Biofortification of Baby Milk
Info: 10023 words (40 pages) Dissertation
Published: 16th Dec 2019
Tagged: Food and Nutrition
Abstract:
Many children around the world are undernourished. According to the World Health Organization (WHO), about 1.3 million children die as a result of a nutrition based deficiency. In addition, about 156 million children aged less than five years are suffering from stunting, and about 50 million of the same age suffer from wasting (1). It is clear that many children worldwide have inadequate nutrition, which makes them vulnerable to many diseases and sometimes death. To protect kids from these serious consequences, their food must contain essential nutrition supplements that includes vitamins and minerals. This is because of the importance of minerals and vitamins in the growth and development stages of children. Therefore, infant formulas must contain the essential vitamins and minerals for the physiological functions in the body of infants. However, a number of micronutrients should be suitable for the body’s needs, so that it does not result in deficiency or of overdoses.
Food fortification means the adding of micronutrients to food during its manufacture (2). One must choose the appropriate method of infant formula fortification to ensure the preservation of micronutrients during processing and storage. Nanotechnology in food fortification has several benefits, including economic, practical, plus effective and healthy benefits for the body by increasing the supply of nutrients (3). Nanotechnology in food and dairy manufacture is divided into two categories; food additives (nano inside) and food and dairy packaging (nano outside).
| Abstract …………………. …………………………………………………………….. | 4 |
| Introduction …………………………………………………………………………….. | 5 |
| Minerals to be fortified ………………………………………………………………… | 6 |
| Calcium …………………………………………..…………………………………… | 6 |
| Copper …………………………………………..……………………………………. | 6 |
| Fluoride …………………………………………..…………………………………… | 8 |
| Iodine …………………………………………..……………………………………… | 9 |
| Iron …………………………………………..………………………………………… | 10 |
| Magnesium …………………………………………..……………………………….. | 11 |
| Manganese …………………………………………..……………………………… | 12 |
| Selenium …………………………………………..………………………………….. | 12 |
| Sodium …………………………………………..……………………………………. | 13 |
| Zinc …………………………………………..………………………………………… | 13 |
| Vitamins …………………………………………..…………………………………….. | 14 |
| Water-Soluble Vitamins ……………………………………………………………….. | 14 |
| Vitamin B1 …………………………………………..………………………………… | 14 |
| Vitamin B2 …………………………………………..………………………………… | 15 |
| Vitamin B3 …………………………………………..………………………………… | 15 |
| Vitamin B5 ………………………………………..…………………………………… | 15 |
| Vitamin B6 ………………………………………..…………………………………… | 15 |
| Vitamin B7………………………………………..…………………………………… | 16 |
| Vitamin B9 ………………………………………..…………………………………… | 16 |
| Vitamin B12 ………………………………………..…………………………………. | 16 |
| Vitamin C………………………………………..……………………………………… | 16 |
| Fat-Soluble Vitamins ………………………………………..………………………… | 17 |
| Vitamin A ………………………………………..…………………………………….. | 17 |
| Vitamin D ………………………………………..…………………………………….. | 17 |
| Vitamin E ………………………………………..…………………………………….. | 19 |
| Vitamin K ………………………………………..…………………………………….. | 19 |
| Vitamins and Minerals Fortification ………………………………………..………… | 20 |
| Nanotechnology ………………………………………..……………………………… | 20 |
| Food additives (nano inside) ………………………………………..……………… | 20 |
| Methods of fortification ………………………………………..………………………. | 22 |
|
22 |
|
23 |
| Conclusion ………………………………………..……………………………………. | 24 |
| References ………………………………………..……………………………………. | 25 |
Table of Contents:
Introduction:
According to (WHO), 45% of children around the world die due to a lack of nutrition. In 2015, 156 million under the age of five years suffered from stunting (too short compared to their age), 50 million of the same age suffered from wasting (too thin compared to their age). In contrast, 42 million children around the world were overweight and obese (1). All these facts show that many children worldwide do not receive adequate nutrition. Therefore, one must support all sources of nutrition for children by providing the essential nutrients, which are necessary for growth and which protect against diseases.
WHO and UNICEF, recommend providing early breastfeeding during the first hour from birth and to continue breastfeeding exclusively for six months. After six months, one can begin to give children safe and complementary nutrition with continued breastfeeding up to two years of age (1). This is because breastfeeding contains all the required nutrients for healthy growth and development. Also, it contains antibodies, that protects the baby from common childhood diseases like pneumonia and diarrhea. Moreover, breastfeeding is easily available and affordable, which ensures that children receive adequate nutrition (4). However, there are exceptional circumstances that may prevent or reduce breastfeeding such as maternal exposure to some diseases, teenage mothers and infants who suffer from malnutrition(1). For these reasons, formula milk is an appropriate alternative.
“Infant formula is defined as a breast milk substitute that can fulfil by itself all the nutritional requirements of an infant from birth up to the introduction of complementary feeding” (5). The aim of formula milk is to supply a formula-fed infant the same growth and development as a breastfeed infant. So, an infant formula must be prepared carefully to meet the needs of infants, not only the macronutrients (carbohydrates, proteins and lipids), but also the micronutrients (vitamins, minerals, etc.). Cow’s milk is the essential ingredient for an infant formula, but it cannot be given to babies because of the different composition of breast milk (5). Although, the milk is rich in nutritional proteins, amino acids, minerals and vitamins, some of these elements are lost during the manufacturing process. For example, vitamins in food are susceptible to loss due to technological or cooking processes. Fat soluble vitamins are destroyed by oxygen, whereas B vitamins are destroyed by temperature and light (6). Therefore, there should be a careful selection of vitamins and minerals to be added to an infant formula (3).
Fortification is defined as the addition or enrichment of micronutrients to the diet, whether these nutrients are normally present in the food or not. The goal of food fortification is to prevent or correct a demonstrated deficiency. However, it should be added in sufficient quantities to meet targets without causing a risk of toxicity as a result of overdosing (3). In the process of fortification one must choose the appropriate method to ensure the preservation of the minerals and vitamins during processing and storage. Recently, nanotechnology applications have played an important role in food fortification, because of the increase in surface area in nano size when compared with the bulk materials of the same components. Nanoparticles are absorbed in the digestive tract easily, leading to the increased bioavailability of nutrients in the body (3).
The aim of this report is to discuss the importance of vitamins and minerals for the physiological functions the body. Furthermore, this review will explain the effects of a lack of micronutrients especially in infants, and the consequences as a result of deficiency. These consequences could be reduced in infants by improving the micronutrient value of infant formulas. This can be obtained by using nanotechnology to fortify baby milk. This review contains three sections. The first section will explain the importance of minerals for the human body and diseases resulting from either shortage or excess (overdosing). In addition, it will discuss the metabolism of minerals, and the factors that could have an effect on their absorption. The second section will demonstrate the importance of vitamins for the physiological functions, and it will show the damages which can be caused by a deficiency or too high a dose. The last section will explain the background of food fortification especially using nanotechnology.
Essential minerals and vitamins for babies:
Minerals to be fortified:
Minerals are inorganic elements that are necessary for normal growth and development of the body (3). Although, minerals are essential for several biological processes, the body needs only small amounts of them to complete the vital functions.
Calcium:
It is known that, calcium is the essential ingredient for building bones, which is considered the main cation of bone mineralization. Also, calcium plays other important roles in the body including a signaling role and as an intrasellar messenger in many systems and cells (7).
There are two routes for absorbing calcium through the intestine; transcellular and paracellular. The transcellular route is saturable and it mainly depends on vitamin D, while the paracellular route is non-saturable and is the transport mechanism for most calcium absorption (7)(8). The process of transcellular calcium transport in the intestine is affected by vitamin D. The calcium intake recorded in formula-fed infants during the first year of life is up to 900mg/day; it is higher than the calcium intake in breast-fed infants which is about 200 mg/day. The absorption fraction in this range is between 30% and 60% at the lowest intake. There is no evidence of damage at the highest intake of calcium. There is no evidence of damage to the high intakes of calcium (9).
There are several factors affecting calcium absorption. For example, calcium absorption in a formula containing lactose is about 60%, which is greater than from a lactose-free formula (9)(10).
A deficiency of calcium could lead to osteomalacia and osteoporosis due to inadequate mineralization of the bone matrix, inaccessibility of peak bone mass, a higher risk of colon cancer, growth stoppage and high blood pressure (3). Rickets is a common disease among children resulting from a lack of vitamins and calcium intake. However, there are many cases of rickets in children due to low calcium in the presence of sufficient vitamin D intake. For example, in rural villages of South Africa, the cause of rickets is attributed to low calcium intakes, where the children’s meals were free of milk and milk products. It has been estimated that their calcium intake is about 200mg. This amount of calcium intake was very small when compared with the children’s needs (11). In contrast, overdoses of calcium intake may cause hypercalcemia (kidney stones, nausea, constipation). In extreme cases, it might lead to coma and death (3).
Table 1. Recommended Dietary Allowances of Calcium Intakes for Children(12)
| Age | RDA (per day) |
| 0-6 months | 200mg |
| 7-12 months | 260mg |
| 1-3 years | 700mg |
| 4-8 years | 1000mg |
| 9-13 years | 1300mg |
Copper:
In general, dairy products are considered poor sources of copper. However, copper concentration in human milk is higher than in cows’ milk. Over the past 25 years most infant formulas have been fortified with copper by 90-12mcg/100 kal (approx. 110-160 mcg/kg/d). This requirement has changed to 120-150 mcg/kg/d or between 100-130 mcg/kg/d(13).
Copper is required for growth and development, where it works as a significant catalytic cofactor to oxidize proteins which perform many fundamental biological functions (14). “Further studies confirmed these findings and established that copper was required for infant growth, host defense mechanisms, bone strength, red and white cell maturation, iron transport, cholesterol metabolism, myocardial contractility, glucose metabolism, and brain development” (15).
In humans, copper is absorbed into the small intestine and stomach in small proportions.
The proteins in blood plasma and interstitial fluid play an important role in uptake and transport of copper by affinity copper binding. These proteins include albumin which is bound to 10-12% of the total copper in plasma. But it is not required for the absorption of copper in the liver and kidney. Ceruloplasmin is likely the major source of copper for other types of tissues. Due to the nature of highly reactive copper, it is possible to interact with cell membrane proteins and nucleic acids in the cells and damage them. Thus, copper (Cu) is delivered to the cells as copper chaperone proteins instead of free ions (14).
Copper deficiency is often seen in infants, during the first five months – the liver stores provide a sufficient quantity of copper for both preterm infants and full-term infants. Copper deficiency in this period is due to a decrease in copper deposits at birth, malabsorption, inadequate dietary intake of copper or increase of the copper loss (15). However, preterm infants are more susceptible to copper deficiency, and this is because of the lack of copper in the liver stores and their high requirements, which are necessary for rapid growth. Copper deficiency might occur in other cases, such as where formula milk is not fortified with copper, or there are high intakes of iron, zinc or ascorbic acid, which reduces the copper absorption rate. However, most cases of copper deficiency occur in children who are malnourished, whether due to low birth weight, a short breast feeding period, diarrheal disease or other deficiency factors (15). All these cases of decreases of copper in the body lead to hypochromic anemia not responding to iron, a defect in the production of heme and depigmentation of skin and hair (3). In contrast, a high intake of copper could lead to toxicity. Although copper overload is likely to happen in only a few cases compared with copper deficiency, it might lead to vomiting, hepatic necrosis, nausea and cellular oxidative stress. High doses of copper could be more dangerous for patients who suffer from genetic diseases. These diseases have a higher risk of accumulating of copper, such as Wilson’s disease (WD) (16)(3).
Fluoride:
Fluoride plays an important role in bones and teeth. In the bone, it can stimulate bone cells and increases the distribution of new mental in cancellous bone. Also, it reduces the solubility of the bone (apatite) by the merger of fluoride with bone crystals, which become bigger and more resistant to osteoclastic attack (17). In teeth, the basic role of fluoride is to protect the teeth from decay. This occurs because of the fermentation of carbohydrates to acids, which demineralize tooth enamels, by colonies of bacteria on tooth surfaces (17).
As with most nutrients, fluoride is absorbed significantly through the digestive system but the absorption ratio is variable (ranging 10-90%) and depends on influential factors (18). During the first year, fluoride supplements for children should consider other sources such as fluoridated water to avoid the risk of dental fluorosis, and an increase of the brittleness of bones and ligament (17)(3).
Tooth decay is one of the most common health problems among children around the world even in the developed countries. In 2013, for example, about 31% of British children who were aged 5 years and about 46% of 8 years olds were suffering from decay in primary teeth (19). Dental caries could be a serious health problem at all stages of life, due to severe pain in the mouth resulting from tooth decay. Desire and ability to eat will be reduced which can lead to malnutrition (17).
Table 2. Dietary Reference Intakes for Fluoride in Children
| Age group | Dietary Reference Intakes for Fluoride | ||
| Reference weight kg(lb) | Adequate intake (mg/day) | Tolerable upper limit (mg/day) | |
| Infants 0-6 months | 7(16) | 0.01 | 0.7 |
| Infants 6-12 months | 9(20) | 0.5 | 0.9 |
| Children 1-3 years | 13(29) | 0.7 | 1.3 |
Iodine:
Milk and its products are a great source of iodine. The most important functions of iodine in human bodies are helping in the body’s growth and development, and participation in the formation of thyroid hormones(3). Most of the iodine that is found in food is inorganic. This inorganic iodine is mostly absorbed through the gastrointestinal tract, whilst other types of iodine are converted to inorganic forms before absorption. Iodide ions are linked with plasma proteins, where they are oxidized to iodine in the thyroid gland. The thyroid hormones are formed by the interaction of the tyrosine components of thyroglobulin with iodine (8).
A deficiency of iodine has several negative impacts on growth and development in humans. Iodine deficiency leads to inadequate thyroid hormone production and all iodine deficiency disorders are called panel. Health problems caused by iodine deficiency are hypothyroidism, stillbirths, abortions, congenital anomalies dwarfism, impaired mental function, and delayed physical development in adults. Thus, this element is an essential nutrient especially in pregnancy because of the increase in production of thyroid hormones and its transfer with iodine to the fetus (3)(20).
Table 3. US Institute of Medicine Recommendation for Iodine Intake by Age (20)
| Age | Iodine intake (µg/day) |
| Infants 0-12 months | 110/130 |
| Children 1-8 years | 90 |
| Pregnancy | 220 |
| Lactation | 290 |
Table 4. WHO Recommendation for Iodine Intake by Age (20)
| Age | Iodine intake (µg/day) |
| Children 0-5 years | 90 |
| Children 6-12 | 120 |
| Pregnancy | 250 |
| Lactation | 250 |
Iron:
Iron is one of the trace minerals which are necessary for growth and development. It has a significant role in electron transport, DNA synthesis and oxygen transport. The basic physiological functions of iron in the body are the metalloproteins such as, hemoglobin, myoglobin and oxidases (3)(21). The free radical form of iron leads to tissue damage. Therefore, it should be kept in the trivalent redox state or linked to proteins. Most iron in food exists as ferric iron or heme iron (21). As with the majority of metals in food, iron is absorbed in the duodenum and the mucosal cells of the small intestine. There are three pathways to insert the three forms of iron (heme, ferric and ferrous) to the mucosal cells. These cells can either store the iron temporarily as heme, which is released and enters as non-heme, combined with ferritin, which transports iron in the blood, or these cells can be combined with ferro protein to transfer iron via body cells(8)(10). There are significant factors influencing the bioavailability of iron. For example, ascorbate and citrate have an important effect in enhancing iron absorption in the duodenum. This boost occurs because of the ability of ascorbate and citrate to reduce ferric to ferrous at low PH and due to its chelating properties. Although ascorbic acid has a negative effect on the absorption of iron in all inhibitors such as proteins and calcium in phytate and polyphenols, it increases the fortification of iron and native iron (8)(22). On the other hand, there are many factors inhibiting iron absorption including calcium, phytates, polyphenols, calcium some proteins such as portions from soybean, egg proteins, albumin and milk proteins. Other several types of metals could share the pathway of iron absorption in the intestine such as manganese, cobalt and zinc (22).
During the first six weeks of life the average hemoglobin synthesis decreases from about 170g/l to 120g/l. Iron is transferred from hemoglobin resulting from recirculation of iron in senescent red cells to iron stores. Thus, the size of infant doubled up during the 4-6 months in normal birth weight. Due to the rapid growth of infants between 6-24 months, iron requirements of the body will rise per kilogram weight from 300-600mg/k during this period (23).
Table 5 Recommendation for iron intake by different authorities(23).
| Age | Iron intake (mg/d) |
| 6-12 months | 7.8 – 11mg |
| 1-3 years | 5.8 – 9mg |
| 4-8 years | 6.1 – 10mg |
| 9-13 years | 8 – 10mg |
The main reason for iron deficiency in the body is the depletion of iron stores. Iron deficiency could lead to anemia where the level of hemoglobin in blood is low when compared with normal levels (8). According to WHO there are about two billion people around the world who are suffering from anemia, and 50% of this anemia is caused by iron deficiency. It affects all ages but is more prevalent in women and young children(22).
Table 6 Global prevalence of anemia and population affected of children(24).
| Group | Prevalence of anemia | Population | Affect | |
| Percent % | 95% Cl | Number (millions) | 95% Cl | |
| Preschool age children | 47.4 | 45.7- 49.1 | 293 | 283-303 |
| School age children | 25.4 | 19.9-30.9 | 305 | 238-371 |
To minimize the risk of iron deficiency, infant food and milk should be supported by iron fortification. Even in the case of breastfeeding, infants should be supplemented with iron. Because of the influence of proteins in human milk on the absorption of iron in the body and due to the influence of protein, one should not use whole milk for formula-fed infants before one year of age.
Magnesium:
Magnesium has two significant properties which are competing with calcium to bind with membranes and proteins and its ability of forming chelates with ATP. For these properties magnesium plays a great role in physiological functions of the body including, carbohydrate metabolism, proper functioning in different organs such as nerves, muscles and cardiovascular systems, and growth and proper maintenance of bones. Also, more than 300 enzymes need magnesium for them to be active (3)(25).
The absorption of magnesium from milk is better than from other types of food. The solubility ratio of magnesium is different between the different types of milk. In human milk, 92% of total magnesium is soluble, whilst in infant formulas, 83% is soluble in whey and 70% to 90% is soluble in casein (8). Magnesium is observed basically in the small intestine. The rise in absorption decreases with increasing of the dose. Magnesium uptake is kept either for the growth of tissue or stored in the skeleton, where 60% of magnesium in the human body occurs in bones. When the intake of magnesium is high, the kidney maintains balance because of its effectiveness in conserving magnesium (8)(25).
A deficiency of magnesium in humans does occasionally happen, and it can cause hypomagnesemia, weakness, respiratory disorders, high blood pressure, anxiety, nausea, tremors and muscle cramps(8)(3).
Manganese:
Manganese is one of the heaviest metals and a neurotoxicant, which is necessary for human health. The physical function of manganese in the body includes bone development, the immune function, wound healing, antioxidant defense and a great role in metabolism of cholesterol, amino acids and carbohydrates (3)(26).
The absorption of manganese is general relatively small, and it could be less than 5%. Homeostatic manganese is primarily regulated by excretion via bile and not through the absorbent. The most absorbed manganese is as Mn+2 transported through CC-2-macroglobulin and manganese as Mn+3 through transferrin. Manganese contains the enzyme arginase, which is responsible for pyruvate carboxylase catalysis and urea formation (8). High amounts of iron in food might reduce the absorption of manganese. This is because of the rivalry between iron and manganese on the same absorption sites and binding. Unlike the absorption of iron, manganese absorption is not affected by phytate, phosphate or ascorbic acid(8). The deficiency and disorders of manganese is that rarely it causes Hypocholesterolemia, weight loss and dermatitis (3).
Selenium:
Selenium is an essential trace mineral and an important part of most of the antioxidant enzymes like peroxidase and selenoprotein. In addition, it has several physiological functions including maintaining homeostasis, protection from radiation damage and contributing to the formation of triiodothyronine from thyroxine (3)(27).
The absorption of selenium compounds in the body varies depending on the chemical formula, where 80% in case of seleniteand selenomethionine is 90%. By intestinal cells in the duodenum, selenium is absorbed via amino acid transport systems. Selenium is decomposed into elemental selenium, which gets included in glutathione peroxidase (GPx) to give selenoproteins. In the liver selenoproteins are changed into selenoprotein P (SePP) and distributed to the various organs of the body such as the heart, brain, muscles, kidney, gonads and spleen (27).
A deficiency of selenium causes cardiovascular diseases. In addition, there are many complex health outcomes due to a lack of selenium including abnormalities of gastrointestinal and nervous systems, a defect of the immune system and the thyroid, fertility and type 2 diabetes (27). In contrast, high doses of selenium lead to neuropathy, alteration in mental status, diarrhea, nausea and loss of hair and nails (3).
Table 7. Recommended Dietary Allowance and Tolerable Upper Intake of Selenium (27)
| Age | Recommended dietary allowance | Tolerable upper intake levels (µg/day) |
| 0-6 months | 15 | 45 |
| 7-12 months | 20 | 60 |
| 1-3 years | 20 | 90 |
Sodium:
Sodium is an important nutrient for the human body. It is extracellular caution, which has significant physiological functions including maintaining osmotic pressure which controls water balance, preserve heartbeat, ease of conducting nerve impulses, muscle contraction and various membrane transport proteins (3)(28).
Sodium is easily and mainly absorbed into the upper part of the small intestine. Glucose transfers the sodium across the intestinal epithelium, which depends on passive leaks and pumps located in the membranes of cells. Sodium is also absorbed in the rumen and in most parts of the digestive tract. It seems that, there is no control of sodium absorption, and where it is absorbed about 80% of sodium intake is by the digestive system (29).
The deficiency and disorders of sodium in the body lead to headache, vomiting, nausea, seizures, coma, cramps, fatigue, muscle weakness and short-term memory loss (3). Since there is no control of the absorption of sodium, there is a great possibility for high sodium intake. High sodium intake is one of the serious factors for hypertension in children. High blood pressure in the early stages of growth and development increases the proportion of risk for cardiovascular disease and death. In addition, it predisposes children to hypertension in adulthood (30).
Zinc:
The physiological roles of zinc are dependent on its biochemical mechanisms. Unlike iron which is found in defined cellular components, zinc is ubiquitous intracellularly. Zinc has three functions in biology: structural, catalytic and regulatory functions (31).
Carrie-mediated is the mechanism that contributes to zinc absorption in the small intestine. Zinc is also secreted in the small intestine. Zinc is also secreted in the large intestine, so it is difficult to determine zinc uptake. High or low zinc uptake in the body depends on dietary zinc. There are some dietary factors affecting bioavailability of zinc absorption. Iron and calcium might have negative effects upon zinc absorption, unlike proteins which can have positive impacts (31).
The deficiency and disorders of zinc lead to growth arrest, chronic diarrhea, behavioural changes, stunted growth, poor wound healing, hypogonadism and infertility. By contrast, an overdose of zinc causes weakness, diaphoresis, nausea, gastric erosions low HDL, epigastric pain and impaired cellular immunity(3).
Vitamins:
Vitamins are a set of organic compounds, which are chemically heterogeneous. They are present in small quantities in natural foodstuffs and are considered very essential for growth and metabolism in the human body (32). Vitamins are classified into two groups according to their solubility, the fat-soluble vitamins: A, D, E, K, and the water-soluble vitamins: Thiamine, Riboflavin, Niacin, Pantothenic acid, Pyridoxine, Biotin, Folic acid, Cobalamin and Ascorbic acid (3)(32).
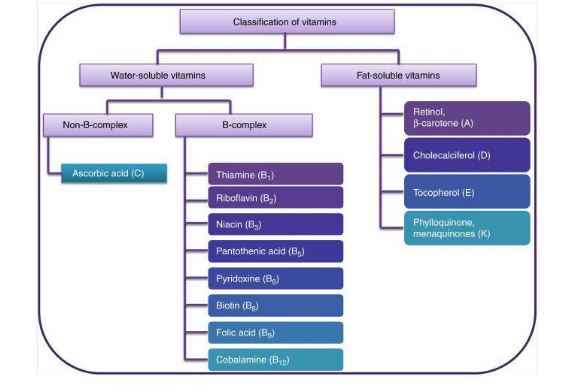
Figure 1 Classification of Vitamins(3).
Water-Soluble Vitamins:
Vitamin B group.
B vitamins are soluble in water. They are significant cofactors to the interaction of enzymes. B vitamins have an important role in energy production through the processing of fats and carbohydrates (32).
Vitamin B1 (Thiamine)
The physiological functions of Thiamin are: maintains proper functioning of digestive system and nervous system, works as a coenzyme for enzymes such as transketolase and ketoglutarate dehydrogenase (3). Thiamine pyrophosphate is the active form of this vitamin. The deficiency and disorders of vitamin B1 cause: Beriberi (70% of patients who suffer from this disease have ocular abnormalities like optic atrophy, dry eyes and epithelial changes in the conjunctiva. Since vitamin B1 deficiency is often caused by a lack of nutrition, it could result in an imbalance of the cardiac muscle, skeletal muscle and the nervous system. This may lead to reduced blood pressure, muscle weakness, hypothermia, paresthesia and anorexia (32).
Vitamin B2 (Riboflavin)
Riboflavin has important effects in the body, where it works as a prosthetic set of flavoproteins, as a coenzyme in reduction reactions and as a coenzyme in oxidation. Riboflavin deficiency causes normochromic anemia, normocytic anemia, stomatitis, cheilosis, edema of the nasopharyngeal mucosal, hyperaemia, seborrhoeic dermatitis and lesions at the corner of tongue, lips and mouth (3).
Vitamin B3 (Niacin)
The physiological functions of Niacin are as active part of NAD+ and NADP+, in addition to being a coenzyme in reduction reactions and oxidation (3). Niacin deficiency occurs for two reasons. The main reason is due to low nicotinamide and tryptophan in the diet. The second reason can be as a result of cirrhosis, chronic diarrhea, and also because of intensive parenteral nutrition fluids and cirrhosis (32). Niacin deficiency leads to Pellagra (it does not affect infants and children) (33), stomatitis, glossitis, burning dysesthesias and vertigo. Overdoses of this vitamin can cause hyperglycemia, hyperuricemia, parenchymal and vasomotor phenomenons (flushing) (3).
Vitamin B5 (Pantothenic Acid)
Pantothenic acid mainly exists in the human body as coenzyme A. It is essential for several metabolic processes, especially the metabolism of fat, proteins and carbohydrates (32). In addition, vitamin B5 has a role in the formation of vitamins A and D (3). A deficiency of vitamin B5 could lead to vomiting, diarrhea, insomnia, fatigue, high insulin sensitivity, abdominal pain, paresthesia of the extremities, mental depression and neuromotor disorders (3).
Vitamin B6 (Pyridoxine)
Pyridoxine has an important role as a coenzyme in decarboxylation of amino acids, transamination and in glycogen phosphorylase. Also it is involved in the formation of Niacin from tryptophan, compilation of many neurotransmitters, formation of δ-aminolevulinic acid, a remedy for regulating
steroid activity and discouraging receptor affinity to DNA(3). A deficiency of vitamin B6 in infants might lead to convulsions, anemia, hyper-irritability, weight loss and growth retardation (32). High doses of this vitamin cause photosensitivity and peripheral neuropathy (3).
Vitamin B7 (Biotin)
Biotin is synthesized by bacterial action in the intestine and is a factor in the formation of fatty acids. Biotin improves the condition of hair, nails and skin cells. In addition, it supports the synthesis of keratin processes. A deficiency of Biotin is rare and might cause localized infections of the skin around the mouth, nose, eyes, conjunctivitis and abnormalities in fat metabolic (32).
Vitamin B9 (Folic Acid, Folate)
The physiological function of folate is as a coenzyme in the transfer of single carbon in the formation of nucleotides and the metabolism of amino acids. A deficiency of vitamin B9 can cause: neural tube disorders in children, glossitis, diarrhea, megaloblastic anemia and cell hyperplasia in the bone marrow that creates blood with immature nuclei, resulting in ineffective DNA consists(3).
Vitamin B12 (Cyanocobalamin)
Vitamin B12 is one of the essential vitamins for the health of the body, where it has physiological functions in the metabolism of folic acid and transfer of the fragments of single carbon (3). Thus, it is necessary for the proper functioning of the nervous system and affects the synthesis of blood cells (32). A deficiency of vitamin B12 cause pernicious anemia, loss of absorption in the intestine, atrophic gastritis, pancreatic insufficiency, demyelination of nerves in the brain, peripheral nerves and nerves within lateral columns and posterior of the spinal cord, depression, mental distress, psychoses and complications in neurology and hematology (3).
Vitamin C (Ascorbic Acid)
Ascorbic acid has an active role in many functions of the body. Especially, it is essential to the formation of collagen. Also, it produces noradrenaline and neurotransmitters. In addition, vitamin C improves the function of the hepatic oxygenase system, promotes iron absorption and increases the intake of non-heme iron in the intestine. Another function is biosynthesis of carnitine, norepinephrine and bile acids. Moreover, ascorbic acid works as an antioxidant. Vitamin C deficiency occurs due to incorrect nutrition and could lead to Scurvy, defects in bone growth (in infants) and ossification. In contrast, overdoses of vitamin C cause a higher risk of oxalate kidney stones (3)(32).
Table 8 Recommended Daily Allowances of Water-soluble Vitamins for Children (3).
| Water-soluble vitamins | RDA (per day) |
| B1 (Thiamine) | 0.5-0.9 (mg) |
| B2 (Riboflavin) | 0.5-0.9 (mg) |
| B3 (Niacin) | 6-12 (mg) |
| B5 (Pantothenic acid) | 2-4 (mg) |
| B6 (Pyridoxine) | 0.5-1 (mg) |
| B7 (Biotin) | 8-20 (µg) |
| B9 (Folic acid) | 160-300 (µg) |
| B12 (Cyanocobalamin) | 0.9-1.8 (µg) |
| C (Ascorbic acid) | 30-35 (mg) |
Fat-soluble Vitamins:
“Fat-soluble vitamins are polar molecules that are hydrophobic derivatives of isoprene” (32). They are soluble in fats and are stored in chylomicrons (fat globules). These chylomicrons travel via the lymphatic system to the adipose tissