enquiry, provide health-related services, and facilitate access to non-health support services (Jeanjot, Barlow, & Rozenberg, 2008; Martin & Garcia, 2011). Currently, Bangladesh does not have a screening protocol. The findings from this study will provide the basis for preparing nationally appropriate guidelines that would aid in the identification of women experiencing or at risk for IPV, and facilitate appropriate intervention including supportive referral and proper counseling by trained health care providers and social workers.
1.4 Research Questions
The research aims to answer two questions:
RQ1 How do pregnancy and the postpartum period influence the prevalence of IPV?
RQ2 Does IPV influence delayed entry into prenatal care, postpartum depression and mother’s exclusive breastfeeding?
1.5 Aims of the study
To address the first research question, this study broadly examines IPV victimisation during pregnancy among women in Bangladesh with specific aims to:
Aim-1: Examine IPV victimisation for pregnant women in Bangladesh.
| Aim 1.1 | : | Determine the prevalence of different forms of IPV before, during and after pregnancy; |
| Aim 1.2 | : | Examine the changing patterns of IPV victimisation before, during and after pregnancy; |
| Aim 1.3 | : | Identify and describe potential correlates of different types of IPV victimisation during pregnancy. |
To detail the impacts of IPV on the health of mothers and babies, the study addresses the following specific aims:
Aim-2: Explore the health consequences of IPV victimisation for pregnant women in Bangladesh.
1.6 Thesis framework
The thesis is structured in five portions including introduction, literature review, research process, research contribution and conclusion and consists of eight chapters (as shown in Figure 1.1).
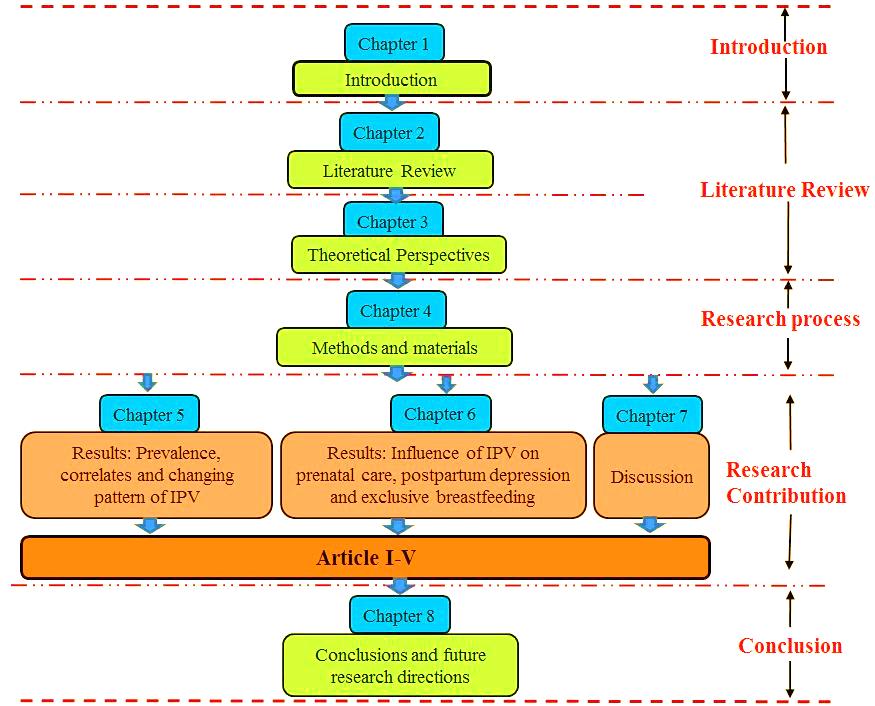
Figure 1.1: Thesis Framework
Introduction
Chapter 1 contextualises the problem of IPV during pregnancy and postpartum period. It explores the Bangladeshi context including the prevalence of IPV. This chapter also provides the purpose, objectives and research questions of the study.
Literature review
Chapter 2 presents a review of the available literature on IPV and pregnancy-prevalence and changing pattern of IPV both during and after pregnancy and potential correlates of IPV during pregnancy that has relevance with the cultural context of Bangladesh. It also elaborately illustrates direct and indirect consequences of IPV before, during and after pregnancy.
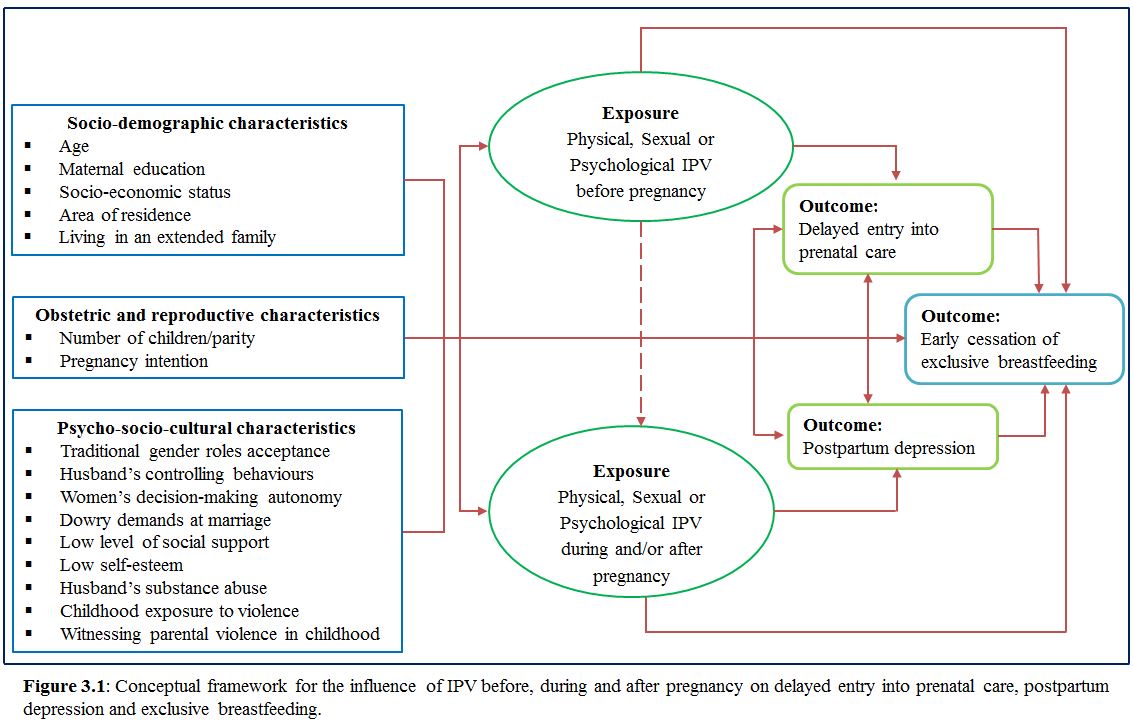
Chapter 3 depicts the contextual reasons for IPV victimization during pregnancy followed by the theoretical perspectives of IPV. Among theories, feminist theory, social learning theory and evolutionary psychological theory are elaborately explained. At the end of this chapter, a conceptual framework has been developed based on the theories and past literature of IPV.
Research process
Chapter 4 focuses the methodology of the study. This part consists of study design, data collection sites, sample of the study, detailed procedure in undertaking the study and research instruments. Finally, ethical considerations are highlighted in this chapter.
Research contribution
During the PhD candidature, the candidate made a considerable contribution to five published and unpublished peer-reviewed journal articles (two has already been published and three are under review), which confirms the originality of this research (presented in Chapter 5, 6 and 7, as shown in Table 1.1). Paper I addresses research aim 1.1 and 1.2. Paper II, III, IV and V address aim 1.3, 2.1, 2.2 and 2.3 respectively. The articles are listed as follows:
Table 1.1: Published and unpublished articles from this thesis
| Articles | Descriptions | Current status | |
| Paper I | : | Islam, M.J., Broidy, L., Mazerolle, P., and Baird, K. Exploring intimate partner violence before, during and after pregnancy in Bangladesh, Justice Quarterly. | Under review |
| Paper II | : | Islam, M.J., Mazerolle, P, Broidy, L., and Baird, K. Exploring the prevalence and correlates associated with intimate partner violence during pregnancy in Bangladesh, Journal of Interpersonal Violence. | Under review |
| Paper III | : | Islam, M.J., Broidy, L., Baird, K., and Mazerolle, P. (2017). Exploring the associations between intimate partner violence and delayed entry to prenatal care: Evidence from a cross-sectional study in Bangladesh, Midwifery. 47:43-55. | Published |
| Paper IV | : | Islam, M.J., Broidy, L., Baird, K., and Mazerolle, P. Intimate partner violence around the time of pregnancy and postpartum depression: The experience of women of Bangladesh, PLoS One. | Under review |
| Paper V | : | Islam, M.J., Baird, K., Mazerolle, P., and Broidy, L. (2017). Exploring the influence of psychosocial factors on exclusive breastfeeding in Bangladesh, Archives of Women’s Mental Health. 20 (1): 173-188. | Published |
Analytical results and significance of the findings are discussed in chapter 5–7.
Chapter 5 presents the analytical results of aim 1 (RQ1). Prevalence, potential risk factors of IPV during pregnancy, and changing pattern of IPV throughout the pregnancy are identified and described in this chapter.
Chapter 6 discusses the analytical results of aim 2 (RQ2). The influence of IPV on the timing of entry into prenatal care, postpartum depression and mother’s exclusive breastfeeding are explored in this chapter.
Chapter 7 discusses the significance of the findings outlined in chapter 5 and chapter 6 in light of past studies and theoretical frameworks.
Conclusion
To conclude, chapter 8 presents the summary of the core research findings extracted from the study. Having outlined the limitations of the research, the outlook for future research directions is also stated in this chapter.
Chapter 2
Literature Review: Prevalence, correlates and consequences of IPV during pregnancy |
The prevalence of IPV directed at pregnant women in both developed and developing countries remains elusive and varies widely from study to study depending on how IPV has been assessed. Variation in IPV prevalence estimates may be due to actual differences in the prevalence of violent acts within different study populations, as well as differences in methodologies, definitions and cultural aspects among studies that make it difficult to compare the results (Jasinski, 2004; Jeanjot, Barlow, & Rozenberg, 2008; Taillieu & Brownridge, 2010). With varied prevalence rates of IPV, a number of risk factors relevant to understanding the risk of IPV during pregnancy are also available in the literature. In the first part of this chapter, the prevalence of IPV during and after pregnancy, and the patterns of IPV experienced by pregnant women are discussed. Further, the factors that put women at risk for experiencing IPV during pregnancy and the negative consequences of IPV during pregnancy are demonstrated in the later part of this chapter.
2.1 Prevalence of IPV during pregnancy
Gazmararian et al.’s (1996) review, synthesizing the results of 13 studies from the USA and other developed countries reveals that the prevalence of IPV against pregnant women ranges from 0.9% to 20.6%, with most studies reporting estimates between 3.9% and 8.3% (Gazmararian et al., 1996; Martin, Mackie, Kupper, Buescher, & Moracco, 2001; Saltzman, Johnson, Gilbert, & Goodwin, 2003). Another review of six studies from developing countries (including India, China, Pakistan and Ethiopia) reports that the prevalence of IPV during pregnancy is between 4% and 29% (Nasir & Hyder, 2003). A review of 19 studies from some African countries has documented that 8 to 57.1% pregnant women experience IPV during pregnancy (Shamu, Abrahams, Temmerman, Musekiwa, & Zarowsky, 2011). Another systematic review consolidating findings from both developed and developing nations has documented the prevalence as 0.9-30% physical violence, 1-3.9% sexual violence, and 1.5-36% psychological violence during pregnancy (Taillieu & Brownridge, 2010). A recently published meta-analysis synthesizing the results of 92 studies from both developed and developing countries reports that the prevalence of IPV against pregnant women varies between 4.8% in China and 63.4% in Brazil (James, Brody, & Hamilton, 2013). This review also reveals that the prevalence of psychological IPV to be 28.4%, physical IPV to be 13.8% and sexual IPV during pregnancy to be 8%. Notably, the prevalence of IPV against pregnant women appears to be higher in African and Latin American countries compared to the Asian and European countries (Devries et al., 2010).
The literature contains mixed results concerning whether pregnancy is a vulnerable period for IPV and whether IPV escalates in severity during pregnancy. A number of factors are responsible for these discrepancies. First, IPV (e.g. physical, sexual, and/or psychological) has been defined differently from study to study (McMahon & Armstrong, 2012). IPV measurements that include multiple items and consider a number of different types of violence tend to result in the highest prevalence rates (Farid, Saleem, Karim, & Hatcher, 2008; Perales et al., 2009). Furthermore, IPV has been assessed with a range of instruments including the Conflict Tactics Scales, the Danger Assessment Scale, the Abuse Assessment Scale and the Index of Spouse Abuse, among other instruments. Second, the pregnancy period has been defined variously, up to one-year pre- or post-delivery (McMahon & Armstrong, 2012). Third, prevalence rates vary whether national or community samples are used, with community samples reporting more violence than national samples (Bailey & Daugherty, 2007; James, Brody, & Hamilton, 2013; Jasinski, 2004). Fourth, prevalence rates also vary whether population-based samples or hospital or clinic-based samples are used. Notably, population-based studies have found lower rates of IPV than hospital-based samples (Guo, Wu, Qu, & Yan, 2004b; James, Brody, & Hamilton, 2013; Janssen et al., 2003; Yost, Bloom, McIntire, & Leveno, 2005). Fifth, the prevalence is higher in low-income countries in comparison to high-income countries and within countries, it is higher in rural areas than in urban areas (Fanslow, Silva, Robinson, & Whitehead, 2008; Naved & Persson, 2008; Peek-Asa et al., 2011; Valladares, Pena, Persson, & Hogberg, 2005). Sixth, prevalence rates vary depending on the timing of inquiry (e.g. single point early in pregnancy vs. multiple points during pregnancy). Finally, the mode of inquiry (Self-administered questionnaire vs face-to-face interview) also plays an important role in estimates of prevalence rate. Higher prevalence rates have been associated with in-person interviews than self-administered questionnaire (Gazmararian et al., 1996).
Although the prevalence of IPV during pregnancy vary, it is clear that a significant number of women experience IPV during pregnancy. For this thesis, a comprehensive search of the current studies has been undertaken on the prevalence of IPV before, during and after pregnancy. The results are summarized in Table 2.1.
2.2 Prevalence of IPV during postpartum period
The postpartum period begins immediately after the birth of the baby and extends up to six weeks (WHO, 2014b) to six months after birth (Brown, Posner, & Stewart, 1999). Since most deaths occur during the postpartum period, WHO describes this period as the most critical and yet, the most neglected phase in the lives of mothers and babies (WHO, 2014b).
A number of studies have demonstrated that the risk of IPV associated with pregnancy is not only limited to the time between conception and birth, but also the period of one year before conception until one year after childbirth (Charles & Perreira, 2007; Jasinski, 2004; Martin et al., 2004; Saltzman, Johnson, Gilbert, & Goodwin, 2003; Taillieu & Brownridge, 2010). An increasing number of studies have shown that the postpartum period is also a time of increased risk for IPV victimisation (Ezechi et al., 2004; Hedin, 2000; Macy, Martin, Kupper, Casanueva, & Guo, 2007; Martin et al., 2004; Silva, Ludermir, de Araujo, & Valongueiro, 2011; Woolhouse, Gartland, Hegarty, Donath, & Brown, 2012). Previous studies have reported that IPV during the postpartum period ranges from 2–25% (Charles & Perreira, 2007; Gartland, Hemphill, Hegarty, & Brown, 2011; Hellmuth, Gordon, Stuart, & Moore, 2013; Saito, Creedy, Cooke, & Chaboyer, 2012; Silva, Valongueiro, Araújo, & Ludermir, 2015).
One longitudinal study has reported that the rates of psychological and sexual IPV are the highest during the first month after the birth of the infant (Macy, Martin, Kupper, Casanueva, & Guo, 2007). One study reports that the prevalence of physical IPV in the postpartum period is around eight times higher in women who have also experienced IPV during pregnancy as compared to those who have not (Moraes et al., 2011). Another study has revealed that physical IPV among young mothers is as high as 21.3% at 3 months postpartum, and 78% of these women have reported no IPV before pregnancy (Harrykissoon, Rickert, & Wiemann, 2002). In the same study, 75% of mothers experienced IPV during their pregnancies also reported IPV within 24 months following birth.
Table 2.1: Worldwide prevalence of IPV during pregnancy and postpartum period from previous research
| Author(s) (year) | Country/ Region | Setting | Sample Size | Type of Sample | Design | Instrument | Percentage | ||
| Before pregnancy/ lifetime | During pregnancy | After birth | |||||||
| (Scribano, Stevens, & Kaizar, 2013) | USA | P | 10,855 | First time and low-income mothers, ≥ 13 years old. | Longitudinal | AAS | 8.1 % | 4.7 % | 12.4 % |
| (Koenig et al., 2006) | USA | C | T1: 634
T2: 485 |
Pregnant women with HIV | Prospective, correlational (late pregnancy and 6 months postpartum) | Questionnaire | Not reported | 8.9% (physical or sexual) | 4.9% (physical or sexual) |
| (Dunn & Oths, 2004) | USA/ Alabama | H | 439 | Pregnant women, 20-34 years of age | Prospective, correlational | AAS | 15% | 10.9% (physical) | Not reported |
| (Daoud et al., 2012) | Canada | P | 6421 | Postpartum women (5-14 months), aged ≥15 years. | Cross-sectional | Questionnaire | 6% (physical & sexual) | 1.4% (physical & sexual) | 1% (physical & sexual) |
| (Heaman, 2005) | Canada/ Manitoba | H | 680 | Postpartum mothers | Cross-sectional | AAS | 9.1% (physical) 1.9% (sexual) Lifetime: 36.7% (physical, psychological) | 5.7% (physical) | Not reported |
| (Bacchus, Mezey, & Bewley, 2004) | UK/Bristol Avon | P | 200 | Pregnant women, aged ≥16 years | Cross-sectional | AAS | 10.6% (physical) 23.4% (sexual) Lifetime: 23.5% (physical) | 3% (physical) 1% (sexual) | Not reported |
| (Bowen, Heron, Waylen, & Wolke, 2005) | UK/ Bristol Avon | P | 7591 | Pregnant mothers | Prospective longitudinal cohort (18 weeks of gestation, 8 weeks, 8 months, 21 months and 33 months postpartum) | Questionnaire | Not reported | 1% (physical) 4.8% (psychological) | 1.8% (physical) 7.3% (psychological) (at 8 months) |
| (Thananowan & Heidrich, 2008) | Thailand/ Bangkok | H | 475 | Pregnant women, aged ≥ 18 | Cross-sectional | AAS | 9.9% (Physical) 4.8% (sexual) | 4.8% (physical) | Not reported |
| (Perales et al., 2009) | Peru/ Lima | H | 2,392 | Postpartum mothers, 15 – 49 years age, | Cross-sectional | DHS Domestic Violence Module | Lifetime: 45.1% (any)34.2% (physical)8.7% (sexual)28.4% (psychological) | 21.5% (any) 11.9% (physical), 3.9% (sexual), 15.6% (psychological) | Not reported |
| (Farid, Saleem, Karim, & Hatcher, 2008) | Pakistan/ Karachi | H | 500 | Pregnant women, age 15-49 years. | Cross-sectional | WHO’s Domestic Violence Module. | 28.4% (physical) 49.8% (psychological) | 12.6% (physical) 43.2% (psychological) | Not reported |
| (Peedicayil et al., 2004) | India/Bhopal, Chennai, Delhi, Lucknow, Nagpur, Trivandrum and Vellore | P (Rural & Urban) | 9938 | Women of 15 to 49 years old who were living with a child younger than 18 years. | Cross-sectional | Questionnaire | 23% (physical) | 18% (physical) | Not reported |
| (Karaoglu et al., 2005) | Turkey/ Malatya | P (Urban & Rural) | 824 | Pregnant women | Cross-sectional | Questionnaire (developed from AAS) | 16.3% (physical), 8.5% (sexual) 30.8% (Psychological) | 8.1% (physical) 9.7% (sexual) 26.7% (Psychological) | Not reported |
| (Díaz-Olavarrieta et al., 2007) | Mexico/ Mexico City | H (public) | 1311 | Pregnant women, | Longitudinal (once in each trimester (<20 weeks, 20.1–36 weeks, >36.1 weeks) | A composite case record form adapted from AAS and other instruments. | 11.1% (physical and/or sexual) Lifetime: 41% (physical, sexual) | 7.6% (physical and/or sexual) 6.7% (physical) 1.8% (sexual) | Not reported |
| (Fawole, Hunyinbo, & Fawole, 2008) | Nigeria/ Abeokuta | H | 534 | Pregnant women, | Cross-sectional | A 21-item semi-structured questionnaire | 14.2% | 2.3% | Not reported |
| (Guo, Wu, Qu, & Yan, 2004b) | China/ Tianjing, Liaoning, Henan, and Shaanxi | P | 12,044 | Women with children aged 6–18 months | Cross-sectional | Questionnaire | 8.5% (physical, sexual) 4.2% (physical) 5.8% (sexual) | 3.6% (physical, sexual) 1.3% (physical) 2.8% (sexual) | 7.8% (physical, sexual) 3.8% (physical) 4.9% (sexual) |
| (Ludermir, Valongueiro, & Araújo, 2014) | Brazil/ Recife | C | 1,120 | Pregnant women of 18-49 years old | Cross-sectional | Questionnaire | Not reported | 31% (any type) 16.6% (psychological) | Not reported |
| (Van Parys, Deschepper, Michielsen, Temmerman, & Verstraelen, 2014) | Belgium/ Flanders | C | 1894 | Pregnant women, aged ≥ 18 | Cross-sectional | Questionnaire (developed from AAS) | 14.3% (overall) 2.3% (physical) 0.6 (sexual) 13.6 (psychological) | 10.6% (overall) 0.8% (physical) 0.5 (sexual) 10.1 (psychological) | Not reported |
| (Clark, Hill, Jabbar, & Silverman, 2009) | Jordan | C | 390 | Ever-married women who visited family planning clinics. | Cross-sectional | Questionnaire (developed from WHO’s Multi-Country Study) | 8% (physical) | 15% (physical) | Not reported |
| (Kabir, Nasreen, & Edhborg, 2014) | Bangladesh/ Mymensingh | P | T1=720
T2=660 |
Pregnant women | Longitudinal | Questionnaire (developed from WHO’s Multi-Country Study) | Lifetime 70% (physical) | 18% (physical) | 52% (physical) 65% (sexual) 84% (psychological) |
| (Mohammadhosseini, Sahraean, & Bahrami, 2010) | Iran/ Jahrom | C | 300 | Married women with a child aged 6 to 18 months | Cross-sectional | Questionnaire (developed from previous studies) | 52% (any type), 17% (physical), 21% (sexual) 42% (psychological) | 42% (any type) 10% (physical) 17% (sexual) 33% (psychological) | 54% (any type) 15% (physical) 25% (sexual) 43% (psychological) |
Note: P: Population-based, C= Clinic-based, H= Hospital-based, AAS: Abuse Assessment Screen, CTS2 = Conflict Tactics Scale 2,
2.3 Changing patterns of IPV during pregnancy
A debate continues in the literature whether pregnancy provides a time of protection or increased risk for IPV. Varied prevalence rates of IPV during pregnancy across literature have intensified the debate largely (Taylor & Nabors, 2009). Some argue that IPV may increase during pregnancy (Burch & Gallup Jr., 2004; Charles & Perreira, 2007; Clark, Hill, Jabbar, & Silverman, 2009; Martin et al., 2004; Mercedes & Lafaurie, 2015; Richardson et al., 2002), while other studies suggest that pregnancy may provide somewhat of a protective respite (Decker, Martin, & Moracco, 2004; Jasinski, 2001). Most of the studies have documented that the prevalence of IPV during pregnancy is consistently lower than IPV occurring before pregnancy, both in developed (Bacchus, Mezey, & Bewley, 2004; Charles & Perreira, 2007; Datner, Wiebe, Brensinger, & Nelson, 2007; Dunn & Oths, 2004; Heaman, 2005; Janssen et al., 2003; Renker & Tonkin, 2006; Saltzman, Johnson, Gilbert, & Goodwin, 2003; Yost, Bloom, McIntire, & Leveno, 2005), and developing nations (Díaz-Olavarrieta et al., 2007; Farid, Saleem, Karim, & Hatcher, 2008; Guo, Wu, Qu, & Yan, 2004a, 2004b; Nasir & Hyder, 2003; Perales et al., 2009; Thananowan & Heidrich, 2008). For example, a study among a national sample of Canadian women has found that 8.2% of women have experienced IPV before pregnancy, 3.3% during pregnancy and 2.2% after childbirth (Daoud et al., 2012). Similarly, Koenig et al. (2006) have reported that the prevalence of IPV is 8.9% during pregnancy and 4.9% in the postpartum period.
IPV around the time of pregnancy has been categorized into four different patterns in the literature: (1) Commencement of IPV (no IPV before pregnancy, but violence during pregnancy), (2) Continuation of IPV (IPV both before and during pregnancy), (3) Termination of IPV (IPV before pregnancy, but no IPV during pregnancy), and (4) No IPV either before or during pregnancy (Agrawal, Ickovics, Lewis, Magriples, & Kershaw, 2014; Ballard et al., 1998; Van Parys, Deschepper, Michielsen, Temmerman, & Verstraelen, 2014). Gazmararian et al. (1996) have proposed two patterns of IPV among pregnant women as: (1) Chronic, where pre-existing IPV may either increase or decrease in severity and chronicity during pregnancy, and (2) Acute, where IPV starts for the first time during pregnancy. In a longitudinal study with pregnant women to assess IPV during the late pregnancy and 6 months postpartum, Koenig et al. (2006) have proposed three patterns of IPV, as: (1) abating pattern (during pregnancy only), (2) repeating pattern (during and after pregnancy), and (3) emerging pattern (after delivery only).
Past history of IPV before pregnancy is one of the strongest predictors of experiencing IPV during pregnancy (Martin, Mackie, Kupper, Buescher, & Moracco, 2001). Studies have revealed that the commencement of IPV during pregnancy is the least common pattern of IPV against pregnant women, between 4% and 40% of women experience IPV for the first time during pregnancy (Taillieu & Brownridge, 2010). On the other hand, between 31% and 69% of pregnant women with a past history of IPV have reported that IPV has ceased during their pregnancies (Taillieu & Brownridge, 2010). Moreover, the WHO multi-country study has revealed that women who were victims of IPV before pregnancy, 13–50% of women were physically abused for the first time during pregnancy, and 8–34% of women reported that the extent of the abuse was more severe and frequent during pregnancy (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2005).
During pregnancy, there is a common pattern that the prevalence of psychological IPV is predominantly greater than the prevalence of physical IPV and sexual IPV, whereas the prevalence of sexual IPV is generally less than the prevalence of physical IPV (Castro, Peek-Asa, & Ruiz, 2003; Perales et al., 2009). Among three types of IPV, Physical IPV is relatively lower during pregnancy compared to other periods (Martin, Mackie, Kupper, Buescher, & Moracco, 2001; Scribano, Stevens, & Kaizar, 2013). However, in their longitudinal study, Macy et al. (2007) have revealed that women who have experienced physical IPV early in pregnancy always experience higher mean rates of each type of IPV during all of the time periods relative to women who do not report IPV at the beginning of their pregnancies.
The level of gender inequality within a society and cultural attitudes towards pregnancy may have an influence on IPV against pregnant women (Taillieu & Brownridge, 2010). In explaining why IPV is comparatively lower during pregnancy in comparison to before pregnancy, Van Parys et al. (2014) have reported three hypotheses: (a) pregnancy changes social status and increases social control and respect for the women; (b) a pregnant women is viewed as a receptacle for the vulnerable unborn baby, and use less physical and sexual IPV, and (c) during pregnancy, women themselves feel more vulnerable and in turn, use more strategies to avoid violent escalations. However, little is known about what factors contribute to the changing patterns, and why pregnancy appears to be a protective time for some women, while it is a period of increased risk for others (Macy, Martin, Kupper, Casanueva, & Guo, 2007; Silva, Ludermir, de Araujo, & Valongueiro, 2011; Taillieu & Brownridge, 2010; Van Parys, Deschepper, Michielsen, Temmerman, & Verstraelen, 2014).
2.4 Correlates of IPV during pregnancy
Correlates or factors associated with IPV during pregnancy are important to identify high-risk groups and illuminate intermediary factors in the causal pathway. Although there is no consensus as to the primary cause of IPV during pregnancy, several studies have attempted to identify some multiple social, economic, cultural, biological and environmental risk factors (Bohn, Tebben, & Campbell, 2004; Dunn & Oths, 2004; Hellmuth, Gordon, Stuart, & Moore, 2013; Karaoglu et al., 2005; Lipsky, Holt, Easterling, & Critchlow, 2005; McMahon & Armstrong, 2012; Saltzman, Johnson, Gilbert, & Goodwin, 2003). Factors that have been mentioned in different studies can be categorized into socio-demographic characteristics, obstetric and reproductive characteristics, and psycho-socio-cultural characteristics.
2.4.1 Socio-demographic characteristics
The socio-demographic correlates of age, maternal education, socio-economic status, area of residence and family status are illustrated in this section.
2.4.1.1 Age
A growing number of studies have shown that a relationship exists between young age and an increased risk of experiencing IPV during pregnancy (Datner, Wiebe, Brensinger, & Nelson, 2007; Farid, Saleem, Karim, & Hatcher, 2008; Heaman, 2005; Rådestad, Rubertsson, Ebeling, & Hildingsson, 2004; Thananowan, 2008; Thananowan & Heidrich, 2008; Valladares, Pena, Persson, & Hogberg, 2005). However, most of the studies use health facility-based samples rather than population-based samples and are limited in their generalizability (Brownridge et al., 2011; Jasinski, 2004). Some studies, on the other hand, have found no significant association between age and IPV victimisation during pregnancy IPV (Bacchus, Mezey, & Bewley, 2004; Fanslow, Silva, Whitehead, & Robinson, 2008). Few studies have documented that older age is also a risk factor for experiencing IPV during pregnancy (Hedin, 2000; Horrigan, Schroeder, & Schaffer, 2000). However, several studies have shown that increasing age is protective for physical and psychological IPV (Naved & Persson, 2008; Ruiz-Pérez et al., 2006; Thananowan & Heidrich, 2008; Varma, Chandra, Thomas, & Carey, 2007). Therefore, it is difficult to draw a general conclusion regarding the association between age and an increased risk of experiencing IPV during pregnancy.
2.4.1.2 Maternal Education
Research reveals contradictory findings in examining the association between women’s education and the risk of experiencing IPV during pregnancy. While some studies demonstrate that illiteracy or low education increases the risk of IPV during pregnancy (Audi, Segall-Correa, Santiago, Andrade, & Perez-Escamilla, 2008; Charles & Perreira, 2007; Datner, Wiebe, Brensinger, & Nelson, 2007; Farid, Saleem, Karim, & Hatcher, 2008; Fikree, Jafarey, Korejo, Afshan, & Durocher, 2006; Hammoury, Khawaja, Mahfoud, Afifi, & Madi, 2009; Heaman, 2005; Khosla, Dua, Devi, & Sud, 2005; Perales et al., 2009; Thananowan & Heidrich, 2008), several others reveal no significant difference (Campbell, Poland, Waller, & Ager, 1992; Chan et al., 2011; Díaz-Olavarrieta et al., 2007; Fanslow, Silva, Robinson, & Whitehead, 2008; Perales et al., 2009; Tiwari et al., 2008). A study has demonstrated that women with less than 12 years of education are nearly 5 times more likely to experience IPV during pregnancy than women with more than 12 years of education (Saltzman, Johnson, Gilbert, & Goodwin, 2003).
2.4.1.3 Socio-economic status (SES)
In the literature, the association between low income and the risk of IPV victimisation during pregnancy is inconsistent. Some studies have reported that women with low income are likely to be at a greater risk for experiencing IPV during pregnancy (Daoud et al., 2012; Díaz-Olavarrieta et al., 2007; Fanslow, Silva, Robinson, & Whitehead, 2008; Heaman, 2005; Perales et al., 2009; Ruiz-Pérez et al., 2006; Thananowan & Heidrich, 2008). In contrast, several studies find no significant difference in terms of household income between abused and non-abused pregnant women (Dunn & Oths, 2004; Farid, Saleem, Karim, & Hatcher, 2008; Lau, 2005; Leung, Leung, Lam, & Ho, 1999; Muthal-Rathore, Tripathi, & Arora, 2002). Quite surprisingly, while Varma et al. (2007) have shown that higher household income increases the risk of IPV victimisation during pregnancy; Fanslow et al. (2008) have reported that higher household income decreases the risk of experiencing IPV during pregnancy.
To assess the relationship between SES and the risk of IPV during pregnancy, these studies have directly used household income (Dunn & Oths, 2004; Sagrestano, Carroll, Rodriguez, & Nuwayhid, 2004) or proxy socioeconomic indicators [e.g. Medicaid or WIC participation (special supplemental food program for women, infants and children): a proxy measure of lower SES] (Gazmararian et al., 1995; Goodwin et al., 2000; Saltzman, Johnson, Gilbert, & Goodwin, 2003). For example, Saltzman et at. (2003) revealed that Medicaid recipients were 4.2 times more likely to be abused during pregnancy compared with non-Medicaid recipients. Pregnancy or the childbirth may intensify existing strains such as low socioeconomic status, which in turn may increase the stress level in the family and the risk of IPV (Jasinski, 2004).
2.4.1.4 Area of residence
There is no concrete evidence in the literature to get an idea regarding the association of area of residence (rural/urban) with the risk of IPV victimisation during pregnancy. Rural women may have more limited access to health care and social services than urban women, which may be a potential determinant of IPV victimisation during pregnancy (Brownridge et al., 2011). Some studies have found that the place of residence is not significantly associated with IPV, which may indicate that IPV is a serious social issue both in urban and rural areas (Daoud et al., 2012; Salari & Nakhaee, 2008).
2.4.1.5 Family status
While a few studies have found a positive relationship between living in an extended family and higher risk for experiencing violence during pregnancy (Mohammadhosseini, Sahraean, & Bahrami, 2010), at least one study has documented a negative relationship (Koenig, Ahmed, Hossain, & Mozumder, 2003).
In the culture of many traditional Asian societies, a newly married woman moves into her male partner’s household, which is generally an extended or joint family encompasses her husband’s parents and siblings. In these extended families, the mother-in-law commonly exercises power and control over household matters and the daughter-in-law is expected to carry out all her instructions and household chores (Gausia, Fisher, Ali, & Oosthuizen, 2009). During pregnancy, if the daughter-in-law fails to perform her household tasks because of her physical weakness or illness, in-laws often instigate violence. A study with Pakistani pregnant women reported that presence of in-laws is the most common reason for marital conflicts in the family (Fikree & Bhatti, 1999). A limited number of studies have shown a positive relationship between IPV victimisation and in-law-conflict or poor relationship with in-laws (Chan et al., 2011). Conversely, Naved and Persson (2008) have not found any association between spousal violence during pregnancy and living with one’s in-laws. Although the presence of in-laws in the household may create some conflict, at the same time they may prevent IPV as well (Naved & Persson, 2005).
2.4.2 Obstetric and reproductive characteristics
The obstetric and reproductive correlates of number of children/parity and pregnancy intention are discussed in this section.
2.4.2.1 Number of children/parity
Some studies have indicated that multiparous women are more likely to experience IPV during pregnancy than those pregnant with their first child (Farid, Saleem, Karim, & Hatcher, 2008; Heaman, 2005; Mohammadhosseini, Sahraean, & Bahrami, 2010; Muhajarine & D’Arcy, 1999; Ruiz-Pérez et al., 2006; Salari & Nakhaee, 2008; Tiwari et al., 2008). Farid et al. (2008) have shown an independent association between the number of living children and physical and/or emotional IPV victimisation among Pakistani pregnant women, with each additional child increases the risk of IPV victimisation by 34%. A study from Iran has shown that multiparous women are up to 7 times more likely to experience IPV during pregnancy than primiparous women (Salari & Nakhaee, 2008). The reason behind these outcomes may be that many children intensify the existing socioeconomic stress of the family. In contrast, a range of studies has found no significant difference between parity and the likelihood of experiencing IPV during pregnancy (Charles & Perreira, 2007; Díaz-Olavarrieta et al., 2007; Dunn & Oths, 2004; Srinivasan & Bedi, 2007).
2.4.2.2 Pregnancy intention
Previous studies have revealed an association between pregnancy intention and the increased risk for IPV victimisation during pregnancy. A growing number of studies have found that unintended or unplanned pregnancy is significantly correlated with higher risk for experiencing IPV during pregnancy (Charles & Perreira, 2007; Cripe et al., 2008; Fanslow, Silva, Whitehead, & Robinson, 2008; James, Brody, & Hamilton, 2013; Mercedes & Lafaurie, 2015; Okenwa, Lawoko, & Jansson, 2011; Pallitto et al., 2013; Perales et al., 2009; Raihana, Shaheen, & Rahman, 2012; Salari & Nakhaee, 2008; Tiwari et al., 2008). A few studies, on the other hand, find no significant association between unintended pregnancy and the risk for IPV victimisation during pregnancy (Martin & Garcia, 2011).
Salari & Nakhaee (2008) has shown that unintended pregnancy in Iran is the most significant associated factor for IPV victimisation during pregnancy, carrying an adjusted odds ratio of 7.7. Goodwin et al. (2000) have indicated that women with unintended pregnancies in the United States are approximately 2.5 times more likely to have been physically abused than women with intended pregnancies. Couples expecting an unplanned or unwanted child may be facing a greater level of stress compared to those couples who have children that were planned, consequently elevate the risk for IPV victimisation (Jasinski, 2004). Moreover, a pregnancy not planned by the male partner might mean something that he could not control and therefore increases the risk for IPV against his spouse (Jasinski, 2004).
2.4.3 Psycho-socio-cultural characteristics
The psycho-socio-cultural correlates of traditional gender roles acceptance, husband’s controlling behaviours, women’s decision-making autonomy, dowry demands at marriage, low level of social support, low self-esteem, husband’s substance abuse and childhood exposure to violence are examined in this section.
2.4.3.1 Traditional gender roles acceptance
Cross-cultural research of IPV suggests that it widely occurs in male-dominant, patriarchal social structures where societies support higher levels of inequality between male and female, and where highly conservative attitudes towards traditional gender roles may lead to endorsement and acceptance of IPV (Fulu et al., 2013; Jewkes, 2002; Okenwa, Lawoko, & Jansson, 2009). Traditional gender constructions limit women’s responsibilities to maintain exclusively the household through housework, childbearing and child caring. In contrast, the social acceptability of male domination reinforces the belief that men should be the breadwinner with the prime decision-making authority as the head of the family. Feminist theorists consider traditional gender roles to be the principal breeding ground for IPV in patriarchal societies because it gives superiority to male over female (Clark, Hill, Jabbar, & Silverman, 2009; Flood & Pease, 2009; Stark, 2007; Walker, 2009). Notably, gender roles attitudes act as socio-cultural tools for the intimidation and control of women (Islam, Broidy, Baird, & Mazerolle, 2017).
Studies from countries with traditional gender constructions indicate that physical violence is seen to be normatively acceptable when a wife is perceived to be disobedient, and when she fails to conform to certain traditional gender role expectations (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; Hadi, 2005; Healey, Smith, & O’Sullivan, 1998; Sugarman & Frankel, 1996). Furthermore, evidence suggests that societal norms, such as male dominance and female subjugation and subordination become internalized and integrated into the culture so much so that women themselves support a man’s right to beat his wife under certain circumstances (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; Jewkes, 2002; Uthman, Moradi, & Lawoko, 2009). Existing literature also reveals a positive relationship between traditional gender roles attitudes and tolerant views of IPV (Dobash & Dobash, 1979; Haj-Yahia, 1998; Straus, Gelles, & Steinmetz, 1980; Sugarman & Frankel, 1996; Willis, Hallinan, & Melby, 1996).
Women’s conservative attitude towards traditional gender roles is rarely evaluated as a determinant for IPV during pregnancy (Clark, Hill, Jabbar, & Silverman, 2009). A few studies demonstrated that traditional attitudes towards gender roles, such as the belief that men should be the head of the family and women should be the homemakers, or that women should be always emotionally and physically available to men, are correlated with victimisation and perpetration of IPV during pregnancy (Bacchus, Mezey, & Bewley, 2006; Brownridge et al., 2011; Burch & Gallup Jr., 2004; Pallitto, Campbell, & O’campo, 2005). During pregnancy, women may be unable to perform their traditional roles as homemaker/caretaker due to reduced mobility, increased tiredness and a lack of emotional availability, which may induce increased IPV by abusers who tend to hold more conventional sex role attitudes (Taillieu & Brownridge, 2010).
2.4.3.2 Husband’s controlling behaviours
There is a dearth of research on the impact of husband’s controlling behaviours on the risk of IPV during pregnancy (Taillieu & Brownridge, 2010). Limited evidence suggests that male partners may be more prone to abusive behaviour in the presence of jealousy or suspicion of infidelity, especially during pregnancy (Goetz, Shackelford, Romero, Kaighobadi, & Miner, 2008; Harris, 2003; Hellmuth, Gordon, Stuart, & Moore, 2013). Men want to control female sexuality and to prevent predicted infidelity (Buss & Shackelford, 1997; Cousins & Gangestad, 2007; Pallitto & O’Campo, 2005), and use violence as a controlling strategy (Buss & Duntley, 2011). Notably, paternal uncertainty and accusations of infidelity have been linked to an increased risk for experiencing IPV among pregnant women (Bacchus, Mezey, & Bewley, 2006; Burch & Gallup Jr., 2004; Chambliss, 2008; Pallitto & O’Campo, 2005). Burch and Gallup (2004) suggest that the male constantly monitors his partner or isolates her from other men so as to be sure that the child she bears is his own. Therefore, men may develop paternal assurance tactics, such as the use of IPV to establish control, to combat paternal uncertainty and to make sure that the children he raises are his own (Brownridge et al., 2011).
In a study from the U.S, 43% of women experiencing IPV during pregnancy have reported that their partner regulated all their activities in the year prior to pregnancy onset (Decker, Martin, & Moracco, 2004). Moreover, financial control by restricting access to money has been reported by women who have experienced IPV during pregnancy (Bacchus, Mezey, & Bewley, 2006; Pulido, 2001). Sexual jealousy and possessiveness, financial control and social isolation from family and friends are some of the male partner’s controlling behaviours that are inflicted upon the pregnant women (Brownridge et al., 2011).
2.4.3.3 Women’s decision-making autonomy
Cross-cultural research of IPV demonstrates that women whose husbands have the final authority in household decisions are more likely to experience physical, sexual and psychological IPV (Morash, Bui, Zhang, & Holtfreter, 2007; Rani & Bonu, 2009; Uthman, Moradi, & Lawoko, 2009; Zhu & Dalal, 2010). All forms of IPV were found to be least common among couples when they hold joint autonomy in household decisions, and when women had decision-making power on spending her own earnings (Uthman, Moradi, & Lawoko, 2009; Zhu & Dalal, 2010). It is undebated that abused women commonly have less decision-making power, limited freedom of movement and higher financial dependency on their male partners (Ellsberg, Peña, Herrera, Liljestrand, & Winkvist, 2000; Smith & Martin, 1995). Women’s low decision-making autonomy is an important component of the feminist theory that reflects a power and control motive.
2.4.3.4 Dowry demands at marriage
A number of studies have found that payment of dowry (the bride’s family commits to provide large sums of money, jewellery, and other goods to the groom or groom’s family at marriage) is associated with IPV in some developing countries, especially in South Asian countries (Hasan, Muhaddes, Camellia, Selim, & Rashid, 2014; Naved, Azim, Bhuiya, & Persson, 2006; Naved & Persson, 2008; Peedicayil et al., 2004). There is a common tendency in those societies to consider dowry as groom price (Taher, Islam, Chowdhury, & Siddiqua, 2014) that may be an indicator of patriarchal attitude (Naved & Persson, 2010). Dissatisfaction with non-payment or inadequate dowry payment usually leads to conflict between the couple after marriage, and substantially contributes to IPV[2], though giving and taking dowry is legally prohibited (Babu & Kar, 2010; Barnett, Miller-Perrin, & Perrin, 2005; Naved & Persson, 2010; Odhikar, 2014; Taher, Islam, Chowdhury, & Siddiqua, 2014). Brides families offer dowry for their daughters, especially when daughters are not beautiful by conventional and cultural norms (Hasan, Muhaddes, Camellia, Selim, & Rashid, 2014). Thus, dowry completely demolishes the dignity of women, and makes them very vulnerable to IPV (Taher, Islam, Chowdhury, & Siddiqua, 2014). Marriage involved dowry demands are positively associated with IPV during pregnancy in rural areas of Bangladesh (Naved & Persson, 2008) and India (Peedicayil et al., 2004).
2.4.3.5 Low level of social support
A lack of social support from friends, family and significant others have been linked with an increased risk of IPV victimisation during pregnancy (Farid, Saleem, Karim, & Hatcher, 2008; Jeanjot, Barlow, & Rozenberg, 2008; Peedicayil et al., 2004; Ruiz-Pérez et al., 2006; Valladares, Pena, Persson, & Hogberg, 2005). Past studies have revealed that abused pregnant women report being socially isolated from family, friends and other social support networks by their male partners due to jealousy of other close relationships (Bacchus, Mezey, & Bewley, 2006; Noel & Yam, 1992; Pulido, 2001; Wiemann, Agurcia, Berenson, Volk, & Rickert, 2000). Besides, abused pregnant women have reported both lower level of social support from others and from their male partners compared to non-abused pregnant women (Heaman, 2005). It may be due to that a male partner’s attempt to socially isolate his female partner may decrease her social support networks, and in turn, increase the dependence on the male partner (Taillieu & Brownridge, 2010). Conversely, other research has not found significant differences in the social support networks of abused and non-abused pregnant women (Chan et al., 2011; Charles & Perreira, 2007; Dunn & Oths, 2004).
2.4.3.6 Low self-esteem
Previous studies have documented an association between low self-esteem and the increased risk for experiencing IPV during pregnancy (Loft Abadi, Ghazinour, Nojomi, & Richter, 2012). In abusive relationships, the abused women were found to have a lower self-esteem and were more likely to report physical, sexual and psychological aggression compared to women with higher self-esteem (Salari & Baldwin, 2002). A woman’s lowered sense of self-esteem creates a feeling of guilt, shame, unworthiness, helplessness, powerlessness and a negative perception of the self that ultimately increase her frustration, depression, motivational impairment of problem-solving ability and isolation from others (Bell & Mattis, 2000; Deyessa et al., 2009; Mechanic, Weaver, & Resick, 2008). As a consequence, she may no longer enjoy her intercommunication with her husband and significant others (Stewart, 2007), suggesting that a lowered sense of self-esteem makes women unworthy of being loved by others which in turn increases a woman’s risk of IPV victimisation (Bell & Mattis, 2000). Moreover, the feeling of unworthiness and powerlessness generates fear of being alone within abused women, which in turn prevents women from leaving the abusive relationship (Bell & Mattis, 2000).
2.4.3.7 Husband’s substance abuse
IPV during pregnancy is associated with the use of tobacco, alcohol, and/or illicit drugs. Although a number of studies have found a strong relationship between pregnant women’s substance abuse and the increased risk for IPV victimisation (Bailey & Daugherty, 2007; Certain, Mueller, Jagodzinski, & Fleming, 2008; Charles & Perreira, 2007; Datner, Wiebe, Brensinger, & Nelson, 2007; Lipsky, Holt, Easterling, & Critchlow, 2005), few studies so far have documented the relationship between the husband’s substance abuse and the risk of perpetrating IPV against a woman during pregnancy (Bacchus, Mezey, & Bewley, 2006; Díaz-Olavarrieta et al., 2007; McFarlane, Parker, & Soeken, 1995; Muhajarine & D’Arcy, 1999; Wiemann, Agurcia, Berenson, Volk, & Rickert, 2000). Other than alcohol use, male partners’ illicit drug abuse also significantly increases the odds of IPV against a pregnant partner (Amaro, Fried, Cabral, & Zuckerman, 1990; Charles & Perreira, 2007).
2.4.3.8 Childhood exposure to violence
Previous history of violence in the families of origin of either partner has an impact on degrees of adult perpetration and victimization because it is often transmitted across generations through the socialisation process (Brownridge et al., 2011; Flood & Pease, 2009; Zhu & Dalal, 2010). However, it has not been fully explored whether childhood exposure to violence is associated with the risk of IPV during pregnancy. Very few studies have demonstrated that women who witnessed or experienced violence during their childhood are more likely to experience IPV during pregnancy (Castro, Peek-Asa, & Ruiz, 2003; Clark, Hill, Jabbar, & Silverman, 2009; Farid, Saleem, Karim, & Hatcher, 2008; Guo, Wu, Qu, & Yan, 2004a; Naved & Persson, 2008). Naved and Persson (2008) found that spousal abuse of a woman’s mother or mother-in-law is one of the strongest predictors of her risk for experiencing IPV during pregnancy by her husband.
2.5 Consequences of IPV during pregnancy
Studies from the developed and developing countries have generated increasing evidence that IPV during pregnancy is a serious public health concern with consequences for the health and well-being of the mother, the developing fetus and the baby during pregnancy, at birth and during the postpartum period (Brown, McDonald, & Krastev, 2008; Han & Stewart, 2014; Howard, Oram, Galley, Trevillion, & Feder, 2013; Jasinski, 2004; Kendall-Tackett, 2007; Trabold, Waldrop, Nochajski, & Cerulli, 2013; Van Parys, Verhamme, Temmerman, & Verstraelen, 2014). These devastating effects generally have long lasting consequences on the emotional well-being of victims and may prevail well after the IPV has ended (Campbell, 2002; Trabold, Waldrop, Nochajski, & Cerulli, 2013). Some of the negative consequences of IPV during pregnancy for women and their children are presented in this section.
2.5.1 Injuries and physical health outcomes
Victims of IPV usually report negative physical health effects such as chronic health conditions, poor quality of life and increased use of health care services (Campbell, 2002). The mean medical cost per incident of physical assault in the US is US$548 which may rise to US$2,665 if all medical services are sought (National Center for Injury Prevention and Control, 2003). IPV is one of the leading causes of injury in women (Campbell, 2002). Women experiencing IPV during pregnancy report being kicked, punched, threatened with knives, choked, scalded and having objects thrown at them (Bacchus, Mezey, & Bewley, 2006). Along with a number of IPV-related injuries, including cuts, bruises to the face, neck, chest and abdomen, fractures, concussions, dental injuries, stab wounds, pneumothorax, performed eardrums, women also report to have vaginal bleeding and persistent headaches as a result of the IPV they experience (Bacchus, Mezey, & Bewley, 2006; Rachana, Suraiya, Hisham, Abdulaziz, & Hai, 2002; Sharps, Laughon, & Giangrande, 2007). Studies have reported that IPV during pregnancy is a risk factor for antepartum hospitalization (Kaye, Mirembe, Bantebya, Johansson, & Ekstrom, 2006), and 10% of hospitalizations during this period are the result of intentional injuries due to IPV against the pregnant woman (Chambliss, 2008).
Other adverse outcomes include general poor health, high blood pressure, diabetes, asthma, cardiovascular problem, gastrointestinal, frequent kidney infections and urinary tract infection (Dillon, Hussain, Loxton, & Rahman, 2013; Rachana, Suraiya, Hisham, Abdulaziz, & Hai, 2002). Sexual IPV can lead to an increased risk of sexually transmitted diseases, pelvic inflammatory disease, sexual dysfunction, bladder infections and other gynaecological health problems (Campbell & Lewandowski, 1997). Women who are victims of sexual IPV with or without physical IPV are more likely to report gynaecological health problems than women who experience physical IPV only, or those who have never abused (Stenson, 2004; Stephenson, Koenig, & Ahmed, 2006). Studies also have reported that self-perceived poor health status is significantly associated with IPV (Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, 2008; Ishida, Stupp, Melian, Serbanescu, & Goodwin, 2010; Nur, 2012; Yoshihama, Horrocks, & Kamano, 2009).
2.5.2 Mental health outcomes
A growing number of studies have demonstrated that IPV during and after pregnancy is associated with maternal mental health complexities such as anxiety disorders, depression, posttraumatic stress disorder, low self-esteem, negative self-image, less life satisfaction, functional impairment and fear of intimacy (Bacchus, Mezey, & Bewley, 2006; Chambliss, 2008; Escribà-Agüir, Ruiz-Pérez, & Saurel-Cubizolles, 2007; Jeanjot, Barlow, & Rozenberg, 2008; Martin, Li, Casanueva, Britt, & Kupper, 2006; Murphy & Ouimet, 2008; Pallitto, Campbell, & O’campo, 2005; Romito, Pomicino, Lucchetta, Scrimin, & Molzan Turan, 2009; Zlotnick, Johnson, & Kohn, 2006). These mental health problems often co-occur (Ogbonnaya, Kupper, Martin, Macy, & Bledsoe-Mansori, 2013). Martin and colleagues (2006) have revealed that women who have experienced multiple forms of IPV (physical, sexual and/or psychological) before or during pregnancy are at a greater risk for psychological distress and depression compared to non-victims. It is estimated that the cost for women who seek mental health care after being abused is US$269 per incident of IPV in the US, while the cost rises to US$1017 if victims seek a full set of mental health care visits (National Center for Injury Prevention and Control, 2003).
Other related complications of IPV during pregnancy are prenatal substance use or abuse including tobacco, alcohol, prescription drugs and illicit drugs (Datner, Wiebe, Brensinger, & Nelson, 2007; Heaman, 2005; Lipsky, Holt, Easterling, & Critchlow, 2005; Pallitto, Campbell, & O’campo, 2005; Sarkar, 2008), and suicide (Karmaliani et al., 2008; Naved & Akhtar, 2008; Shadigian & Bauer, 2004). Women who have experienced IPV, and have attempted suicide reports higher levels of sadness, self-dislike, feeling of worthlessness and suicidal thoughts (Houry, Kaslow, & Thompson, 2005). A number of women who are abused during pregnancy hold themselves responsible for their partner’s abusive behaviour (Bacchus, Mezey, & Bewley, 2006), and as a consequence report perceived stress (Valladares, Ellsberg, Peña, Högberg, & Persson, 2002). The WHO multi-country study on women’s health and domestic violence against women reports that memory loss, problems with concentration and dizziness are significantly associated with lifetime experiences of IPV across all the study sites (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2005).
Considering the severity and frequency, the more severe and/or the more frequent the experience of IPV, the more severe the symptomatology of mental health complications appears to be, suggesting a dose-response association between IPV victimisation and depression, anxiety and suicidal ideation (Dillon, Hussain, Loxton, & Rahman, 2013). These mental health complexities not only affect the quality of life for the new mothers but also their daily functioning in the postpartum period (Martin, Li, Casanueva, Britt, & Kupper, 2006; Rådestad, Rubertsson, Ebeling, & Hildingsson, 2004).
2.5.3 Pregnancy outcomes
IPV beforeor during pregnancy may affect pregnancy outcomes through direct and indirect mechanisms (Koski, Stephenson, & Koenig, 2011; Shah & Shah, 2010).The most studied pregnancy outcome due to IPV is low birth weight (LBW) of babies (Kaye, Mirembe, Bantebya, Johansson, & Ekstrom, 2006; Murphy, Schei, Myhr, & Du Mont, 2001; Saltzman, Johnson, Gilbert, & Goodwin, 2003; Sarkar, 2008; Shah & Shah, 2010). A meta-analysis of studies across the USA and Canada demonstrated that women who report experiencing IPV during pregnancy are 40% more likely to give birth to an LBW baby (Murphy, Schei, Myhr, & Du Mont, 2001).It has been suggested that there is a relationship between IPV and stress. An increase in stress is thought to lead to increased levels of cortisol, which has been linked to LBW babies (Valladares, Peña, Ellsberg, Persson, & Högberg, 2009). LBW is one of the most significant risk factors of infant ill-health and mortality during the first year of life.
IPV is also significantly linked to other adverse pregnancy outcomes such as unwanted pregnancy, low prenatal weight gain (McFarlane, Campbell, Sharps, & Watson, 2002; Shadigian & Bauer, 2004), preterm delivery (Rachana, Suraiya, Hisham, Abdulaziz, & Hai, 2002; Sarkar, 2008; Shah & Shah, 2010), miscarriage/abortion (Jewkes, Penn-Kekana, Levin, Ratsaka, & Schrieber, 2001; Silverman, Gupta, Decker, Kapur, & Raj, 2007), placental abruption, fetal injury and perinatal death (Janssen et al., 2003; Sarkar, 2008; Shadigian & Bauer, 2004; Van Parys, Verhamme, Temmerman, & Verstraelen, 2014). Sexual IPV can cause vaginal infection which in turn increases the risk of preterm rupture of membranes and preterm delivery (Moodley & Sturm, 2000).
2.5.4 Maternal health service utilization
Although service accessibility (Rahman, Mosley, Ahmed, & Akhter, 2008)demographic (Chakraborty, Islam, Chowdhury, & Bari, 2002; Chakraborty, Islam, Chowdhury, Bari, & Akhter, 2003; Rai, Singh, Singh, & Kumar, 2014) and socio-economic factors (Amin, Shah, & Becker, 2010; Navaneetham & Dharmalingam, 2002; Paul & Rumsey, 2002; Rahman, Mosley, Ahmed, & Akhter, 2008; Rai, Singh, Singh, & Kumar, 2014) are notable in affecting when, where and how often women receive maternal health care services; research has begun to investigate the influence of other psychosocial risk factors. Scholars have proposed that IPV might introduce unique risks that negatively affect women’s reproductive behaviour and utilization of health care services such as prenatal care (Bailey & Daugherty, 2007; Moraes, Arana, & Reichenheim, 2010; Taillieu & Brownridge, 2010). Several studies have revealed that women who experience IPV during pregnancy are more likely to receive inadequate prenatal care (Heaman, 2005; Lipsky, Holt, Easterling, & Critchlow, 2005) and entry into prenatal care late (Bailey & Daugherty, 2007; Goodwin et al., 2000; Huth-Bocks, Levendosky, & Bogat, 2002; Jasinski, 2004; McCloskey et al., 2007; McFarlane, Campbell, Sharps, & Watson, 2002; Sharps, Laughon, & Giangrande, 2007) compared to non-abused women.
Survivors of IPV are also reported to have a lack of family support, restricted access to health services, strained relationship with health care providers and employers, and isolation from social networks (Heise & Garcia-Moreno, 2002). Additionally, IPV can compromise women’s health seeking behaviour due to the associated mental and emotional health impairments such as trauma, chronic pain, stress, depression, anxiety, dizziness, functional disorders and other mental health problems (Coker, Smith, Bethea, King, & McKeown, 2000; Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, 2008), which may limit women’s energy to take appropriate health care measures. Delayed entry in seeking maternal health care services may be due to either controlling behaviour by the perpetrator (Dietz et al., 1997; Koski, Stephenson, & Koenig, 2011; Taggart & Mattson, 1996) or fear of exposing obvious signs of physical violence, such as black eyes or bruises (Taggart & Mattson, 1996).
2.5.5 Maternal-child bonding
IPV may have adverse effects on women’s mental health during pregnancy and after delivery (Bacchus, Mezey, & Bewley, 2004; Bonomi et al., 2006; Romito, Molzan Turan, & De Marchi, 2005). Studies have demonstrated associations between maternal depression and disturbances in mother-child interactions (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Depressed mothers are more likely to express behaviours that have a long-term emotional, cognitive, intellectual and developmental problem in children (Cooper & Murray, 1998; Hart, Field, & Nearing, 1998; Murray, Fiori‐Cowley, Hooper, & Cooper, 1996; Wachs, Black, & Engle, 2009; Weinberg & Tronick, 1998). Furthermore, IPV during pregnancy significantly affects maternal-child bonding, fetal brain development and breastfeeding practices (Janssen et al., 2003; Jasinski, 2004; Sarkar, 2008; Sharps, Laughon, & Giangrande, 2007; Trabold, Waldrop, Nochajski, & Cerulli, 2013). A mother experienced IPV will likely to expend most of her time and energy coping with ongoing violence, rather than focus on bonding and caring for her baby. Additionally, a depressed mother may be tired, unable to concentrate and preoccupied with feelings of guilt, worthlessness and hopelessness, and consequently, may no longer enjoy her interaction with her child (Stewart, 2007).
2.5.6 Homicide
Homicide is the most extreme consequence of IPV (WHO, 2011). Researchers have reported that pregnant women are at an increased risk for lethal IPV or homicide (Burch & Gallup Jr., 2004; Chang, Berg, Saltzman, & Herndon, 2005; Decker, Martin, & Moracco, 2004; Horon & Cheng, 2005; Martin et al., 2004; McFarlane, Campbell, Sharps, & Watson, 2002; Shadigian & Bauer, 2004). McFarlane et al. (2002) have documented that women who experience IPV during pregnancy have three times higher odds of attempted or completed homicide. Studies have reported that homicide is the leading cause of all types of death during pregnancy and the first year postpartum in the U.S. (Chang, Berg, Saltzman, & Herndon, 2005; Cheng & Horon, 2010). IPV-related homicide is the leading cause of maternal mortality, accounting for 13% to 24% of all deaths among pregnant women (Plichta, 2004). Homicide during pregnancy kills the fetus as well, and during postpartum, leaves the infant to live without his/her biological mother.
From the above discussion, it is apparent that IPV before, during and after pregnancy has grave consequences for mothers, children and families.
2.6 Chapter summary
From the aforementioned discussion, it is apparent that a significant number of pregnant women experience intimate partner violence during pregnancy. Research on the prevalence of different forms of IPV women experience over the course of the reproductive lifespan is needed to better understand the important patterns of IPV during pregnancy. Moreover, an understanding of the potential correlates and consequences of IPV during pregnancy is crucial in order reduce or prevent the social problem in an effective manner. The chapter clearly described the prevalence, changing patterns, potential correlates and consequences of IPV during pregnancy. In the next chapter, three theoretical perspectives (feminist theory, social learning theory and evolutionary psychology theory) that can explain IPV during pregnancy are examined.
Theories explaining intimate partner violence during pregnancy |
Theoretical frameworks of crime are of crucial importance for communicating main ideas and its causes, sharing knowledge and informing interventions intended to prevent, reduce or eliminate the social problem (Dixon & Graham-Kevan, 2011; Mazerolle, 2007). There are various theoretical explanations of IPV and a range of policy, prevention and intervention protocols have so far been developed targeting the theoretical mechanisms (Bell & Naugle, 2008; Dixon & Graham-Kevan, 2011). No single theory can be able to explain IPV properly, even little consensus has yet been reached on the etiology of IPV (Heise, 1998). Theories of IPV have yet been strongly influenced by either the disciplinary biases of anthropology, biology, psychology, sociology, and criminology or the ideological and political agendas of feminist activists (Heise, 1998; Lawson, 2012). However, there is widespread agreement that IPV is not simply an individual problem; rather it is a social problem (Miller, 1994; Portwood & Heany, 2007). Macro-level theories focus on historical, sociological and cultural contexts that explain variation in rates of IPV while micro-level theories focus on perpetrators and victims as well as their interactions within these contexts to account for individual-level involvement on IPV. However, in order to understand the complex phenomenon of IPV these theories provide a framework for research and practice (O’Neill, 1998).
This chapter provides theoretical explanations for IPV during pregnancy. In the first instance, contextual reasons for IPV during pregnancy are depicted, followed by theoretical perspectives of IPV during pregnancy. Finally, relying on the theories, a conceptual framework for the influence of IPV during pregnancy on delayed entry into prenatal care, postpartum depression and mother’s exclusive breastfeeding has been developed at the end of this chapter.
3.1 Contextual reasons for IPV during pregnancy
Limited scholarship examines the situational context in which IPV during pregnancy occurs. Thus, we know little about the contextual correlates of IPV during pregnancy. Gelles (1975) has proposed five major situations of causation of IPV during pregnancy, as: (1) male sexual frustration, (2) the stress of imminent parenthood, (3) biochemical changes in the wife, (4) a conscious or subconscious desire to terminate the pregnancy, (5) the women’s increased physical vulnerability and helplessness. However, Gelles’s work has been strongly criticised for its victim-blaming approach and for minimizing the role of male partner for the violence (Campbell, Oliver, & Bullock, 1993).
Another qualitative study by Campbell and colleagues (1993) involving 97 abused women has documented four basic themes of being abused during pregnancy: (1) jealousy of the unborn child (18.5%, n=5), (2) anger towards the unborn child (14.8%, n=4), (3) anger towards the mother or ‘business as usual’ (46%, n=11), and (4) pregnancy-specific violence that was not directed toward the unborn child (14.8%, n=4). Moreover, pregnancy can symbolise a woman’s independence from her male partner, and change the family dynamics and the balance of power between the woman and her partner (Bacchus, Bewley, & Mezey, 2001). Bacchus et al. (2001) also argue that during and immediately after pregnancy, mothers receive more attention from family, friends and health professionals thus creating the potential for IPV to be exposed. Additionally, it has been suggested that the woman who becomes preoccupied with the impending birth, is less physically able to meet her partner’s needs. The abusive partner treats it as a threat to his position of power and may use IPV against the pregnant women in an attempt to regain control over her (Bacchus, Bewley, & Mezey, 2001).
Some researchers have suggested that pregnancy constitutes a particularly critical period of experiencing IPV because of changes in women’s physical, social, emotional, and economic needs during pregnancy, increased economic pressure, and less frequent sexual relations (Brownridge et al., 2011; Jeanjot, Barlow, & Rozenberg, 2008; Saltzman, Johnson, Gilbert, & Goodwin, 2003). For finding out the correlates of IPV during pregnancy, other studies have taken into consideration the psychological status of the perpetrator, such as increased stress over having to support an infant, anger over an unplanned pregnancy and jealousy that the female partner’s attention may have shifted to the baby (Brewer & Paulsen, 1999). Unintended pregnancies may further intensify IPV risks since these can introduce considerable financial stress (Kashif, Murtaza, & Kirkman, 2010). The pregnancy may also induce suspicion of infidelity in abusive males (Daly, Wilson, & Weghorst, 1982; Mezey & Bewley, 1997) which indicates that perpetrators are sexually jealous, and in some cases, they try to deny paternity (Parker & McFarlane, 1991). Besides, IPV during pregnancy may occur due to the jealousy and resentment towards the unborn child and the perception that the pregnancy would interfere with the woman’s role as a caretaker for her partner (Campbell, Oliver, & Bullock, 1993; Mezey & Bewley, 1997). Some researchers have suggested that IPV during pregnancy is not related to pregnancy, but actually a continuation of the ongoing violence (Campbell, Oliver, & Bullock, 1993; Taillieu & Brownridge, 2010).
3.2 Theoretical perspectives of IPV during pregnancy
Research on IPV during pregnancy has remained comparatively atheoretical (Taillieu & Brownridge, 2010), although a few theoretical perspectives have been used to frame IPV during pregnancy. A sociological perspective emphasizes life events stress, unemployment, poverty, male peer support, poor conflict management skills, substance abuse, the intergenerational transmission of violent behaviour, familial and societal patriarchy and power imbalances in the male-female relationship as factors contributing to IPV (DeKeseredy & Schwartz, 2011; Noel & Yam, 1992). A psychopathology perspective, on the other hand, suggests that men who are violent against their spouses have some sort of personality disorder or psychiatric problem (Jasinski & Kantor, 2001; Noel & Yam, 1992). More specifically, IPV theories span several levels of analysis, ranging from the influence of societal norms and power inequalities to the interactions between family members in childhood and adulthood, and finally to individual characteristics that increase the likelihood of IPV perpetration (Woodin & O’Leary, 2009). Therefore, it has been suggested that a multilevel theoretical formulation may explain IPV and the persistence of abusive relationships more comprehensively (Chornesky, 2000).
It is beyond the scope of this study to outline all theories. Therefore, the study will focus mainly on the most widely used and empirically validated theories pertaining to IPV. The most prominent theories used in the literature to explain IPV include the WHO ecological model, the social learning theory, gender and masculinity, feminist theories and the inter-generational transmission theory (Ellsberg & Heise, 2005; Johnson, Ollus, & Nevala, 2007). However, this section will focus on three different approaches: feminist theory, social learning theory and evolutionary psychology theory. Very few studies have explored these theories in relation to the occurrence of IPV during pregnancy. However, focusing on these theories can help to hypothesize the connection between pregnancy and IPV victimisation. Using these theories, I aim to develop a conceptual model to frame the study of IPV during pregnancy and its impacts on maternal and child health.
3.2.1 Feminist Theory
By examining the sociocultural context, feminist theories focus on how broader social forces such as patriarchy contribute to violence against women (Barrett, 1980; Bell & Naugle, 2008; DeKeseredy & Schwartz, 2011; Woodin & O’Leary, 2009). Anthropological research reveals that patriarchy i.e. men’s structural control over political, legal, economic and religious institutions is almost universal in all societies, across time and space (Glick & Fiske, 1997; McHugh & Frieze, 1997). Patriarchy is thought to consist of two basic components: (1) a structure, in which males possess superior power and economic privilege than women and (2) an ideology that legitimizes this arrangement (Dobash & Dobash, 1979; Smith, 1990). It can be also differentiated as social patriarchy which refers to male dominance in society as a whole, and familial patriarchy which refers to male dominance in the family (Barrett, 1980). Most importantly, gender roles defined by society and taught to individuals during childhood are thought to place men in positions of power over women as a whole (Mihalic & Elliott, 1997).
This theory holds the view that power and control are used as a tool in maintaining male dominance directly or indirectly over women within a patriarchal social system (Babu & Kar, 2010; Dobash & Dobash, 1979; Healey, Smith, & O’Sullivan, 1998; Herzog, 2007; Renzetti, 2004). In a patriarchal system, male voices and experiences have been privileged historically over female voices and experiences (Renzetti, 2004). That’s why men feel that they should be in charge of the family: making decisions, laying down rules, disciplining disobedient partners and children, and correcting unsatisfactory performance of duties (Healey, Smith, & O’Sullivan, 1998). The theory also posits that the social acceptability of male domination embody the belief that males have the right to use physical force against their intimate female partners as a social instrument of intimidation to control them, consequently to sustain unequal power in intimate relationships (Dobash & Dobash, 1979; Herzog, 2007; Smith, 1990; Straus, Gelles, & Steinmetz, 1980; Yllo & Straus, 1990). Therefore, IPV is viewed largely a function of prevailing societal and cultural norms and attitudes that not only condone but also legitimate violent acts (Ashrafun & Säävälä, 2014; Dobash & Dobash, 1979; Fonagy, 1999; Haj-Yahia, 1998; Straus, Gelles, & Steinmetz, 1980; Sugarman & Frankel, 1996).
Evidence suggests that IPV commonly occurs in societies and in families where high levels of gender inequality exist, women are less empowered and male partners have more power and control (Ackerson & Subramanian, 2008; Ashrafun & Säävälä, 2014; Schuler, Bates, & Islam, 2008; Yllo, 2005). These elements reinforce male dominance and female subjugation and subordination. Most feminist explanations of the persistence of IPV focus on the subjugation and subordination of women as the principal breeding ground for violence against women (Dobash & Dobash, 1979; Stark, 2007; Walker, 2009). Some theoretical and empirical studies on the relationship between patriarchy and IPV show that men tend to physically beat their wives when they disobey or are perceived as disobeying husband’s authority (Dobash & Dobash, 1979; Sugarman & Frankel, 1996). Research has revealed that there is a positive relationship between traditional gender-role attitudes and tolerant perceptions of IPV (Dobash & Dobash, 1979; Haj-Yahia, 1998; Straus, Gelles, & Steinmetz, 1980; Sugarman & Frankel, 1996; Willis, Hallinan, & Melby, 1996).
In many low- and middle-income countries, including Bangladesh, the traditional patriarchal normative structure puts women subordinate to men in all realms of life and supports men’s use of force against women when necessary (Cain, Khanam, & Nahar, 1979; Hadi, 2005; Mollah, 2005). In a patriarchal social system, the social acceptability of male domination commonly supports the belief that the men should be the head of the household and responsible for earning money to support the family, but they also have decision-making authority. This role comes with a range of responsibilities and privileges. Conversely, the role of the woman is to take care of the children, care for the family members and elderly, manage household activities, and be sexually subservient. Traditional norms support a man’s right to inflict IPV when a wife fails to conform to certain traditional gender role expectations, for example, if a woman does not obey her elders, goes out without telling her partner, neglects their children, argues with him, refuses to have sex with him, or not having the food ready on time (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International, 2009), and as such it is considered that violent behaviour by a husband is justified when a wife fails to conform to such traditional role expectations (Hadi, 2005). Nearly one-third of women in Bangladesh believe that a husband is justified in beating his wife under certain circumstances with 23% accepting IPV as justified in the context of an argument (Rashid, Kader, Perera, & Sharma, 2014). Moreover, the majority of Bangladeshi men think that a wife is accountable to her husband for her behaviour and daily activities, and that violence is acceptable as a corrective punishment (Hadi, 2005; UNFPA, 2003). Therefore, women’s subordination is reflected in the sexual division of labour, lack of decision-making autonomy, restrictions on freedom of movement and differential access to resources within the family in many low- and middle-income countries, including Bangladesh (Hadi, 2000; Rashid, Kader, Perera, & Sharma, 2014).
There is little research on the impact of patriarchal dominance on the risk of IPV during pregnancy (Brownridge et al., 2011). IPV may originate from a man’s need to enforce power and control in his relationship (Daly & Chesney-Lind, 1988), and pregnancy may have a significant influence on the power dynamics of a relationship (Bacchus, Mezey, & Bewley, 2006). Pregnancy symbolizes the woman’s autonomous control over her own body and may represent a degree of independence from her partner (Bacchus, Mezey, & Bewley, 2006). Therefore, IPV during pregnancy may be due to the abusive partner’s attempt to re-establish his control over his partner (Bacchus, Mezey, & Bewley, 2006). During pregnancy, physical exhaustion, reduced mobility and a lack of emotional availability may limit women’s energy for her traditional duties as homemaker, which frequently may lead to an increased risk of IPV since abusers tend to hold more conventional sex role attitudes (Bacchus, Mezey, & Bewley, 2006; Jasinski, 2001; Noel & Yam, 1992).
Abused women likely have less decision-making power, decreased freedom of movement and higher economic dependency (Ellsberg, Peña, Herrera, Liljestrand, & Winkvist, 2000; Smith & Martin, 1995), which may reduce their ability to make decisions for themselves and their families, including the choice of receiving appropriate maternal health care services. Pregnancy may increase financial pressures, increasing women’s financial dependency on their male partners (Bacchus, Mezey, & Bewley, 2006; Pallitto, Campbell, & O’campo, 2005). Financial control by limiting access to money is one of the ways in which men seek to control and limit their partner’s freedom within abusive relationships (Bacchus, Mezey, & Bewley, 2006). Delayed entry in seeking reproductive health care services may be due to the controlling behaviour by the perpetrator (Koski, Stephenson, & Koenig, 2011).
Feminist theories, however, have been criticised for being an oversimplification of a complex issue with its focus on social and political structures rather than individual traits (Chornesky, 2000; Fonagy, 1999). They have also been criticised for overemphasizing men’s violence against women, while disregarding women’s use of violence (Renzetti, 2004). Social psychologists criticism of the conceptualization of traditional gender-role attitudes suggesting that current socio-political climate has changed remarkably now favouring a more egalitarian position for women, since the formulation of feminist theory (Glick & Fiske, 1997; Herzog, 2007). Against common perceptions, Glick and Fiske (1996, 1997) also argue that traditional attitudes about women’s role do not involve only highly negative or hostile feelings toward women (e.g., anger, antipathy, resentment) but also involve somewhat more positive and benevolent feelings (e.g., protective paternalism, idealization of women, and affection). Moreover, traditional gender-role attitudes are fundamentally ambivalent and involve both hostile and benevolent attitudes toward women (Glick & Fiske, 1996, 1997; McHugh & Frieze, 1997), and these positively evaluated traditional presumptions about women make them men’s “better half” (Glick & Fiske, 1997).
3.2.2 Social Learning Theory
Social learning theory is one of the most popular explanatory perspectives in the intimate partner violence literature (Mihalic & Elliott, 1997; Woodin & O’Leary, 2009). Despite having various types of social learning theories, almost all of these share a common view that violence and aggression are not inherent properties of the individual; rather they are learned behaviours (DeKeseredy & Schwartz, 2011; Mihalic & Elliott, 1997; Walker & Browne, 1985; Woodin & O’Leary, 2009). The violence learning process starts through role models provided by parents or peers and reinforces in childhood (Bell & Naugle, 2008; Bowen, 1993; Cochran, Branch, & Sellers, 2005; Mihalic & Elliott, 1997) and continues in adulthood as a coping mechanism to stress or a method of settling family conflicts (Bandura, 1978).
During childhood and adolescence, witnessing of how parents and relatives behave in their intimate relationships provides a training of behavioural alternatives (Mihalic & Elliott, 1997). The replication may happen at any time during adulthood even in the sensitive period of pregnancy (Godbout, Dutton, Lussier, & Sabourin, 2009; Mihalic & Elliott, 1997; Walker & Browne, 1985). Witnessing violence makes children as invisible victims, since children learn that (1) violence is an appropriate way to resolve conflicts; (2) violence is a part of family matters; (3) the abuser of IPV often goes unpunished; and (4) violence is a means to control other people (Massachusetts Coalition of Battered Women Service Groups, 1995). IPV, therefore, has an impact not only on its direct victims but also on the values and behaviour of children growing up in an abusive environment where they frequently witness violence (Henderson, Bartholomew, Trinke, & Kwong, 2005; Kovacs & Tomison, 2003; Straus, Gelles, & Steinmetz, 1980).
Several studies have demonstrated childhood victimization as well as witnessing IPV during childhood to be associated with adverse behavioural and emotional outcomes in children, including internalizing problems such as withdrawal, anxiety and depression, and externalizing problems such as conduct disorders, aggression and delinquency (Johnsona et al., 2002). A large number of studies have found evidence for the intergenerational “cycle of violence” hypothesis, which entails that violent and abusive adults learned this behaviour as a result of being the victims of or witnesses of aggressive and abusive behaviour during childhood and adolescence (Cochran, Branch, & Sellers, 2005; Mihalic & Elliott, 1997; Straus, Gelles, & Steinmetz, 1980; Tjaden & Thoennes, 2000). Therefore, victims and perpetrators of IPV are thought to have either witnessed violence or directly experienced physical abuse as children, resulting in the development of tolerance or acceptance of violence within the family (Bell & Naugle, 2008; Kovacs & Tomison, 2003; Lewis & Fremouw, 2001). Furthermore, positive results following IPV may increase a person’s expectations that future aggression will provide similar outcomes, ultimately results in continued use of violence (Riggs & O’Leary, 1989).
Social learning theory may have potential as apartial explanation for IPV against pregnant women (Taillieu & Brownridge, 2010). Taillieu and Brownridge (2010) propose that IPV during pregnancy may represent a continuation of a pattern of violence experienced by these women throughout their lives, and is not related to the pregnancy. A history of childhood victimization makes women more susceptible to experiencing IPV during pregnancy (Goodwin et al., 2000; Jasinski, 2004; Martin et al., 2004). In a study, Díaz-Olavarrieta et al. (2007) have reported that 25 out of the 99 women who have been abused during pregnancy also reported abuse during every life period about which they are asked. Dunn and Oths (2004) reported that 81% of women who reported IPV during pregnancy also reported it in the year prior. A study with convicted IPV perpetrators has found that witnessing IPV in the family of origin is significantly correlated with being physically abused, being physically punished, and being sexually abused in childhood (Burch & Gallup Jr., 2004). Besides, several longitudinal studies have shown that childhood exposure to IPV is significantly associated with increased odds of mental health problems, substance abuse, criminal offending (Fergusson & Horwood, 1998), suicidal ideation (Thompson et al., 2005), and suicide attempt (Dube et al., 2001).
One study from Bangladesh reports that one-fourth of women witnessed father-to-mother violence, and those women who witnessed such violence were 2.4 times more likely to experience any kind of IPV than women who never witnessed violence, suggesting that IPV passes from one generation to another (Islam, Tareque, Tiedt, & Hoque, 2014). Due to social learning, daughters may learn tolerance to IPV and receive no health care services during pregnancy from their mothers. Both longitudinal and prospective studies have established the link between early exposure to violence and IPV with more clarity (Godbout, Dutton, Lussier, & Sabourin, 2009), however, this relationship has not been explicitly explored as it relates specifically to the risk of IPV during pregnancy (Taillieu & Brownridge, 2010).
Social learning theory, however, is not without criticism. DeKeseredy & Schwartz (2011) suggested that many people who were raised in relatively nonviolent homes, abuse their female partners and children. Moreover, most of the children have a sense of justice and fairness, and many are likely to regard physical violence as evil (Dobash & Dobash, 1979). On the contrary, many people may have directly experienced child abuse or may have witnessed their fathers beat their mothers but they have never beaten their spouse or children (Barnett, Miller-Perrin, & Perrin, 2005). Many abused mothers may spend a substantial amount of time and effort to teach their children that physical violence is a wrong practice and should be avoided at any means (Dobash & Dobash, 1979).
3.2.3 Evolutionary Psychology Theory
Evolutionary psychology theories focus on survival and reproduction (Maner & Shackelford, 2008). According to evolutionary psychology theory, men are concerned with the continuation of their gene pool and violence is largely motivated by paternal uncertainty (Taillieu & Brownridge, 2010). Men have been historically and genetically more aggressive to compete effectively against other male rivals for sexual access to women for procreation (DeKeseredy & Schwartz, 2011; Fischer & Mosquera, 2001). Evolutionary theories of jealousy generate hypotheses about sex differences in responses to a long-term intimate partner’s emotional infidelity versus sexual infidelity (Maner & Shackelford, 2008). Evolutionary researchers state that jealousy in men is designed primarily to prevent unknowingly caring for a child that is not genetically his own (Cousins & Gangestad, 2007; Maner & Shackelford, 2008).
Because of internal fertilization, men can rarely be certain that their children are actually their own (Burch & Gallup Jr., 2004). Due to rape or infidelity, there is always a possibility that the children she bears are not his. Some evolutionary theorists argue that men use an array of “mate retention tactics” when they have younger as well as physically attractive partners. Men want to control female sexuality and to prevent predicted infidelity (Buss & Shackelford, 1997; Cousins & Gangestad, 2007), and violence is one tactic in that array (Buss & Duntley, 2011). To avert paternal uncertainty, therefore, men are especially likely to guard their partners when their partners are near ovulation since the risk of conception is highest at that period (Haselton & Gangestad, 2006) or consistently monitor their partners, or isolate them from other men (Burch & Gallup Jr., 2004). More severe mate retention tactics are applied to female partners who are suspected to be unfaithful, and physical abuse is the more severe one. One study reported that male partner’s sexual coercion is another consequence of men’s perceptions of a mate’s sexual infidelity (Goetz, Shackelford, & Camilleri, 2008).
The general perception from the vast majority of society in Bangladesh is that following marriage, a woman should be a perfect housewife and be loyal only to her husband. Extra-marital relationships are not acknowledged and frowned upon (Schuler & Islam, 2008). Therefore, male partner’s controlling behaviours are inflicted upon women of Bangladesh due to sexual jealousy and accusations of infidelity. Pallitto and O’Campo (2005) reported that male partner’s controlling behaviour might increase the risk to be experienced IPV during pregnancy. Delayed entry in seeking maternal health care services and restricted access to health services may be due to male partner’s controlling behaviour (Heise & Garcia-Moreno, 2002; Koski, Stephenson, & Koenig, 2011).
Some researchers have demonstrated that due to partners’ jealousy of other close relationships, abused pregnant women are often socially isolated by their male partners from family, friends and other social support systems (Bacchus, Mezey, & Bewley, 2006; Noel & Yam, 1992; Pulido, 2001; Wiemann, Agurcia, Berenson, Volk, & Rickert, 2000). This social isolation decreases pregnant women’s social support network (Taillieu & Brownridge, 2010).
Experts argue that the detection or suspicion of infidelity is one of the important predictors of IPV (Buss & Duntley, 2011; Daly, Wilson, & Weghorst, 1982), and sexual jealousy is a prime motivator for homicide (Wilson & Daly, 1996). A number of studies have demonstrated that abusive male partners tend to be more sexually jealous and possessive of their partners in comparison to non-abused males (Bacchus, Mezey, & Bewley, 2006; Burch & Gallup Jr., 2004; Chambliss, 2008; Decker, Martin, & Moracco, 2004), and doubts about paternity is one of the key factors of IPV within the relationship (Bacchus, Mezey, & Bewley, 2006). In a study with convicted IPV perpetrators, men with pregnant partners have reported significantly higher sexual jealousy scores than men whose partners are not pregnant (Burch & Gallup Jr., 2004). In summary, existing studies provide supportive evidence in favour of evolutionary psychology theory as a potential explanation for IPV during pregnancy.
3.3 Conceptual framework
The applicability and relevance of a particular theory explaining IPV must be tested within the specific cultural context and its normative roles (Loue, 2001). Building on the empirical literature on IPV during pregnancy, the unique aspects of Bangladeshi culture as they might impact how IPV plays out during pregnancy, and key explanatory theories, I propose the conceptual model detailed in figure 3.1.
A range of socio-demographic characteristics, obstetric and reproductive characteristics and psycho-socio-cultural characteristics are hypothesized to determine women’s exposure to different forms of IPV before, during and after pregnancy. Combined with these characteristics, exposure to IPV can compromise women’s reproductive health service utilization, and increase the risk of experiencing postpartum depression and early termination of exclusive breastfeeding. Additionally, IPV can compromise women’s health seeking due to stress and postpartum depression. It is also hypothesized that exposure to IPV, low use of maternal health services and postpartum depression may significantly influence mother’s exclusive breastfeeding practices. Moreover, IPV may be independently associated with maternal health service utilization, postpartum depression and mother’s exclusive breastfeeding.
The association between IPV during pregnancy and mother’s exclusive breastfeeding are poorly understood in the literature. There are also gaps in knowledge whether exposure to IPV during and after pregnancy independently associated with maternal health service utilization and experiencing postpartum depression. This conceptual model will assist in explaining these gaps.
3.4 Chapter summary
No single theory is likely sufficient to explain such a complex phenomenon, as the causes of IPV are multifactorial and somewhat elusive (Kelly, Gonzalex-Guarda, & Taylor, 2011). Complex behaviours, complicated thinking patterns, individual psychologies and the interactions among individuals and systems all can play a role in IPV (Hyde-Nolan & Juliao, 2012). An abuser’s controlling behaviour (Dutton, van Ginkel, & Landolt, 1996) may be exacerbated by pregnancy due to the stress and anxiety of first time parenting or having an unplanned pregnancy (Jasinski, 2004). Moreover, reduced attention given to the male partner during pregnancy is treated by the abusive partner as a threat to his positions of power, and may lead to perpetrate violence against the women during pregnancy (Bacchus, Bewley, & Mezey, 2001).
The lack of research on IPV during pregnancy in women of Bangladesh reflects the lack of application of theories that explain IPV during pregnancy. To address the gap in knowledge, this research will examine the three theories discussed above to determine whether they hold for the women of Bangladesh in explaining IPV during pregnancy. Dowry demands by husband, low level of social support and women’s decision-making autonomy explore the application of feminist theories. Correlates such as childhood exposure to violence and witnessing parental violence during childhood, explore the utilization of social learning theory. Husband’s controlling behaviour and unintended pregnancy pertain to evolutionary psychology theory. The findings will contribute to knowledge on theories explaining IPV during pregnancy.
The next chapter discusses the research methods that were utilized to collect data for analysis to examine IPV victimization and to explore the health consequences of IPV victimization during pregnancy among women in Bangladesh.
Methods and materials |
The research methods used to address the following two research questions are described in this chapter. Demographic characteristics of women of Bangladesh, research design, sampling processes, variables measures, data collection and analysis processes have been outlined in sequential phases in this chapter.
Research Questions:
RQ1 How do pregnancy and the postpartum period influence the prevalence of IPV?
RQ2 Does IPV influence delayed entry into prenatal care, postpartum depression, and mother’s exclusive breastfeeding?
To address these aforementioned research questions, this study broadly explores IPV situations before, during and after pregnancy for women of Bangladesh with specific aims to:
Aim-1: Examine IPV victimisation for pregnant women in Bangladesh.
| Aim 1.1 | : | Determine the prevalence of different forms of IPV before, during and after pregnancy; |
| Aim 1.2 | : | Examine the changing pattern of IPV victimisation before, during and after pregnancy; |
| Aim 1.3 | : | Identify and describe potential correlates of different types of IPV victimisation during pregnancy. |
Aim-2: Explore the health consequences of IPV victimisation for pregnant women in Bangladesh.
| Aim 2.1 | : | Examine the influence of IPV victimisation before and during pregnancy on delayed entry into prenatal care; |
| Aim 2.2 | : | Explore the association of postpartum depression in relation to maternal exposure to IPV before, during and after pregnancy; |
| Aim 2.3 | : | Examine the influence of IPV victimisation before, during and after pregnancy on exclusive breastfeeding. |
4.1 Study setting
The study was carried out in randomly selected expanded program of immunization (EPI) centres in two Upazilas (sub-district) of the Chandpur district of Bangladesh. For the smooth implementation of government programs, Bangladesh is administratively divided into 64 districts; each district is further subdivided into several Upazilas; each Upazila (except for those in the metropolitan area) into several Unions; each Union into nine Wards, and each Ward into several villages (GOB, 2016). The lowest administrative unit is a Ward, which has a population of around 8,000 to 10,000.
For vaccination purposes, each ward is divided into 8 sub-blocks based on the population, and each sub-block has an EPI outreach site where routine EPI services are provided once in a month for catchments of approximately 1,000 people. Almost all EPI outreach sites in a Ward are within 15-20 minutes walking distance. Health workers visit homes to register newborns (in the EPI Registration Book) and invite parents to bring their target children to vaccination sessions prior to the day of the session.
4.2 Research Design
A community-based cross-sectional study was conducted in Chandpur district of Bangladesh from October 2015 to January 2016. Interview data was collected from postpartum mothers who visited one of the 80 randomly selected EPI centres for their children’s vaccinations. EPI centres were chosen because women of reproductive age usually come to the centres to receive Tetanus vaccines for themselves, and compulsory vaccines (six preventable diseases-diphtheria, measles, pertussis, polio, tetanus, and tuberculosis) for their children (0–1year) provided free of charge by the government. Questions about IPV need to be asked in a setting that is safe and where the individual is alone (Family Violence Prevention Fund (FVPF), 2004; Shadigian & Bauer, 2004). This prevents the risk of a potential perpetrator being present during the interview session. Instead of households, vaccination centres were chosen because they represent an opportune site for providing a safe and private setting since husbands usually do not accompany their wives to the vaccination centres (Mohammadhosseini, Sahraean, & Bahrami, 2010). If the questionnaire was administered in the household, other family members, including spouses might remain present. In this situation, the respondent might not feel safe to disclose any sensitive information against her partner.
The questionnaire was developed in English and then translated into the Bengali language to collect information on socio-demographic, experience of IPV, the timing of the entry into prenatal care, postpartum depression, and exclusive breastfeeding practices. The questionnaire was developed from those used in international studies to suit Bangladeshi women. Before being used in this study, the questionnaire was piloted on a small number of Bengali speaking women (n = 15) to check for the questionnaire clarity, flow, design and completion time. After examining the feedback and responses from the pilot study, the format of the questionnaire was revised, a number of sections reorganised and the wording of some questions was modified. To ensure the quality of data collection, the principal researcher (Md. Jahirul Islam) monitored field activities through field visits every day.
4.3 Sample
4.3.1 Selection of study site
The study was carried out in two Upazilas of the Chandpur district that has 8 Upazilas (Haimchar, Faridganj, Kachua, Shahrasti, Matlab North, Matlab South, Hajiganj, and Chandpur Sadar) and 88 Unions (Banglapedia: National Encyclopedia of Bangladesh, 2012). With a population of 2.4 million, the district is situated 55 km southwest of the capital city of Dhaka (Wikipedia, 2014). The area is dominated by subsistence agriculture and characterized by diversity in socio-economic activities, ethnicity, culture and language. Therefore, the populations are mostly representative of the broader socio-economic segment and religion of the country. Regular flood and river bank erosion are common phenomena in this district. As a common scenario of Bangladesh, the majority of women are involved in household work and child rearing.
The rationale for choosing Chandpur district as study site is: (1) the populations are broadly representative of socioeconomic strata and religions of the country, (2) nearness to the capital city, making it convenient to move from Dhaka to the study site for the research purpose, (3) exceptionally diverse transportation systems (bus, train and launch) make it easy to connect with Dhaka and nearby districts as well as with other sub-districts of Chandpur district, (4) because of logistical and financial considerations, (5) If any abused and depressed women are detected, they could be referred to available support services to the locality or could be advised to go to Dhaka city for improved services due to easy transportation systems. The first four criteria minimize bias in site selection, and the last criteria assure the ethical obligation of the research of ensuring services to the abused women.
4.3.2 Sampling Process
The sample size was determined based on the expression: N
Childhood exposure to violence: Childhood physical abuse was measured by asking respondents if they had ever been beaten or physically mistreated in any way by anyone before 15 years of age. Childhood sexual abuse was measured by asking respondents if they had ever been forced to have sex, kissed, or forced to undress or perform sexual acts against their will before 15 years of age. Childhood psychological abuse was measured by asking respondents if they had ever been verbally abused by anyone other than their husband before 15 years of age (Godbout, Dutton, Lussier, & Sabourin, 2009; Pico-Alfonso et al., 2006). For each item, respondents answered either no (0) or yes (1). If respondents scored a 0 on all the three items, they were classified as having no childhood exposure to violence = 0, while those with any childhood exposure to violence scored a 1 on this measure.Witnessing parental violence in childhood: Witnessing parental violence in childhood (prior to 15 years old) was measured by asking respondents whether they had ever witnessed their father physically or verbally abusing their mother during their childhood (Godbout, Dutton, Lussier, & Sabourin, 2009; Pico-Alfonso et al., 2006). Response choices range from 0 (no) to 1 (yes).
4.7 Analytical strategies
The Statistical Packages for Social Science (SPSS version 22.0 for Windows, SPSS Inc., Chicago, IL, USA) was used for coding and analysing the data. Before analysing the data, a range of activities such as coding, data screening for finding out errors, data cleaning, replacing missing values and recoding were done. Firstly, the researcher himself performed the data entry process to ensure the data quality. The researcher randomly double-checked 10% of cases (included 45 cases) and the data entry error rate was below 1%. Secondly, respondent’s responses were checked visually at first and then, by using SPSS to identify any missing values or out of range values. Frequency analyses diagnosed no missing values or out of range values. Thirdly, negatively worded items in scales were reversed to compute total scores for the scale. Fourthly, all the continuous variables were transformed into categorical variables. After screening and cleaning, the researcher started data analysis. Analysis of the data comprised of descriptive statistics, bivariate analysis using Chi-square test, and multivariate logistic regression analysis.
4.7.1 Descriptive statistics
Descriptive statistics describe, show or summarise the features of the study sample in a meaningful way in terms of variable or combinations of variables (Pallant, 2007; Tabachnick & Fidell, 2013). A range of descriptive statistics was done for respondents’ socio-demographic characteristics, respondents’ obstetric and reproductive characteristics and psycho-socio-cultural characteristics. Frequencies and percentages were used to summarise all categorical variables.
Socio-demographic characteristics of the respondents are displayed in Table 4.2. Approximately quarter of the women (24.9%) were 14–18 years old, just less than half of the women (43.9%) were 19–24 years old and one-third or the women (31.2%) were ≥25 years old during their pregnancy. Only 8.2% of the respondents had received no formal education and 58.5% of the women attained secondary and higher education. Regarding respondents’ husband education, on the other hand, only 13.6% had attained no formal education and 50.9% attained secondary and higher education. Approximately, 68.5% of them lived in rural areas, and nearly 60% lived in a nuclear family at the time of the survey. Nearly 38.3% women had an average monthly income less than or equal to the national average (8500 BDT ~ 109 USD).
Table 4.2: Summary statistics for the respondents’ socio-demographic characteristics
| Characteristics | n | % |
| Women’s age during last pregnancy (tertiles) | ||
| 14-18 | 106 | 24.9 |
| 19-24 | 187 | 43.9 |
| ≥25 | 133 | 31.2 |
| Women’s education | ||
| No education | 35 | 8.2 |
| Primary | 104 | 24.4 |
| Secondary and higher | 287 | 67.4 |
| Husband’s education | ||
| No education | 58 | 13.6 |
| Primary | 151 | 35.4 |
| Secondary and higher | 217 | 50.9 |
| Area of residence | ||
| Rural | 292 | 68.5 |
| Urban | 134 | 31.5 |
| Family structure | ||
| Extended | 171 | 40.1 |
| Nuclear | 255 | 59.9 |
| Family income | ||
| ≤8500 | 163 | 38.3 |
| >8500 | 263 | 61.7 |
Regarding women’s Obstetric and reproductive characteristics (see Table 4.3), nearly two-fifths of their children were 3–4 and 5–6 months old each. About 41.1% of women had one child (primiparous) and 26.5% had three children or more. Nearly one-fifth (22.1%) had two children less than five years of age. Approximately, 57% of women reported that their husband had a preference for a son. One in ten women described her health status as bad. Furthermore, one-fourth of their last pregnancies was unintended, 16.2% of women had experienced complications during childbirth, and approximately three quarter (73.9%) of women received insufficient ANC (< four visits) during their last pregnancy. Approximately, 69.2% of women had vaginal deliveries, and both the home and medical facility shared the equal proportion (50%) as a place of giving birth. Just over half (56.8%) of the women reported that they could initiate breastfeeding within 24h of childbirth.
Table 4.3: Summary statistics of the respondents’ Obstetric and reproductive characteristics (N = 426)
| Characteristics | n | % |
| Age of the last child, month | ||
| 1–2 | 88 | 20.7 |
| 3–4 | 168 | 39.4 |
| 5–6 | 170 | 39.9 |
| Number of children | ||
| 1 | 175 | 41.1 |
| 2 | 138 | 32.4 |
| ≥3 | 113 | 26.5 |
| Parity | ||
| Primiparous | 175 | 41.1 |
| Multiparous | 251 | 58.9 |
| Number of children less than five years of age | ||
| 1 | 332 | 77.9 |
| 2 | 94 | 22.1 |
| Pregnancy intention | ||
| Unintended | 107 | 25.1 |
| Intended | 319 | 74.9 |
| Complications during childbirth | ||
| No | 357 | 83.8 |
| Yes | 69 | 16.2 |
| Number of antenatal care (ANC) visits | ||
| < four times | 315 | 73.9 |
| ≥ four times | 111 | 26.1 |
| Husband’s preference for a son | ||
| No | 242 | 56.8 |
| Yes | 184 | 43.2 |
| Mode of childbirth | ||
| Caesarean section | 131 | 30.8 |
| Vaginal | 295 | 69.2 |
| Place of childbirth | ||
| Birth at home | 213 | 50.0 |
| Birth at medical facility | 213 | 50.0 |
| Breastfeeding initiation | ||
| Immediately | 249 | 58.5 |
| Late | 177 | 41.5 |
| Maternal general health status | ||
| Good | 247 | 58.0 |
| Fair | 135 | 31.7 |
| Bad | 44 | 10.3 |
Psycho-socio-cultural characteristics are illustrated in Table 4.4. Regarding decision-making autonomy, 25.8% had low, 41.1% had moderate and 33.1% had high decision-making autonomy. Nearly, 30.0% of women had low, 37.1% had medium and 32.9% had high social support. Regarding traditional gender role attitude, 37.8% had low, 23.9% had medium and 38.3% had high traditional gender roles acceptance. Two-thirds (63.4%) of marriages involved dowry demands and one-third of the women (29.6%) reported relationship difficulties with their mother-in-law. Nearly one-third of women (30.0%) had limited social support and more than half of the women (58.5%) had low self-esteem. Approximately 57% of women had high perceived stress and nearly 26.8% of women reported a prior history of depressive symptoms.
Nearly 85.0% of the respondents’ husband was not addicted to any substance, 5.6% were taken alcohol, 6.6% were addicted to the drug and 3.1% were addicted to both alcohol and drug. Regarding husband’s controlling attitude, 33.3% were less controlling, 39.0% was moderately controlling and 27.7% were highly controlling. About 56.1% of women witnessed parental violence (physical or psychological) during their childhood and 55.6% of women experienced any childhood violence.
Table 4.4: Summary statistics of the respondents’ psycho-socio-cultural characteristics (N = 426)
| Characteristics | n | % |
| Traditional gender roles attitude (tertiles) | ||
| Low | 161 | 37.8 |
| Medium | 102 | 23.9 |
| High | 163 | 38.3 |
| Decision-making autonomy (Tertiles) | ||
| Low | 110 | 25.8 |
| Moderate | 175 | 41.1 |
| High | 141 | 33.1 |
| Husband’s controlling behaviours (tertiles) | ||
| Less controlling | 142 | 33.3 |
| Moderately controlling | 166 | 39.0 |
| Highly controlling | 118 | 27.7 |
| Dowry demands at marriage | ||
| No | 156 | 36.6 |
| Yes | 270 | 63.4 |
| Relationship with mother-in-law | ||
| Bad | 126 | 29.6 |
| Mild | 188 | 44.1 |
| Good | 112 | 26.3 |
| Social support (tertiles) | ||
| Low | 128 | 30.0 |
| Medium | 158 | 37.1 |
| High | 140 | 32.9 |
| Self-esteem | ||
| Low | 249 | 58.5 |
| High | 177 | 41.5 |
| Perceived stress | ||
| Low | 183 | 43.0 |
| High | 243 | 57.0 |
| Previous depressive symptoms | ||
| No | 312 | 73.2 |
| Yes | 114 | 26.8 |
| Witnessing parental violence in childhood
|
||
| No | 187 | 43.9 |
| Yes | 239 | 56.1 |
| Any childhood exposure to violence | ||
| No | 189 | 44.4 |
| Yes | 237 | 55.6 |
| Substance abuse | ||
| None | 361 | 84.7 |
| Alcohol | 24 | 5.6 |
| Drug | 28 | 6.6 |
| Both | 13 | 3.1 |
4.7.2 Reliability analysis for scales
Reliability analysis refers to the internal consistency of a scale to which a scale produces consistent results across different situations (Pallant, 2007). The internal consistency of different scales for this research was measured using Cronbach’s alpha (α). Theoretically, Cronbach’s alpha is a function of the number of items of a scale, the average covariance between pairs of items, and the variance of the total score of a scale (Field, 2009; Pallant, 2007). A summary of the scale reliability is shown in Table 4.5. Even though sexual IPV before, during and after pregnancy had low Cronbach’s alpha values, these instruments were used for this research since these instruments were important to know why IPV occurs.
Table 4.5: Summary of Cronbach’s alphas for scales used in this study
| Scale | Items | Cronbach’s alpha | Standardised Item alpha |
| Physical IPV before pregnancy | 7 | .83 | .81 |
| Physical IPV during pregnancy | 7 | .78 | .77 |
| Physical IPV after pregnancy | 7 | .86 | .84 |
| Sexual IPV before pregnancy | 3 | .40 | .53 |
| Sexual IPV during pregnancy | 3 | .35 | .56 |
| Sexual IPV after pregnancy
V |
3 | .47 | .67 |
| Psychological IPV before pregnancy | 6 | .73 | .74 |
| Psychological IPV during pregnancy | 6 | .71 | .70 |
| Psychological IPV after pregnancy | 6 | .75 | .75 |
| Husband’s controlling behaviours | 7 | .72 | .71 |
| Women’s decision-making autonomy | 6 | .87 | .87 |
| Traditional gender roles attitudes | 6 | .85 | .85 |
| Postpartum depression | 10 | .86 | .86 |
| Perceived stress | 10 | .93 | .93 |
| Self-esteem | 10 | .84 | .83 |
| Social support | 10 | .90 | .91 |
4.7.3 Bivariate statistical analysis
Aims 1.1 and 1.2 are descriptive in nature. The  analysis assesses and compares the prevalence of the different types of IPV before, during and after pregnancy. To address Aim 1.3, bivariate
analysis assesses and compares the prevalence of the different types of IPV before, during and after pregnancy. To address Aim 1.3, bivariate  analysis tested linear associations between predictor variables (socio-demographic characteristics, relationship characteristics and behavioural characteristics) and different forms of IPV during pregnancy. Furthermore, to address Aim 2.1, 2.2 and 2.3, bivariate
analysis tested linear associations between predictor variables (socio-demographic characteristics, relationship characteristics and behavioural characteristics) and different forms of IPV during pregnancy. Furthermore, to address Aim 2.1, 2.2 and 2.3, bivariate  analysis was utilized to identify the distributions of the outcome variables (delayed entry into prenatal care, postpartum depression and exclusive breastfeeding) by selected covariates. Results from the bivariate analysis are illustrated in Chapter 5 and Chapter 6 (Table 5.1, Table 6.1, Table 6.4 and Table 6.9).
analysis was utilized to identify the distributions of the outcome variables (delayed entry into prenatal care, postpartum depression and exclusive breastfeeding) by selected covariates. Results from the bivariate analysis are illustrated in Chapter 5 and Chapter 6 (Table 5.1, Table 6.1, Table 6.4 and Table 6.9).
4.7.4 Multivariate logistic analysis
Logistic regression analysis is an appropriate technique for predicting a dichotomous outcome variable from a list of predictor variables. Logistic regression does not assume linearity of variables, normal distributions of variables or homoscedasticity (Tabachnick & Fidell, 2013). Before logistic regression analyses were conducted, the multicollinearity of all independent variables was checked using a cut-off variance inflation factor (VIF) of 2.50 or above (Field, 2009; Pallant, 2007), to establish if they were highly correlated. IPV prior to pregnancy had a high correlation with IPV during pregnancy (correlation of physical, psychological and any form of IPV between before and during pregnancy are .70, .90, and .84 respectively), and was excluded from the multivariate analysis. A two-tailed p-value of <.05 was set to refer the level of statistical significance.
Since all of the predictor variables and outcome variables (physical IPV, sexual IPV, psychological IPV and any IPV) in Aim 1.3 were categorical, four logistic regression analyses were conducted, one for each type of IPV during pregnancy to assess multivariate associations between the relevant predictors and outcome variables. Furthermore, in addressing Aim 2.1, 2.2 and 2.3, multivariate logistic regression models were used to estimate adjusted odds ratios (AOR) and 95% confidence intervals to compare the strength of the associations between each of the factors and selected health consequences (delayed entry into prenatal care, postpartum depression and exclusive breastfeeding). Results from the multivariate logistic analysis are presented in Chapter 5 and Chapter 6 (Table 5.2, Table 6.2, Table 6.3, Table 6.5, Table 6.6, Table 6.7, Table 6.10, Table 6.11 and Table 6.12).
4.8 Chapter summary
The research design and data collection procedure were described in this chapter. The independent and dependent variables of the study were illustrated here. The data analysis strategies in addressing the research aims were discussed in this chapter. Descriptive statistics for the respondents and reliability statistics for the scales used in this study were described in this chapter. The results of the analyses and their discussion will be illustrated in the next four chapters.
References:
Aarts, C., Kylberg, E., Hornell, A., Hofvander, Y., Gebre-Medhin, M., & Greiner, T. (2000). How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. International journal of epidemiology, 29, 1041-1046.
Abedin, S., Islam, R., & Hossain, T. (2008). Antenatal care during pregnancy: A study on Naogaon district of Bangladesh. The Social Sciences, 3(8), 537-541.
Ackerson, L. K., & Subramanian, S. V. (2008). State gender inequality, socioeconomic status and intimate partner violence (IPV) in India: A multilevel analysis. Australian Journal of Social Issues, 43(1), 81-102.
Afsana, K., Rashid, S. F., Thurston, W., & BRAC, B. (2005). Challenges and gaps in addressing domestic violence in Health Policy of Bangladesh. BRAC, Bangladesh.
Agrawal, A., Ickovics, J., Lewis, J. B., Magriples, U., & Kershaw, T. S. (2014). Postpartum intimate partner violence and health risks among young mothers in the United States: A prospective study. Maternal and child health journal, 1-8.
Amaro, H., Fried, L. E., Cabral, H., & Zuckerman, B. (1990). Violence during pregnancy and substance use. Am J Public Health, 80(5), 575-579.
Amin, R., Shah, N. M., & Becker, S. (2010). Socioeconomic factors differentiating maternal and child health-seeking behavior in rural Bangladesh: A cross-sectional analysis. Int J Equity Health, 9(9), 1-12.
Amnesty International. (2004). Making violence against women count: Facts and Figures – a summary. ACT 77/034/2004 (Public). Retrieved 8 December, 2014
Annan, S. L. (2008). Intimate Partner Violence in Rural Environments. Annual Review of Nursing Research, 26, 85-113.
Ashrafun, L., & Säävälä, M. (2014). Domestic violence made public: A case study of the use of alternative dispute resolution among underprivileged women in Bangladesh. Contemporary South Asia, 22(2), 189-202.
Åsling‐Monemi, K., Tabassum Naved, R., & Persson, L. Å. (2008). Violence against women and the risk of under‐five mortality: analysis of community‐based data from rural Bangladesh. Acta Paediatrica, 97(2), 226-232.
Audi, C. A. F., Segall-Correa, A. M., Santiago, S. M., Andrade, M. d. G. G., & Perez-Escamilla, R. (2008). Violence against pregnant women: prevalence and associated factors. Revista de Saúde Pública, 42(5).
Australian Bureau of Statistics (ABS). (2013). Bridging the data gaps for family, domestic and sexual violence, Australia. Canberra: ABS.
Babu, B. V., & Kar, S. K. (2010). Domestic violence in Eastern India: factors associated with victimization and perpetration. Public health, 124(3), 136-148.
Bacchus, L., Bewley, S., & Mezey, G. (2001). Domestic violence in pregnancy. Fetal and Maternal Medicine Review, 12(4), 249-271.
Bacchus, L., Mezey, G., & Bewley, S. (2004). Domestic violence: prevalence in pregnant women and associations with physical and psychological health. European Journal of Obstetrics & Gynecology and Reproductive Biology, 113(1), 6-11.
Bacchus, L., Mezey, G., & Bewley, S. (2006). A qualitative exploration of the nature of domestic violence in pregnancy. Violence Against Women, 12(6), 588-604.
Bailey, B. A., & Daugherty, R. A. (2007). Intimate partner violence during pregnancy: incidence and associated health behaviors in a rural population. Maternal and child health journal, 11(5), 495-503.
Ballard, T. J., Saltzman, L. E., Gazmararian, J. A., Spitz, A. M., Lazorick, S., & Marks, J. S. (1998). Violence during pregnancy: measurement issues. Am J Public Health, 88(2), 274-276.
Bandura, A. (1978). Social learning theory of aggression. The Journal of communication, 28(3), 12-29.
Bangladesh Bureau of Statistics (BBS). (2013). Violence against women survey 2011. Dhaka, Bangladesh: Bangladesh Bureau of Statistics (BBS).
Banglapedia: National Encyclopedia of Bangladesh. (2012). Chandpur District. Retrieved 27 October 2014, from http://www.banglapedia.org/HT/C_0132.htm
Barnett, O. W., Miller-Perrin, C. L., & Perrin, R. D. (2005). Family violence across the lifespan: an introduction (2nd ed.). Thousand Oaks: Sage Publications.
Barrett, M. l. (1980). Women’s oppression today: problems in Marxist feminist analysis. London: Verso Editions and NLB.
Bates, L. M., Schuler, S. R., Islam, F., & Islam, M. K. (2004). Socioeconomic factors and processes associated with domestic violence in rural Bangladesh. International family planning perspectives, 30(4).
Bell, C. C., & Mattis, J. (2000). The importance of cultural competence in ministering to African American victims of domestic violence. Violence Against Women, 6(5), 515-532.
Bell, K. M., & Naugle, A. E. (2008). Intimate partner violence theoretical considerations: Moving towards a contextual framework. Clinical psychology review, 28(7), 1096-1107.
Belli, R. F., Shay, W. L., & Stafford, F. P. (2001). Event History Calendars and Question List Surveys: A Direct Comparison of Interviewing Methods. The Public Opinion Quarterly, 65(1), 45-74.
Beydoun, M. A., Beydoun, H. A., Al-Sahab, B., & Tamim, H. (2010). Intimate Partner Violence as a Risk Factor for Postpartum Depression Among Canadian Women in the Maternity Experience Survey. Annals of Epidemiology, 20(8), 575-583.
Bhuiya, A., Sharmin, T., & Hanifi, S. M. A. (2003). Nature of domestic violence against women in a rural area of Bangladesh: implication for preventive interventions. Journal of Health, Population and Nutrition, 21(1), 48-54.
Bohn, D. K., Tebben, J. G., & Campbell, J. C. (2004). Influences of income, education, age, and ethnicity on physical abuse before and during pregnancy. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 33(5), 561-571.
Bondas, T., & Eriksson, K. (2001). Women’s lived experiences of pregnancy: A tapestry of joy and suffering. Qualitative Health Research, 11(6), 824-840.
Bonomi, A. E., Thompson, R. S., Anderson, M., Reid, R. J., Carrell, D., Dimer, J. A., & Rivara, F. P. (2006). Intimate partner violence and women’s physical, mental, and social functioning. American journal of preventive medicine, 30(6), 458-466.
Bost, K. K., Cox, M. J., Burchinal, M. R., & Payne, C. (2002). Structural and Supportive Changes in Couples’ Family and Friendship Networks across the Transition to Parenthood. Journal of Marriage and Family, 64(2), 517-531.
Bowen, E., Heron, J., Waylen, A., & Wolke, D. (2005). Domestic violence risk during and after pregnancy: findings from a British longitudinal study. BJOG: An International Journal of Obstetrics & Gynaecology, 112(8), 1083-1089.
Bowen, M. (1993). Family therapy in clinical practice. New York: Jason Aronson.
Brewer, V. E., & Paulsen, D. J. (1999). A Comparison of U.S. and Canadian Findings on Uxoricide Risk for Women with Children Sired by Previous Partners. Homicide Studies, 3(4), 317-332.
Brown, J. S., Posner, S. F., & Stewart, A. L. (1999). Urge incontinence: new health-related quality of life measures. Journal of the American Geriatrics Society, 47(8), 980.
Brown, S. J., McDonald, E. A., & Krastev, A. H. (2008). Fear of an intimate partner and women’s health in early pregnancy: findings from the Maternal Health Study. Birth, 35(4), 293-302.
Brownridge, D. A., Taillieu, T. L., Tyler, K. A., Tiwari, A., Chan, K. L., & Santos, S. C. (2011). Pregnancy and intimate partner violence: Risk factors, severity, and health effects. Violence Against Women, 17(7), 858-881.
Burch, R. L., & Gallup Jr., G. G. (2004). Pregnancy as a stimulus for domestic violence. Journal of family violence, 19(4), 243-247.
Buss, D. M., & Duntley, J. D. (2011). The evolution of intimate partner violence. Aggression and Violent Behavior, 16(5), 411-419.
Buss, D. M., & Shackelford, T. K. (1997). From Vigilance to Violence: Mate Retention Tactics in Married Couples. Journal of personality and social psychology, 72(2), 346-361.
Byrne, C. A., Resnick, H. S., Kilpatrick, D. G., Best, C. L., & Saunders, B. E. (1999). The socioeconomic impact of interpersonal violence on women. Journal of consulting and clinical psychology, 67(3), 362-366.
Cain, M., Khanam, S. R., & Nahar, S. (1979). Class, Patriarchy, and Women’s Work in Bangladesh. Population and Development Review, 5(3), 405-438.
Campbell, J. C. (2002). Health consequences of intimate partner violence. The Lancet, 359(9314), 1331-1336.
Campbell, J. C., Garcia-Moreno, C., & Sharps, P. (2004). Abuse during pregnancy in industrialized and developing countries. Violence Against Women, 10(7), 770-789.
Campbell, J. C., Jones, A. S., Dienemann, J., Kub, J., Schollenberger, J., O’campo, P., Gielen, A. C., & Wynne, C. (2002). Intimate partner violence and physical health consequences. Archives of internal medicine, 162(10), 1157-1163.
Campbell, J. C., & Lewandowski, L. A. (1997). Mental and physical health effects of intimate partner violence on women and children. Psychiatric Clinics of North America, 20(2), 353-374.
Campbell, J. C., Oliver, C., & Bullock, L. (1993). Why battering during pregnancy? AWHONN”s Clinical Issues Perinat Womens Health Nursing, 4(3), 343-349.
Campbell, J. C., Poland, M. L., Waller, J. B., & Ager, J. (1992). Correlates of battering during pregnancy. Research in nursing & health, 15(3), 219-226.
Castro, R., Peek-Asa, C., & Ruiz, A. (2003). Violence against women in Mexico: a study of abuse before and during pregnancy. Am J Public Health, 93(7), 1110-1116.
Certain, H. E., Mueller, M., Jagodzinski, T., & Fleming, M. (2008). Domestic abuse during the previous year in a sample of postpartum women. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 37(1), 35-41.
Cha, S., & Masho, S. W. (2014). Intimate partner violence and utilization of prenatal care in the United States. J Interpers Violence, 29(5), 911-927.
Chakraborty, N., Islam, M. A., Chowdhury, R. I., & Bari, W. (2002). Utilisation of postnatal care in Bangladesh: evidence from a longitudinal study. Health & Social Care in the Community, 10(6), 492-502.
Chakraborty, N., Islam, M. A., Chowdhury, R. I., Bari, W., & Akhter, H. H. (2003). Determinants of the use of maternal health services in rural Bangladesh. Health Promotion International, 18(4), 327-337.
Chambliss, L. R. (2008). Intimate partner violence and its implication for pregnancy. Clinical Obstetrics and Gynecology, 51(2), 385-397.
Chan, K. L., Brownridge, D. A., Tiwari, A., Fong, D. Y., Leung, W. C., & Ho, P. C. (2011). Associating pregnancy with partner violence against Chinese women. J Interpers Violence, 26(7), 1478-1500.
Chandran, M., Tharyan, P., Muliyil, J., & Abraham, S. (2002). Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India: Incidence and risk factors. the British journal Of psychiatry, 181(6), 499-504.
Chang, J., Berg, C. J., Saltzman, L. E., & Herndon, J. (2005). Homicide: A leading cause of injury deaths among pregnant and postpartum women in the United States, 1991–1999. Am J Public Health, 95(3), 471.
Chang, J. C., Cluss, P. A., Ranieri, L., Hawker, L., Buranosky, R., Dado, D., McNeil, M., & Scholle, S. H. (2005). Health care interventions for intimate partner violence: What women want. Women’s health issues, 15(1), 21-30.
Charles, P., & Perreira, K. M. (2007). Intimate partner violence during pregnancy and 1-year post-partum. Journal of family violence, 22(7), 609-619.
Chaudhury, R. (2008). Multi-sectoral determinants of maternal mortality in Bangladesh. Paper presented at the Hefei, Anhui Province, China: Workshop on addressing multi-sectoral determinants of maternal mortality ESCAP Region.
Cheng, D., & Horon, I. L. (2010). Intimate-partner homicide among pregnant and postpartum women. Obstetrics and gynecology, 115(6), 1181-1186.
Chornesky, A. (2000). The Dynamics of Battering Revisited. Affilia, 15(4), 480-501.
Choudhury, K. K., Hanifi, M. A., Rasheed, S., & Bhuiya, A. (2000). Gender inequality and severe malnutrition among children in a remote rural area of Bangladesh. J Health Popul Nutr, 18(3), 123-130.
Clark, C. J., Hill, A., Jabbar, K., & Silverman, J. G. (2009). Violence during pregnancy in Jordan: its prevalence and associated risk and protective factors. Violence Against Women, 15(6), 720-735.
Cochran, J. K., Branch, K. A., & Sellers, C. S. (2005). Social learning theory and partner violence: A research note. Deviant Behavior, 26(4), 379-395.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A Global Measure of Perceived Stress. Journal of health and social behavior, 24(4), 385-396.
Coker, A. L., Smith, P. H., Bethea, L., King, M. R., & McKeown, R. E. (2000). Physical health consequences of physical and psychological intimate partner violence. Archives of Family Medicine, 9(5), 451-457.
Cook, K. J., & Kaya, Y. (2010). A cross-national analysis of physical intimate partner violence against women. International Journal of Comparative Sociology, 51(6), 423-444.
Cooper, P. J., & Murray, L. (1998). Postnatal depression. BMJ: British Medical Journal, 316(7148), 1884-1886.
Cousins, A. J., & Gangestad, S. W. (2007). Perceived threats of female infidelity, male proprietariness, and violence in college dating couples. Violence and victims, 22(6), 651-668.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. the British journal Of psychiatry, 150(6), 782-786.
Cripe, S. M., Sanchez, S. E., Perales, M. T., Lam, N., Garcia, P., & Williams, M. A. (2008). Association of intimate partner physical and sexual violence with unintended pregnancy among pregnant women in Peru. International Journal of Gynecology & Obstetrics, 100(2), 104-108.
Dalal, K., Rahman, F., & Jansson, B. (2009). Wife abuse in rural Bangladesh. J Biosoc Sci, 41(5), 561-573.
Daly, K., & Chesney-Lind, M. (1988). Feminism and criminology. Justice Quarterly, 5(4), 497-538.
Daly, M., Wilson, M., & Weghorst, S. J. (1982). Male sexual jealousy. Ethology and Sociobiology, 3(1), 11-27.
Daoud, N., Urquia, M. L., O’Campo, P., Heaman, M., Janssen, P. A., Smylie, J., & Thiessen, K. (2012). Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. Am J Public Health, 102(10), 1893-1901.
Datner, E. M., Wiebe, D. J., Brensinger, C. M., & Nelson, D. B. (2007). Identifying pregnant women experiencing domestic violence in an urban emergency department. J Interpers Violence, 22(1), 124-135.
de Jager, E., Skouteris, H., Broadbent, J., Amir, L., & Mellor, K. (2013). Psychosocial correlates of exclusive breastfeeding: A systematic review. Midwifery, 29(5), 506-518.
Decker, M. R., Martin, S. L., & Moracco, K. E. (2004). Homicide risk factors among pregnant women abused by their partners: Who leaves the perpetrator and who stays? Violence Against Women, 10(5), 498-513.
DeKeseredy, W. S., & Schwartz, M. D. (2011). Theoretical and definitional issues in violence against women. Sourcebook on violence against women (3-20). Thousand Oaks, CA: Sage.
Desmarais, S. L., Pritchard, A., Lowder, E. M., & Janssen, P. A. (2014). Intimate partner abuse before and during pregnancy as risk factors for postpartum mental health problems. BMC Pregnancy Childbirth, 14(1), 132-132.
Devries, K. M., Kishor, S., Johnson, H., Stöckl, H., Bacchus, L. J., Garcia-Moreno, C., & Watts, C. (2010). Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reproductive Health Matters, 18(36), 158-170.
Deyessa, N., Berhane, Y., Alem, A., Ellsberg, M., Emmelin, M., Hogberg, U., & Kullgren, G. (2009). Intimate partner violence and depression among women in rural Ethiopia: a cross-sectional study. Clinical Practice and Epidemiology in Mental Health, 5(8).
Díaz-Olavarrieta, C., Paz, F., Abuabara, K., Martínez Ayala, H. B., Kolstad, K., & Palermo, T. (2007). Abuse during pregnancy in Mexico City. International Journal of Gynaecology and Obstetrics, 97(1), 57-64.
Dietz, P. M., Gazmararian, J. A., Goodwin, M. M., Bruce, F. C., Johnson, C. H., & Rochat, R. W. (1997). Delayed entry into prenatal care: effect of physical violence. Obstetrics & Gynecology, 90(2), 221-224.
Dillon, G., Hussain, R., Loxton, D., & Rahman, S. (2013). Mental and Physical Health and Intimate Partner Violence against Women: A Review of the Literature. International journal of family medicine, 2013, 313909-313915.
DiPietro, J. A., Hilton, S. C., Hawkins, M., Costigan, K. A., & Pressman, E. K. (2002). Maternal stress and affect influence fetal neurobehavioral development. Developmental psychology, 38(5), 659-668.
Dixon, L., & Graham-Kevan, N. (2011). Understanding the nature and etiology of intimate partner violence and implications for practice and policy. Clinical psychology review, 31(7), 1145-1155.
Dobash, R. E., & Dobash, R. (1979). Violence against wives: a case against the patriarchy. New York: Free Press.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Jama, 286(24), 3089-3096.
Dunn, L. L., & Oths, K. S. (2004). Prenatal predictors of intimate partner abuse. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 33(1), 54-63.
Dutton, D. G., van Ginkel, C., & Landolt, M. A. (1996). Jealousy, intimate abusiveness, and intrusiveness. Journal of family violence, 11(4), 411-423.
Dyson, T., & Moore, M. (1983). On Kinship Structure, Female Autonomy, and Demographic Behavior in India. Population and Development Review, 9(1), 35-60.
Ellsberg, M. (2006). Violence against women and the Millennium Development Goals: Facilitating women’s access to support. International Journal of Gynecology & Obstetrics, 94(3), 325-332.
Ellsberg, M., & Heise, L. (2005). Researching Violence Against Women: A Practical Guide for Researchers and Activists. Washington DC, United States: The World Health Organization, PATH.
Ellsberg, M., Heise, L., Pena, R., Agurto, S., & Winkvist, A. (2001). Researching domestic violence against women: methodological and ethical considerations. Stud Fam Plann, 32(1), 1-16.
Ellsberg, M., Jansen, H. A. F. M., Heise, L., Watts, C. H., & Garcia-Moreno, C. (2008). Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet, 371(9619), 1165-1172.
Ellsberg, M., Peña, R., Herrera, A., Liljestrand, J., & Winkvist, A. (2000). Candies in hell: women’s experiences of violence in Nicaragua. Social Science & Medicine, 51(11), 1595-1610.
Escribà-Agüir, V., Ruiz-Pérez, I., & Saurel-Cubizolles, M.-J. (2007). Screening for domestic violence during pregnancy. Journal of Psychosomatic Obstetrics & Gynecology, 28(3), 133-134.
Eskenazi, B., & Pearson, K. (1988). Validation of a self-administered questionnaire for assessing occupational and environmental exposures of pregnant women. American journal of epidemiology, 128(5), 1117-1129.
Ezechi, O. C., Kalu, B. K., Ezechi, L. O., Nwokoro, C. A., Ndububa, V. I., & Okeke, G. C. E. (2004). Prevalence and pattern of domestic violence against pregnant Nigerian women. Journal of Obstetrics & Gynaecology, 24(6), 652-656.
Family Violence Prevention Fund (FVPF). (2004). National consensus guidelines on identifying and responding to domestic violence victimization in health care settings: FVPF.
Fanslow, J., Silva, M., Robinson, E., & Whitehead, A. (2008). Violence during pregnancy: Associations with pregnancy intendedness, pregnancy-related care, and alcohol and tobacco use among a representative sample of New Zealand women. Australian and New Zealand Journal of Obstetrics and Gynaecology, 48(4), 398-404.
Fanslow, J., Silva, M., Whitehead, A., & Robinson, E. (2008). Pregnancy outcomes and intimate partner violence in New Zealand. Australian and New Zealand Journal of Obstetrics and Gynaecology, 48(4), 391-397.
Farid, M., Saleem, S., Karim, M. S., & Hatcher, J. (2008). Spousal abuse during pregnancy in Karachi, Pakistan. International Journal of Gynaecology and Obstetrics, 101(2), 141-145.
Fawole, A. O., Hunyinbo, K. I., & Fawole, O. I. (2008). Prevalence of violence against pregnant women in Abeokuta, Nigeria. Australian and New Zealand Journal of Obstetrics and Gynaecology, 48(4), 405-414.
Fergusson, D. M., & Horwood, L. J. (1998). Exposure to interparental violence in childhood and psychosocial adjustment in young adulthood. Child Abuse and Neglect, 22(5), 339-357.
Field, A. P. (2009). Discovering statistics using SPSS (3rd ed.). Los Angeles; London: Sage.
Fikree, F. F., & Bhatti, L. I. (1999). Domestic violence and health of Pakistani women. International Journal of Gynecology & Obstetrics, 65(2), 195-201.
Fikree, F. F., Jafarey, S. N., Korejo, R., Afshan, A., & Durocher, J. M. (2006). Intimate partner violence before and during pregnancy: experiences of postpartum women in Karachi, Pakistan. J Pak Med Assoc, 56(6), 252-257.
Fischer, A. H., & Mosquera, P. M. R. (2001). What concerns men? Women or other men?: A critical appraisal of the evolutionary theory of sex differences in aggression. Psychology, Evolution & Gender, 3(1), 5-25.
Fisher, J., Mello, M. C. d., Patel, V., Rahman, A., Tran, T., Holton, S., & Holmes, W. (2012). Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization, 90(2), 139-149.
Fisher, J., Tran, T. D., Biggs, B., Dang, T. H., Nguyen, T. T., & Tran, T. (2013). Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. International Health, 5(1), 29-37.
Flood, M., & Pease, B. (2009). Factors influencing attitudes to violence against women. Trauma, violence & abuse, 10(2), 125-142.
Flury, M., Nyberg, E., & Riecher-Rössler, A. (2010). Domestic violence against women: Definitions, epidemiology, risk factors and consequences. Swiss medical weekly, 140, w13099-13027.
Fonagy, P. (1999). Male perpetrators of violence against women: An attachment theory perspective. Journal of Applied Psychoanalytic Studies, 1(1), 7-27.
Fulu, E., Warner, X., Miedema, S., Jewkes, R., Roselli, T., & Lang, J. (2013). Why do some men use violence against women and how can we prevent it? Quantitative findings from the United Nations multi-country study on men and violence in Aisa and the Pacific. Bangkok: UNDP, UNFPA, UN Women and UNV.
Garcia-Moreno, C., Heise, L., Jansen, H. A. F. M., Ellsberg, M., & Watts, C. H. (2005). Violence against women. Science, 310(5752), 1282-1283.
Garcia-Moreno, C., Jansen, H. A. F. M., Ellsberg, M., Heise, L., & Watts, C. H. (2005). WHO multi-country study on women’s health and domestic violence against women: Initial results on prevalence, health outcomes and women’s responses. Geneva: World Health Organization.
Garcia-Moreno, C., Jansen, H. A. F. M., Ellsberg, M., Heise, L., & Watts, C. H. (2006). Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. The Lancet, 368, 1260-1269.
Garcia-Moreno, C., & Watts, C. H. (2011). Violence against women: an urgent public health priority. Bulletin of the World Health Organization, 89(1), 2-2.
Gartland, D., Hemphill, S. A., Hegarty, K., & Brown, S. J. (2011). Intimate Partner Violence During Pregnancy and the First Year Postpartum in an Australian Pregnancy Cohort Study. Maternal and child health journal, 15(5), 570-578.
Gausia, K., Fisher, C., Algin, S., & Oosthuizen, J. (2007). Validation of the Bangla version of the Edinburgh Postnatal Depression Scale for a Bangladeshi sample. JOURNAL OF REPRODUCTIVE AND INFANT PSYCHOLOGY, 25(4), 308-315.
Gausia, K., Fisher, C., Ali, M., & Oosthuizen, J. (2009). Antenatal depression and suicidal ideation among rural Bangladeshi women: a community-based study. Arch Womens Ment Health, 12(5), 351-358.
Gazmararian, J. A., Adams, M. M., Saltzman, L. E., Johnson, C. H., Bruce, F. C., Marks, J. S., & Zahniser, S. C. (1995). The Relationship Between Pregnancy Intendedness and Physical Violence in Mothers of Newborns. Obstetrics & Gynecology, 85(6), 1031-1038.
Gazmararian, J. A., Lazorick, S., Spitz, A. M., Ballard, T. J., Saltzman, L. E., & Marks, J. S. (1996). Prevalence of violence against pregnant women. JAMA: The Journal of the American Medical Association, 275(24), 1915-1920.
Gelles, R. J. (1975). Violence and Pregnancy: A Note on the Extent of the Problem and Needed Services. The Family Coordinator, 24(1), 81-86.
Gelles, R. J. (1988). Violence and pregnancy: are pregnant women at greater risk of abuse? Journal of Marriage and the Family, 841-847.
Glick, P., & Fiske, S. T. (1996). The Ambivalent Sexism Inventory: Differentiating Hostile and Benevolent Sexism. Journal of personality and social psychology, 70(3), 491-512.
Glick, P., & Fiske, S. T. (1997). Hostile and benevolent sexism: Measuring ambivalent sexist attitudes toward women. Psychology of Women Quarterly, 21(1), 119-135.
GOB. (2016). Health Bulletin 2016. Dhaka, Bangladesh: Ministry of Health and Family Welfare, Government of the people’s Republic of Bangladesh.
Godbout, N., Dutton, D. G., Lussier, Y., & Sabourin, S. (2009). Early exposure to violence, domestic violence, attachment representations, and marital adjustment. Personal Relationships, 16(3), 365-384.
Goetz, A. T., Shackelford, T. K., & Camilleri, J. A. (2008). Proximate and ultimate explanations are required for a comprehensive understanding of partner rape. Aggression and Violent Behavior, 13(2), 119-123.
Goetz, A. T., Shackelford, T. K., Romero, G. A., Kaighobadi, F., & Miner, E. J. (2008). Punishment, proprietariness, and paternity: Men’s violence against women from an evolutionary perspective. Aggression and Violent Behavior, 13(6), 481-489.
Gomez-Beloz, A., Williams, M. A., Sanchez, S. E., & Lam, N. (2009). Intimate partner violence and risk for depression among postpartum women in Lima, Peru. Violence and victims, 24(3), 380-398.
Goodwin, M. M., Gazmararian, J. A., Johnson, C. H., Gilbert, B. C., Saltzman, L. E., & Group, P. W. (2000). Pregnancy intendedness and physical abuse around the time of pregnancy: findings from the pregnancy risk assessment monitoring system, 1996–1997. Maternal and child health journal, 4(2), 85-92.
Greiner, T. (2014). Exclusive breastfeeding: measurement and indicators. International Breastfeeding Journal, 9(1), 18-.
Guo, S.-F., Wu, J.-L., Qu, C.-y., & Yan, R.-Y. (2004a). Domestic abuse on women in China before, during, and after pregnancy. Chinese medical journal, 117(3), 331-336.
Guo, S.-F., Wu, J.-L., Qu, C.-y., & Yan, R.-Y. (2004b). Physical and sexual abuse of women before, during, and after pregnancy. International Journal of Gynecology and Obstetrics, 84(3), 281-286.
Gupta, S., Kishore, J., Mala, Y. M., Ramji, S., & Aggarwal, R. (2013). Postpartum depression in North Indian women: Prevalence and risk factors. Journal of Obstetrics and Gynecology of India, 63(4), 223-229.
Hadi, A. (2000). Prevalence and correlates of the risk of marital sexual violence in Bangladesh. J Interpers Violence, 15(8), 787-805.
Hadi, A. (2005). Women’s productive role and marital violence in Bangladesh. Journal of family violence, 20(3), 181-189.
Haj-Yahia, M. M. (1998). Beliefs About Wife Beating Among Palestinian Women: The Influence of Their Patriarchal Ideology. Violence Against Women, 4(5), 533-558.
Hammoury, N., Khawaja, M., Mahfoud, Z., Afifi, R. A., & Madi, H. (2009). Domestic Violence against Women during Pregnancy: The Case of Palestinian Refugees Attending an Antenatal Clinic in Lebanon. Journal of women’s health (2002), 18(3), 337-345.
Han, A., & Stewart, D. E. (2014). Maternal and fetal outcomes of intimate partner violence associated with pregnancy in the Latin American and Caribbean region. International Journal of Gynaecology and Obstetrics, 124(1), 6-11.
Harris, C. R. (2003). A Review of Sex Differences in Sexual Jealousy, Including Self-Report Data, Psychophysiological Responses, Interpersonal Violence, and Morbid Jealousy. Personality and Social Psychology Review, 7(2), 102-128.
Harrykissoon, S. D., Rickert, V. I., & Wiemann, C. M. (2002). Prevalence and Patterns of Intimate Partner Violence Among Adolescent Mothers During the Postpartum Period. Arch Pediatr Adolesc Med, 156(4), 325-330.
Hart, S., Field, T., & Nearing, G. (1998). Depressed mothers’ neonates improve following the MABI and a Brazelton demonstration. Journal of pediatric psychology, 23(6), 351-356.
Hasan, T., Muhaddes, T., Camellia, S., Selim, N., & Rashid, S. F. (2014). Prevalence and Experiences of Intimate Partner Violence Against Women With Disabilities in Bangladesh Results of an Explanatory Sequential Mixed-Method Study. J Interpers Violence, 29(17), 3105-3126.
Haselton, M. G., & Gangestad, S. W. (2006). Conditional expression of women’s desires and men’s mate guarding across the ovulatory cycle. Hormones and Behavior, 49(4), 509-518.
Healey, K., Smith, C., & O’Sullivan, C. (1998). Batterer intervention: Program approaches and criminal justice strategies. USA: U.S. Department of Justice. National Institute of Justice.
Heaman, M. I. (2005). Relationships between physical abuse during pregnancy and risk factors for preterm birth among women in Manitoba. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 34(6), 721-731.
Hedin, L. W. (2000). Postpartum, also a risk period for domestic violence. European Journal of Obstetrics & Gynecology and Reproductive Biology, 89(1), 41-45.
Hegarty, K. (2011). Domestic violence: the hidden epidemic associated with mental illness. the British journal Of psychiatry, 198(3), 169-170.
Heise, L. L. (1998). Violence Against Women: An Integrated, Ecological Framework. Violence Against Women, 4(3), 262-290.
Heise, L. L., & Garcia-Moreno, C. (2002). Violence by intimate partners. Geneva, Switzerland: World Health Organization.
Hellmuth, J. C., Gordon, K. C., Stuart, G. L., & Moore, T. M. (2013). Risk factors for intimate partner violence during pregnancy and postpartum. Arch Womens Ment Health, 16(1), 19-27.
Henderson, A. J. Z., Bartholomew, K., Trinke, S. J., & Kwong, M. J. (2005). When Loving Means Hurting: An Exploration of Attachment and Intimate Abuse In a Community Sample. Journal of family violence, 20(4), 219-230.
Henderson, J. J., Evans, S. F., Straton, J. A. Y., Priest, S. R., & Hagan, R. (2003). Impact of Postnatal Depression on Breastfeeding Duration. Birth, 30(3), 175-180.
Herzog, S. (2007). An empirical test of Feminist Theory and research: The effect of heterogeneous gender-role attitudes on perceptions of intimate partner violence. Feminist Criminology, 2(3), 223-244.
Hoffman, L. W., & Kloska, D. D. (1995). Parents’ gender-based attitudes toward marital roles and child rearing: development and validation of new measures. Sex roles, 32(5-6), 273-295.
Horon, I. L., & Cheng, D. (2005). Underreporting of pregnancy-associated deaths. Am J Public Health, 95(11), 1879.
Horrigan, T. J., Schroeder, A. V., & Schaffer, R. M. (2000). The triad of substance abuse, violence, and depression are interrelated in pregnancy. Journal of Substance Abuse Treatment, 18(1), 55-58.
Hosain, G. M. M., Chatterjee, N., Ara, N., & Islam, T. (2007). Prevalence, pattern and determinants of mental disorders in rural Bangladesh. Public health, 121(1), 18-24.
Houry, D., Kaslow, N. J., & Thompson, M. P. (2005). Depressive Symptoms in Women Experiencing Intimate Partner Violence. J Interpers Violence, 20(11), 1467-1477.
Howard, L. M., Oram, S., Galley, H., Trevillion, K., & Feder, G. (2013). Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS medicine, 10(5), e1001452.
Huth-Bocks, A. C., Levendosky, A. A., & Bogat, G. A. (2002). The effects of domestic violence during pregnancy on maternal and infant health. Violence and victims, 17(2), 169-185.
Hyde-Nolan, M. E., & Juliao, T. (2012). Theoretical basis for family violence. In R. S. Fife & S. Schrage (Eds.), Family violence: What health care providers need to know. Sudbury: Jones & Bartlett Learning.
Ishida, K., Stupp, P., Melian, M., Serbanescu, F., & Goodwin, M. (2010). Exploring the associations between intimate partner violence and women’s mental health: evidence from a population-based study in Paraguay. Social Science & Medicine, 71(9), 1653-1661.
Islam, M. J., Baird, K., Mazerolle, P., & Broidy, L. (2017). Exploring the influence of psychosocial factors on exclusive breastfeeding in Bangladesh. Archives of Women’s Mental Health, 20(1), 173-188.
Islam, M. J., Broidy, L., Baird, K., & Mazerolle, P. (2017). Exploring the associations between intimate partner violence and delayed entry to prenatal care: Evidence from a cross-sectional study in Bangladesh. Midwifery, 47, 43-55.
Islam, T. M., Tareque, M. I., Tiedt, A. D., & Hoque, N. (2014). The intergenerational transmission of intimate partner violence in Bangladesh. Global health action, 7, 23591 doi: 10.3402/gha.v7.23591
Isomaa, R., Vaananen, J.-M., Forojd, S., Kaltiala-Heino, R., & Marttunen, M. (2013). How low is low? Low self-esteem as an indicator of internalizing psychopathology in adolescence. Health Education & Behavior, 40(4), 392-399.
James, J. P., Taft, A., Amir, L. H., & Agius, P. (2014). Does intimate partner violence impact on women’s initiation and duration of breastfeeding? Breastfeeding Review, 22(2), 11-19.
James, L., Brody, D., & Hamilton, Z. (2013). Risk factors for domestic violence during pregnancy: a meta-analytic review. Violence and victims, 28(3), 359-380.
Janssen, P. A., Holt, V. L., Sugg, N. K., Emanuel, I., Critchlow, C. M., & Henderson, A. D. (2003). Intimate partner violence and adverse pregnancy outcomes: A population-based study. American journal of obstetrics and gynecology, 188(5), 1341-1347.
Jasinski, J. L. (2001). Pregnancy and Violence Against Women An Analysis of Longitudinal Data. J Interpers Violence, 16(7), 712-733.
Jasinski, J. L. (2004). Pregnancy and domestic violence: a review of the literature. Trauma, violence & abuse, 5(1), 47-64.
Jasinski, J. L., & Kantor, G. K. (2001). Pregnancy, stress and wife assault: Ethnic differences in prevalence, severity, and onset in a national sample. Violence and victims, 16(3), 219-232.
Jeanjot, I., Barlow, P., & Rozenberg, S. (2008). Domestic violence during pregnancy: survey of patients and healthcare providers. Journal of Women’s Health, 17(4), 557-567.
Jewkes, R. (2002). Intimate partner violence: causes and prevention. The Lancet, 359(9315), 1423-1429.
Jewkes, R., Penn-Kekana, L., Levin, J., Ratsaka, M., & Schrieber, M. (2001). Prevalence of emotional, physical and sexual abuse of women in three South African provinces. South African Medical Journal, 91(5), 421-428.
Johnson, H., Ollus, N., & Nevala, S. (2007). Violence against women: An international perspective. New York: Springer.
Johnsona, R. M., Kotch, J. B., Catellier, D. J., Winsor, J. R., Dufort, V., Hunter, W., & Amaya-Jackson, L. (2002). Adverse behavioral and emotional outcomes from child abuse and witnessed violence. Child maltreatment, 7(3), 179-186.
Kabir, Z. N., Nasreen, H.-E., & Edhborg, M. (2014). Intimate partner violence and its association with maternal depressive symptoms 6–8 months after childbirth in rural Bangladesh. Global health action, 7, 24725
Kamal, S. M. M. (2013). Domestic violence, unwanted pregnancy and pregnancy termination among urban women of Bangladesh. Journal of Family & Reproductive Health, 7(1), 11-22.
Kantor, G. K., & Straus, M. A. (1999). Report on the USAF Family Needs Screener. Durham, NH: Family Research Laboratory.
Karaoglu, L., Celbis, O., Ercan, C., Ilgar, M., Pehlivan, E., Gunes, G., Genc, M. F., & Egri, M. (2005). Physical, emotional and sexual violence during pregnancy in Malatya, Turkey. European journal of public health, 16(2), 149-156.
Karmaliani, R., Irfan, F., Bann, C. M., Mcclure, E. M., Moss, N., Pasha, O., & Goldenberg, R. L. (2008). Domestic violence prior to and during pregnancy among Pakistani women. Acta obstetricia et gynecologica Scandinavica, 87(11), 1194-1201.
Kashif, M., Murtaza, K., & Kirkman, M. (2010). Violence against women during pregnancy in some Asian countries: a review of the literature. Italian Journal of Public Health, 7(2).
Kaye, D. K., Mirembe, F. M., Bantebya, G., Johansson, A., & Ekstrom, A. M. (2006). Domestic violence during pregnancy and risk of low birthweight and maternal complications: a prospective cohort study at Mulago Hospital, Uganda. TROPICAL MEDICINE & INTERNATIONAL HEALTH, 11(10), 1576-1584.
Keeling, J., & Mason, T. (2011). Postnatal disclosure of domestic violence: comparison with disclosure in the first trimester of pregnancy. Journal of Clinical Nursing, 20(1‐2), 103-110.
Kelly, U. A., Gonzalex-Guarda, R. M., & Taylor, J. (2011). Theories of Intimate Partner Violence. In J. Humphreys & J. C. Campbell (Eds.), Family Violence and Nursing Practice (Second ed.). New York: Springer Publishing Company.
Kendall-Tackett, K. A. (2007). Violence against women and the perinatal period: The impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, violence & abuse, 8(3), 344-353.
Khatun, M. T., & Rahman, K. F. (2012). Domestic Violence against Women in Bangladesh: Analysis from a Socio-legal Perspective. Bangladesh e-Journal of Sociology, 9(2), 19-30.
Khosla, A., Dua, D., Devi, L., & Sud, S. (2005). Domestic violence in pregnancy in North Indian women. Indian Journal of Medical Sciences, 59(5), 195-199.
Kidney, E., Winter, H. R., Khan, K. S., Gülmezoglu, A. M., Meads, C. A., Deeks, J. J., & MacArthur, C. (2009). Systematic review of effect of community-level interventions to reduce maternal mortality. BMC Pregnancy Childbirth, 9(1), 2.
Koenig, L. J., Whitaker, D. J., Royce, R. A., Wilson, T. E., Ethier, K., & Fernandez, M. I. (2006). Physical and sexual violence during pregnancy and after delivery: A prospective multistate study of women with or at risk for HIV infection. Am J Public Health, 96(6), 1052-1059.
Koenig, M. A., Ahmed, S., Hossain, M. B., & Mozumder, A. K. A. (2003). Women’s status and domestic violence in rural Bangladesh: individual-and community-level effects. Demography, 40(2), 269-288.
Koenig, M. A., Jamil, K., Streatfield, P. K., Saha, T., Al-Sabir, A., Arifeen, S. E., Hill, K., & Haque, Y. (2007). Maternal health and care-seeking behavior in Bangladesh: findings from a national survey. International family planning perspectives, 33(2), 75-82.
Koenig, M. A., Stephenson, R., Ahmed, S., Jejeebhoy, S. J., & Campbell, J. (2006). Individual and contextual determinants of domestic violence in North India. Am J Public Health, 96(1), 132.
Koski, A. D., Stephenson, R., & Koenig, M. R. (2011). Physical violence by partner during pregnancy and use of prenatal care in rural India. J Health Popul Nutr, 29(3), 245.
Kovacs, K., & Tomison, A. (2003). An Analysis of Current Australian Program Initiatives for Children Exposed to Domestic Violence. Australian Journal of Social Issues, The, 38(4), 513-540.
Krantz, G. (2002). Violence against women: a global public health issue! Journal of epidemiology and community health, 56(4), 242-243.
Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., & Lozano, R. (Eds.). (2002). World health report on violence and health. Geneva, Switzerland: World Health Organization.
Krug, E. G., Mercy, J. A., Dahlberg, L. L., & Zwi, A. B. (2002). The world report on violence and health. The Lancet, 360(9339), 1083-1088.
Kwagala, B., Wandera, S. O., Ndugga, P., & Kabagenyi, A. (2013). Empowerment, partner’s behaviours and intimate partner physical violence among married women in Uganda. BMC Public Health, 13(1), 1112-1112.
Lau, Y. (2005). Does pregnancy provide immunity from intimate partner abuse among Hong Kong Chinese women? Social Science & Medicine, 61(2), 365-377.
Lau, Y., & Chan, K. S. (2007). Influence of Intimate Partner Violence During Pregnancy and Early Postpartum Depressive Symptoms on Breastfeeding Among Chinese Women in Hong Kong. Journal of Midwifery and Women’s Health, 52(2), e15-e20.
Lawson, J. (2012). Sociological Theories of Intimate Partner Violence. Journal of Human Behavior in the Social Environment, 22(5), 572-590.
Leneghan, S., Gillen, P., & Sinclair, M. (2012). Interventions to reduce Domestic Abuse in Pregnancy: a Qualitative Systematic Review. Evidence Based Midwifery, 10(4), 137-142.
Leung, W. C., Leung, T. W., Lam, Y. Y. J., & Ho, P. C. (1999). The prevalence of domestic violence against pregnant women in a Chinese community: Social issues in reproductive health. International Journal of Gynecology & Obstetrics, 66(1), 23-30.
Lewis, S. F., & Fremouw, W. (2001). Dating violence: a critical review of the literature. Clinical psychology review, 21(1), 105-127.
Liou, S.-R., Wang, P., & Cheng, C.-Y. (2014). Longitudinal study of perinatal maternal stress, depressive symptoms and anxiety. Midwifery, 30(6), 795-801.
Lipsky, S., Holt, V. L., Easterling, T. R., & Critchlow, C. W. (2005). Police-reported intimate partner violence during pregnancy: who is at risk? Violence and victims, 20(1), 69-86.
Loft Abadi, M. N., Ghazinour, M., Nojomi, M., & Richter, J. (2012). The buffering effect of social support between domestic violence and self-esteem in pregnant women in Tehran, Iran. Journal of family violence, 27(3), 225-231.
Loue, S. (2001). Intimate partner violence: societal, medical, legal, and individual responses. New York: Kluwer Academic/Plenum Publishers.
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: a meta-analytic review. Clinical psychology review, 20(5), 561-592.
Ludermir, A. B., Valongueiro, S., & Araújo, T. V. B. d. (2014). Common mental disorders and intimate partner violence in pregnancy. Revista de Saúde Pública, 48(1), 29-35.
Macy, R. J., Martin, S. L., Kupper, L. L., Casanueva, C., & Guo, S. (2007). Partner violence among women before, during, and after pregnancy: multiple opportunities for intervention. Women’s health issues, 17(5), 290-299.
Malyadri, P. (2013). Domestic Violence against Women: Strategical remedies for its Causes and Consequences. International Journal of Information, Business and Management, 5(1), 97-108.
Maner, J. K., & Shackelford, T. K. (2008). The basic cognition of jealousy: an evolutionary perspective. European Journal of Personality, 22(1), 31-36.
Martin, K. R., & Garcia, L. (2011). Unintended Pregnancy and Intimate Partner Violence Before and During Pregnancy Among Latina Women in Los Angeles, California. J Interpers Violence, 26(6), 1157-1175.
Martin, S. L., Harris-Britt, A., Li, Y., Moracco, K. E., Kupper, L. L., & Campbell, J. C. (2004). Changes in intimate partner violence during pregnancy. Journal of family violence, 19(4), 201-210.
Martin, S. L., Li, Y., Casanueva, C., Britt, A. H., & Kupper, L. L. (2006). Intimate Partner Violence and Women’s Depression Before and During Pregnancy. Violence Against Women, 12(3), 221.
Martin, S. L., Mackie, L., Kupper, L. L., Buescher, P. A., & Moracco, K. E. (2001). Physical abuse of women before, during, and after pregnancy. Jama, 285(12), 1581-1584.
Massachusetts Coalition of Battered Women Service Groups. (1995). Children of domestic violence (Working report of the Children’s Working Group). Boston.
Mazerolle, P. (2007). The Role of Theory. In H. Hayes & T. Prenzler (Eds.), An introduction to crime (pp. 166-180). Frenchs Forest, N.S.W: Pearson/Prentice Hall.
McCloskey, L. A., Williams, C. M., Lichter, E., Gerber, M., Ganz, M. L., & Sege, R. (2007). Abused Women Disclose Partner Interference with Health Care: An Unrecognized Form of Battering. Journal of General Internal Medicine, 22(8), 1067-1072.
McFarlane, J., Campbell, J. C., Sharps, P., & Watson, K. (2002). Abuse during pregnancy and femicide: urgent implications for women’s health. Obstetrics & Gynecology, 100(1), 27-36.
McFarlane, J., Parker, B., & Soeken, K. (1995). Abuse during pregnancy: Frequency, severity, perpetrator, and risk factors of homicide. Public Health Nursing, 12(5), 284-289.
McHugh, M. C., & Frieze, I. H. (1997). The measurement of gender-role attitudes. Psychology of Women Quarterly, 21(1), 1.
McMahon, S., & Armstrong, D. e. Y. (2012). Intimate Partner Violence during Pregnancy: Best Practices for Social Workers. Health & social work, 37(1), 9-17.
Mechanic, M. B., Weaver, T. L., & Resick, P. A. (2008). Mental health consequences of intimate partner abuse a multidimensional assessment of four different forms of abuse. Violence Against Women, 14(6), 634-654.
Mercedes, M., & Lafaurie, V. (2015). Intimate partner violence against women during pregnancy: a critical reading from a gender perspective. Revista Colombiana de Enfermerıa, 10(10), 64-77.
Mezey, G. C., & Bewley, S. (1997). Domestic violence and pregnancy. BJOG: An International Journal of Obstetrics & Gynaecology, 104(5), 528-531.
Mihalic, S. W., & Elliott, D. (1997). A social learning theory model of marital violence. Journal of family violence, 12(1), 21-47.
Miller, S. L. (1994). Expanding the boundaries: toward a more inclusive and integrated study of intimate violence. Violence and victims, 9(2), 183-194.
Misch, E. S., & Yount, K. M. (2014). Intimate partner violence and breastfeeding in Africa. Maternal and child health journal, 18(3), 688-697.
Mohammadhosseini, E., Sahraean, L., & Bahrami, T. (2010). Domestic abuse before, during and after pregnancy in Jahrom, Islamic Republic of Iran. Eastern Mediterranean Health Journal, 16(7), 752-758.
Mollah, A. H. (2005). Combating violence against women in South Asia: An overview of Bangladesh: UNPAN.
Moodley, P., & Sturm, A. W. (2000). Sexually transmitted infections, adverse pregnancy outcome and neonatal infection. Seminars in neonatology, 5(3), 255-269.
Moraes, C. L., Arana, F. D. N., & Reichenheim, M. E. (2010). Physical intimate partner violence during gestation as a risk factor for low quality of prenatal care. Revista de Saúde Pública, 44(4), 667-676.
Moraes, C. L., da Silva, T. d. S. T., Reichenheim, M. E., Azevedo, G. L., Oliveira, A. S. D., & Braga, J. U. (2011). Physical violence between intimate partners during pregnancy and postpartum: a prediction model for use in primary health care facilities. Paediatric and perinatal epidemiology, 25(5), 478-486.
Moraes, C. L., Oliveira, A. S. D., Reichenheim, M. E., & Azevedo, G. L. (2011). Severe physical violence between intimate partners during pregnancy: a risk factor for early cessation of exclusive breast-feeding. Public health nutrition, 14(12), 2148-2155.
Morash, M., Bui, H., Zhang, Y., & Holtfreter, K. (2007). Risk Factors for Abusive Relationships A Study of Vietnamese American Immigrant Women. Violence Against Women, 13(7), 653-675.
Muhajarine, N., & D’Arcy, C. (1999). Physical abuse during pregnancy: prevalence and risk factors. Canadian Medical Association Journal, 160(7), 1007-1011.
Murphy, C. C., Schei, B., Myhr, T. L., & Du Mont, J. (2001). Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. Canadian Medical Association Journal, 164(11), 1567-1572.
Murphy, S. B., & Ouimet, L. V. (2008). Intimate partner violence: a call for social work action. Health & social work, 33(4), 309-314.
Murray, L., Fiori‐Cowley, A., Hooper, R., & Cooper, P. (1996). The impact of postnatal depression and associated adversity on early mother‐infant interactions and later infant outcome. Child development, 67(5), 2512-2526.
Muthal-Rathore, A., Tripathi, R., & Arora, R. (2002). Domestic violence against pregnant women interviewed at a hospital in New Delhi. International Journal of Gynecology and Obstetrics, 76(1), 83-85.
Nasir, K., & Hyder, A. A. (2003). Violence against pregnant women in developing countries: review of evidence. The European Journal of Public Health, 13(2), 105-107.
National Center for Injury Prevention and Control. (2003). Costs of intimate partner violence against women in the United States. Atlanta, Georgia: Centers for Disease Control and Prevention.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International. (2009). Bangladesh Demographic and Health Survey 2007. Dhaka, Bangladesh and Calverton, Maryland, USA: NIPORT, Mitra and Associates, and Macro International.
Navaneetham, K., & Dharmalingam, A. (2002). Utilization of maternal health care services in Southern India. Social Science & Medicine, 55(10), 1849-1869.
Naved, R. T. (2013). Sexual violence towards married women in Bangladesh. Archives of Sexual Behavior, 42(4), 595-602.
Naved, R. T., & Akhtar, N. (2008). Spousal violence against women and suicidal ideation in Bangladesh. Women’s health issues, 18(6), 442-452.
Naved, R. T., Azim, S., Bhuiya, A., & Persson, L. Å. (2006). Physical violence by husbands: magnitude, disclosure and help-seeking behavior of women in Bangladesh. Social Science & Medicine, 62(12), 2917-2929.
Naved, R. T., & Persson, L. A. (2008). Factors associated with physical violence against pregnant women in Bangladesh. International family planning perspectives, 34(2), 71-78.
Naved, R. T., & Persson, L. A. (2010). Dowry and Spousal Physical Violence Against Women in Bangladesh. Journal of Family Issues, 31(6), 830-856.
Naved, R. T., & Persson, L. Å. (2005). Factors associated with spousal physical violence against women in Bangladesh. Stud Fam Plann, 36(4), 289-300.
Noel, N. L., & Yam, M. (1992). Domestic violence. The pregnant battered women. The Nursing clinics of North America, 27(4), 871-884.
Nur, N. (2012). The Effect of Intimate Partner Violence on Mental Health Status Among Women of Reproductive Ages: A Population-Based Study in a Middle Anatolian City. J Interpers Violence, 27(16), 3236-3251.
Nurius, P. S., Macy, R. J., Bhuyan, R., Holt, V. L., Kernic, M. A., & Rivara, F. P. (2003). Contextualizing depression and physical functioning in battered women: adding vulnerability and resources to the analysis. J Interpers Violence, 18(12), 1411-1431.
O’Neill, D. (1998). A Post-Structuralist Review of the Theoretical Literature Surrounding Wife Abuse. Violence Against Women, 4(4), 457-490.
Odhikar. (2014). Human Rights Report 2013: Odhikar Report on Bangladesh. Dhaka, Bangladesh.
Ogbonnaya, I. N., Kupper, L. L., Martin, S. L., Macy, R. J., & Bledsoe-Mansori, S. E. (2013). Intimate partner violence and depressive symptoms before pregnancy, during pregnancy, and after infant delivery: an exploratory study. J Interpers Violence, 28(10), 2112-2133.
Okenwa, L., Lawoko, S., & Jansson, B. (2011). Contraception, reproductive health and pregnancy outcomes among women exposed to intimate partner violence in Nigeria. The European Journal of Contraception and Reproductive Health Care, 16(1), 18-25.
Okenwa, L. E., Lawoko, S., & Jansson, B. (2009). Exposure to intimate partner violence amongst women of reproductive age in Lagos, Nigeria: Prevalence and predictors. Journal of family violence, 24(7), 517-530.
Pallant, J. (2007). SPSS survival manual: a step by step guide to data analysis using SPSS for Windows (Version 15) (3rd ed.). Crows Nest, N.S.W., Australia: Allen & Unwin.
Pallitto, C. C., Campbell, J. C., & O’campo, P. (2005). Is intimate partner violence associated with unintended pregnancy? A review of the literature. Trauma, violence & abuse, 6(3), 217-235.
Pallitto, C. C., García-Moreno, C., Jansen, H. A., Heise, L., Ellsberg, M., & Watts, C. (2013). Intimate partner violence, abortion, and unintended pregnancy: Results from the WHO Multi-country Study on Women’s Health and Domestic Violence. International Journal of Gynecology & Obstetrics, 120(1), 3-9.
Pallitto, C. C., & O’Campo, P. (2005). Community level effects of gender inequality on intimate partner violence and unintended pregnancy in Colombia: testing the feminist perspective. Social Science & Medicine, 60(10), 2205-2216.
Parker, B., & McFarlane, J. (1991). Identifying and helping battered pregnant women. The American Journal of Maternal and Child Nursing, 16(3), 161-164.
Paul, B. K., & Rumsey, D. J. (2002). Utilization of health facilities and trained birth attendants for childbirth in rural Bangladesh: an empirical study. Social Science & Medicine, 54(12), 1755-1765.
Peedicayil, A., Sadowski, L. S., Jeyaseelan, L., Shankar, V., Jain, D., Suresh, S., & Bangdiwala, S. I. (2004). Spousal physical violence against women during pregnancy. BJOG: An International Journal of Obstetrics & Gynaecology, 111(7), 682-687.
Peek-Asa, C., Wallis, A., Harland, K., Beyer, K., Dickey, P., & Saftlas, A. (2011). Rural Disparity in Domestic Violence Prevalence and Access to Resources. Journal of women’s health (2002), 20(11), 1743-1749.
Perales, M. T., Cripe, S. M., Lam, N., Sanchez, S. E., Sanchez, E., & Williams, M. A. (2009). Prevalence, types, and pattern of intimate partner violence among pregnant women in Lima, Peru. Violence Against Women, 15(2), 224-250.
Pico-Alfonso, M. A., Garcia-Linares, M. I., Celda-Navarro, N., Blasco-Ros, C., Echeburúa, E., & Martinez, M. (2006). The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. Journal of Women’s Health, 15(5), 599-611.
Plichta, S. B. (2004). Intimate partner violence and physical health consequences: policy and practice implications. J Interpers Violence, 19(11), 1296-1323.
Portwood, S. G., & Heany, J. F. (2007). Responding to violence against women: Social science contributions to legal solutions. International journal of law and psychiatry, 30(3), 237-247.
Pulido, M. L. (2001). Pregnancy: A time to break the cycle of family violence. Health & social work, 26(2), 120-124.
Rachana, C., Suraiya, K., Hisham, A.-S., Abdulaziz, A.-M., & Hai, A. (2002). Prevalence and complications of physical violence during pregnancy. European Journal of Obstetrics and Gynecology, 103(1), 26-29.
Rådestad, I., Rubertsson, C., Ebeling, M., & Hildingsson, I. (2004). What factors in early pregnancy indicate that the mother will be hit by her partner during the year after childbirth? A nationwide Swedish survey. Birth, 31(2), 84-92.
Rahman, M. (2012). Women’s Autonomy and Unintended Pregnancy Among Currently Pregnant Women in Bangladesh. Maternal and child health journal, 16(6), 1206-1214.
Rahman, M., Nakamura, K., Seino, K., & Kizuki, M. (2012). Intimate partner violence and use of reproductive health services among married women: evidence from a national Bangladeshi sample. BMC Public Health, 12, 913.
Rahman, M. H., Mosley, W. H., Ahmed, S., & Akhter, H. H. (2008). Does service accessibility reduce socioeconomic differentials in maternity care seeking? Evidence from rural Bangladesh. J Biosoc Sci, 40(1), 19-33.
Rai, R. K., Singh, P. K., Singh, L., & Kumar, C. (2014). Individual Characteristics and Use of Maternal and Child Health Services by Adolescent Mothers in Niger. Maternal and child health journal, 18(3), 592-603.
Raihana, S., Shaheen, R., & Rahman, M. S. (2012). Influence of Intimate Partners’ Violence on Unintended Pregnancy in Bangladesh. International Journal of Psychology and Behavioral Sciences, 2(5), 159-166.
Rani, M., & Bonu, S. (2009). Attitudes toward wife beating: A cross-country study in Asia. J Interpers Violence, 24(8), 1371-1397.
Rashid, M., Kader, M., Perera, N. K. P., & Sharma, A. (2014). Wife beating: A population-based study in Bangladesh. VIOLENCE AND GENDER, 1(4).
Reichenheim, M. E., Moraes, C. L., Lopes, C. S., & Lobato, G. (2014). The role of intimate partner violence and other health-related social factors on postpartum common mental disorders: a survey-based structural equation modeling analysis. BMC Public Health, 14(1), 427-427.
Renker, P. R., & Tonkin, P. (2006). Women’s Views of Prenatal Violence Screening: Acceptability and Confidentiality Issues. Obstetrics & Gynecology, 107(2, Part 1), 348-354.
Renzetti, C. M. (2004). Feminist theories of violent behavior. In M. A. Zahn, H. H. Brownstein & S. L. Jackson (Eds.), Violence: From Theory to Research (pp. 131-143). Newark: NJ: LexisNexis Anderson Publishing.
Richardson, J., Coid, J., Petruckevitch, A., Chung, W. S., Moorey, S., & Feder, G. (2002). Identifying domestic violence: cross sectional study in primary care. BMJ: British Medical Journal, 324(7332), 274.
Riger, S., Raja, S., & Camacho, J. (2002). The radiating impact of intimate partner violence. J Interpers Violence, 17(2), 184-205.
Riggs, D. S., & O’Leary, K. D. (1989). A theoretical model of courtship aggression. In M. A. Pirog-Good & J. E. Stets (Eds.), Violence in dating relationships: Emerging social issues (pp. 53-71). New York: Praeger Publishers.
Rodriguez, M. A., Heilemann, M. V., Fielder, E., Ang, A., Nevarez, F., & Mangione, C. M. (2008). Intimate partner violence, depression, and PTSD among pregnant Latina women. Annals of family medicine, 6(1), 44-52.
Romito, P., Molzan Turan, J., & De Marchi, M. (2005). The impact of current and past interpersonal violence on women’s mental health. Social Science & Medicine, 60(8), 1717-1727.
Romito, P., Pomicino, L., Lucchetta, C., Scrimin, F., & Molzan Turan, J. (2009). The relationships between physical violence, verbal abuse and women’s psychological distress during the postpartum period. Journal of Psychosomatic Obstetrics & Gynecology, 30(2), 115-121.
Ronsmans, C., Scott, S., Qomariyah, S., Achadi, E., Braunholtz, D., Marshall, T., Pambudi, E., Witten, K., & Graham, W. (2009). Professional assistance during birth and maternal mortality in two Indonesian districts. Bulletin of the World Health Organization, 87(6), 416-423.
Rosenberg, M. (1965). Society and the adolescent self-image. Princeton, N.J Princeton University Press.
Ruiz-Pérez, I., Plazaola-Castaño, J., Álvarez-Kindelán, M., Palomo-Pinto, M., Arnalte-Barrera, M., Bonet-Pla, Á., De Santiago-Hernando, M. L., Herranz-Torrubiano, A., & Garralón-Ruiz, L. M. (2006). Sociodemographic Associations of Physical, Emotional, and Sexual Intimate Partner Violence in Spanish Women. Annals of Epidemiology, 16(5), 357-363.
Sagrestano, L. M., Carroll, D., Rodriguez, A. C., & Nuwayhid, B. (2004). Demographic, psychological, and relationship factors in domestic violence during pregnancy in a sample of low-income women of color. Psychology of Women Quarterly, 28(4), 309-322.
Saito, A., Creedy, D., Cooke, M., & Chaboyer, W. (2012). Effect of intimate partner violence on postpartum women’s health in northeastern Thailand. Nursing & health sciences, 14(3), 345-351.
Salam, M. A., Alim, M. A., & Noguchi, T. (2006). Spousal abuse against women and its consequences on reproductive health: a study in the urban slums in Bangladesh. Maternal and child health journal, 10(1), 83-94.
Salari, S. M., & Baldwin, B. M. (2002). Verbal, physical, and injurious aggression among intimate couples over time. Journal of Family Issues, 23(4), 523-550.
Salari, Z., & Nakhaee, N. (2008). Identifying types of domestic violence and its associated risk factors in a pregnant population in Kerman Hospitals, Iran Republic. Asia-Pacific Journal of Public Health, 20(1), 49-55.
Salomon, A. M. Y., Bassuk, S. S., & Browne, A. (1999). The Impact of Recent Partner Violence on Poor Women’s Capacity to Maintain Work. Violence Against Women, 5(4), 393-426.
Saltzman, L. E., Johnson, C. H., Gilbert, B. C., & Goodwin, M. M. (2003). Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Maternal and child health journal, 7(1), 31-43.
Sambisa, W., Angeles, G., Lance, P. M., Naved, R. T., Thornton, J., & Curtis, S. L. (2010). Physical and sexual abuse of wives in urban Bangladesh: husbands’ reports. Stud Fam Plann, 41(3), 165-178.
Sarkar, N. (2008). The impact of intimate partner violence on women’s reproductive health and pregnancy outcome. Journal of Obstetrics & Gynecology, 28(3), 266-271.
Schuler, S. R., Bates, L. M., & Islam, F. (2008). Women’s rights, domestic violence, and recourse seeking in rural Bangladesh. Violence Against Women, 14(3), 326-345.
Schuler, S. R., & Islam, F. (2008). Women’s acceptance of intimate partner violence within marriage in rural Bangladesh. Stud Fam Plann, 39(1), 49-58.
Scribano, P. V., Stevens, J., & Kaizar, E. (2013). The effects of intimate partner violence before, during, and after pregnancy in nurse visited first time mothers. Maternal and child health journal, 17(2), 307-318.
Shadigian, E. M., & Bauer, S. T. (2004). Screening for partner violence during pregnancy. International Journal of Gynaecology and Obstetrics, 84(3), 273-280.
Shah, P. S., & Shah, J. (2010). Maternal exposure to domestic violence and pregnancy and birth outcomes: a systematic review and meta-analyses. Journal of Women’s Health, 19(11), 2017-2031.
Shamu, S., Abrahams, N., Temmerman, M., Musekiwa, A., & Zarowsky, C. (2011). A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One, 6(3), e17591.
Sharps, P. W., Laughon, K., & Giangrande, S. K. (2007). Intimate partner violence and the childbearing year: maternal and infant health consequences. Trauma, Violence and Abuse, 8(2), 105-116.
Silva, E. P., Ludermir, A. B., de Araujo, T. V. B., & Valongueiro, S. A. (2011). Frequency and pattern of intimate partner violence before, during and after pregnancy. Revista de Saúde Pública, 45(6), 1044-1053.
Silva, E. P., Valongueiro, S., Araújo, T. V. B. d., & Ludermir, A. B. (2015). Incidence and risk factors for intimate partner violence during the postpartum period. Revista de Saúde Pública, 49, 1-9.
Silverman, J. G., Gupta, J., Decker, M. R., Kapur, N., & Raj, A. (2007). Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. BJOG: An International Journal of Obstetrics & Gynaecology, 114(10), 1246-1252.
Smith, M., & Martin, F. (1995). Domestic violence: recognition, intervention, and prevention. Medsurg nursing: official journal of the Academy of Medical-Surgical Nurses, 4(1), 21-25.
Smith, M. D. (1990). Patriarchal ideology and wife beating: a test of a feminist hypothesis. Violence and victims, 5(4), 257-273.
Solotaroff, J. L., & Pande, R. P. (2014). Violence against women and girls : lessons from South Asia (W. Bank Ed.). Washington, DC: The World Bank.
Srinivasan, S., & Bedi, A. S. (2007). Domestic violence and dowry: Evidence from a South Indian village. World Development, 35(5), 857-880.
Stark, E. (2007). Coercive Control : How Men Entrap Women in Personal Life. Oxford: Oxford University Press, New York; Oxford.
Stenson, K. (2004). Men’s Violence against Women–a Challenge in Antenatal Care. (Doctor of Philosophy Ph.D Dissertation), Uppsala University, Uppsala, Sweden.
Stephenson, R., Koenig, M. A., & Ahmed, S. (2006). Domestic violence and symptoms of gynecologic morbidity among women in North India. International family planning perspectives, 32(4), 201-208.
Stewart, R. C. (2007). Maternal depression and infant growth: a review of recent evidence. Matern Child Nutr, 3(2), 94-107.
Straus, M. A., Gelles, R. J., & Steinmetz, S. K. (1980). Behind closed doors: violence in the American family. New York: Anchor Press/Doubleday.
Sugarman, D. B., & Frankel, S. L. (1996). Patriarchal ideology and wife assault: A meta-analytic review. Journal of family violence, 11(1), 13-40.
Tabachnick, B. G., & Fidell, L. S. (2013). Using multivariate statistics. Boston: Pearson.
Taggart, L., & Mattson, S. (1996). Delay in prenatal care as a result of battering in pregnancy: Cross‐cultural implications. Health care for women international, 17(1), 25-34.
Taher, M. A., Islam, M. R., Chowdhury, M. A. M., & Siddiqua, S. (2014). Combating dowry violence against women in Bangladesh: A critical study. International Journal of Innovation and Applied Studies, 8(3), 1126-1131.
Taillieu, T. L., & Brownridge, D. A. (2010). Violence against pregnant women: Prevalence, patterns, risk factors, theories, and directions for future research. Aggression and Violent Behavior, 15(1), 14-35.
Taveras, E. M., Capra, A. M., Braveman, P. A., Jensvold, N. G., Escobar, G. J., & Lieu, T. A. (2003). Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics, 112(1), 108-115.
Taylor, R., & Nabors, E. L. (2009). Pink or blue… black and blue? Examining pregnancy as a predictor of intimate partner violence and femicide. Violence Against Women, 15(11), 1273-1293.
Thananowan, N. (2008). Intimate partner violence (IPV), risk Factors, and health outcomes in adult pregnant women. Thai Journal of Nursing Research, 12(4), 310-323.
Thananowan, N., & Heidrich, S. M. (2008). Intimate partner violence among pregnant Thai women. Violence Against Women, 14(5), 509-527.
The Participation and Quality of Life Tool-Kit. (2016). Rosenberg Self-Esteem Scale. Retrieved 12 December, 2016, from http://www.parqol.com/page.cfm?id=142
Thompson, R., Briggs, E., English, D. J., Dubowitz, H., Lee, L.-C., Brody, K., Everson, M. D., & Hunter, W. M. (2005). Suicidal ideation among 8-year-olds who are maltreated and at risk: findings from the LONGSCAN studies. Child maltreatment, 10(1), 26-36.
Tiwari, A., Chan, K., Fong, D., Leung, W., Brownridge, D., Lam, H., Wong, B., Lam, C., Chau, F., Chan, A., Cheung, K., & Ho, P. (2008). The impact of psychological abuse by an intimate partner on the mental health of pregnant women. BJOG: An International Journal of Obstetrics & Gynaecology, 115(3), 377-384.
Tjaden, P., & Thoennes, N. (2000). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women: Findings From the National Violence Against Women Survey: Research Report: National Institute of Justice Washington, DC.
Trabold, N., Waldrop, D. P., Nochajski, T. H., & Cerulli, C. (2013). An exploratory analysis of intimate partner violence and postpartum depression in an impoverished urban population. Social work in health care, 52(4), 332-350.
Uddin, M. K., Islam, M. T., & Asaduzzaman, M. (2012). Perceived Stress and Self-Esteem as Significant Predictors of Cigarette Smoking Behavior of Bangladeshi Male Adults. Journal of Behavioural Sciences, 22(2), 26.
UNFPA. (2003). Male attitude toward violence against women in Bangladesh. Dhaka, Bangladesh.
United Nations Children’s Fund (UNICEF). (2011). A perspective on gender equality in Bangladesh: From young girl to adolescent: what is lost in transition? Dhaka: UNICEF, Bangladesh.
United Nations Development Programme (UNDP). (2015). Human Development Report 2015. NY, USA: UNDP.
Uthman, O. A., Moradi, T., & Lawoko, S. (2009). The independent contribution of individual-, neighbourhood-, and country-level socioeconomic position on attitudes towards intimate partner violence against women in sub-Saharan Africa: a multilevel model of direct and moderating effects. Social Science & Medicine, 68(10), 1801-1809.
Valladares, E., Ellsberg, M., Peña, R., Högberg, U., & Persson, L. A. (2002). Physical partner abuse during pregnancy: a risk factor for low birth weight in Nicaragua. Obstetrics & Gynecology, 100(4), 700-705.
Valladares, E., Peña, R., Ellsberg, M., Persson, L. A., & Högberg, U. (2009). Neuroendocrine response to violence during pregnancy–impact on duration of pregnancy and fetal growth. Acta obstetricia et gynecologica Scandinavica, 88, 818-823.
Valladares, E., Pena, R., Persson, L. A., & Hogberg, U. (2005). Violence against pregnant women: prevalence and characteristics. A population-based study in Nicaragua. BJOG: An International Journal of Obstetrics & Gynaecology, 112(9), 1243-1248.
Van Parys, A.-S., Deschepper, E., Michielsen, K., Temmerman, M., & Verstraelen, H. (2014). Prevalence and evolution of intimate partner violence before and during pregnancy: a cross-sectional study. BMC Pregnancy Childbirth, 14(1), 294.
Van Parys, A.-S., Verhamme, A., Temmerman, M., & Verstraelen, H. (2014). Intimate Partner Violence and Pregnancy: A Systematic Review of Interventions. PLoS One, 9(1).
Varma, D., Chandra, P. S., Thomas, T., & Carey, M. P. (2007). Intimate partner violence and sexual coercion among pregnant women in India: Relationship with depression and post-traumatic stress disorder. Journal of affective disorders, 102(1), 227-235.
W.W. Norton and Company. (2016). Rosenberg Self-Esteem Scale. Retrieved 12 December, 2016, from http://www.wwnorton.com/college/psych/psychsci/media/rosenberg.htm
Wachs, T. D., Black, M. M., & Engle, P. L. (2009). Maternal Depression: A Global Threat to Children’s Health, Development, and Behavior and to Human Rights. CHILD DEVELOPMENT PERSPECTIVES, 3(1), 51-59.
Walker, L. E. (2009). The battered woman syndrome: with research associates. New York: Springer Pub. Co.
Walker, L. E., & Browne, A. (1985). Gender and victimization by intimates. Journal of personality, 53(2), 179-195.
Wallenborn, J., & Masho, S. (2015). Intimate Partner Violence and the Effects on Breastfeeding Outcomes. Journal of Women’s Health, 24(4), 47-47.
Watts, C., & Zimmerman, C. (2002). Violence against women: global scope and magnitude. The Lancet, 359(9313), 1232-1237.
Weinberg, M. K., & Tronick, E. Z. (1998). Emotional characteristics of infants associated with maternal depression and anxiety. Pediatrics, 102(Supplement E1), 1298-1304.
WHO. (2001). Putting Women First: Ethical and Safety Recommendations for Research on Domestic Violence against Women WHO/FCH/GWH/01.1. Geneva, Switzerland: World Health Organization.
WHO. (2004). The economic dimensions of interpersonal violence. Geneva: World Health Organization.
WHO. (2006). Gender based violence in the Western Pacific region: A hidden epidemic? Geneva, Switzerland: World Health Organization.
WHO. (2008). Indicators for assessing infant and young child feeding practices: part 1 definitions. Geneva: WHO.
WHO. (2011). Intimate partner violence during pregnancy: information sheet. WHO/RHR/11.35. Retrieved 13 January 2015, from www.who.int/reproductivehealth.WHO_RHR_11.35_eng.pdf
WHO. (2014a). Trends in Maternal Mortality: 1990 to 2013. Geneva: WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division.
WHO. (2014b). WHO recommendations on postnatal care of the mother and newborn. Geneva: WHO.
Wiemann, C. M., Agurcia, C. A., Berenson, A. B., Volk, R. J., & Rickert, V. I. (2000). Pregnant adolescents: experiences and behaviors associated with physical assault by an intimate partner. Maternal and child health journal, 4(2), 93-101.
Wikipedia. (2014). Administrative geography of Bangladesh. Retrieved 27 October 2014, from http://en.wikipedia.org/wiki/Administrative_geography_of_Bangladesh
Willis, C. E., Hallinan, M. N., & Melby, J. (1996). Effects of sex role stereotyping among European American students on domestic violence culpability attributions. Sex roles, 34(7-8), 475.
Wilson, M. I., & Daly, M. (1996). Male sexual proprietariness and violence against wives. Current Directions in Psychological Science, 2-7.
Woodin, E. M., & O’Leary, K. D. (2009). Theoretical approaches to the etiology of partner violence. In D. J. Whitaker & J. R. Lutzker (Eds.), Preventing partner violence: Research and evidence-based intervention strategies (pp. 41-65). Washington, DC, US: American Psychological Association.
Woolhouse, H., Gartland, D., Hegarty, K., Donath, S., & Brown, S. J. (2012). Depressive symptoms and intimate partner violence in the 12 months after childbirth: a prospective pregnancy cohort study. BJOG, 119(3), 315-323.
World Health Organization (WHO), & Pan American Health Organization (PAHO). (2012). Understanding and addressing violence against women. Geneva: WHO & PAHO.
Yllo, K. (2005). Through a feminist lens gender, diversity and violence: Extending the feminist framework. In D. R. Loseke, R. J. Gelles & M. M. Cavanaugh (Eds.), Current controversies on family violence. Thousand Oaks, CA: Sage Publications.
Yllo, K., & Straus, M. A. (1990). Patriarchy and violence against wives: The impact of structural and normative factors. In M. A. Straus & R. J. Gelles (Eds.), Physical violence in American families (pp. 383-399). London: Transaction.
Yoshihama, M., Horrocks, J., & Kamano, S. (2009). The role of emotional abuse in intimate partner violence and health among women in Yokohama, Japan. Am J Public Health, 99(4), 647.
Yost, N. P., Bloom, S. L., McIntire, D. D., & Leveno, K. J. (2005). A prospective observational study of domestic violence during pregnancy. Obstetrics & Gynecology, 106(1), 61-65.
Zhu, Y., & Dalal, K. (2010). Childhood exposure to domestic violence and attitude towards wife beating in adult life: A study of men in India. J Biosoc Sci, 42(02), 255-269.
Zlotnick, C., Johnson, D. M., & Kohn, R. (2006). Intimate Partner Violence and Long-Term Psychosocial Functioning in a National Sample of American Women. J Interpers Violence, 21(2), 262-275.
Zureick-Brown, S., Lavilla, K., & Yount, K. M. (2013). Intimate partner violence and infant feeding practices in India: A cross-sectional study. Maternal and Child Nutrition, 11(4), 792 – 802.
[1] The most common terminologies used to indicate IPV includes domestic violence/abuse, gender based violence, violence against women, family violence, spouse/partner violence, spousal abuse/assault, wife beating and battering (Garcia-Moreno, Heise, Jansen, Ellsberg, & Watts, 2005; Krug, Mercy, Dahlberg, & Zwi, 2002). This thesis will focus on IPV that is perpetrated against women by current intimate male partners.
[2] Odhikar, a human right NGO in Bangladesh, defines dowry related violence as the root cause of IPV. In 2013 in Bangladesh, it has been documented that 436 women were victims of dowry related violence, among those 154 were killed, 15 committed suicide with 261 were physically abused (Odhikar, 2014).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Midwifery"
Midwifery is a health profession concerned with the care of mothers and all stages of pregnancy, childbirth, and early postnatal period. Those that practice midwifery are called midwives.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please: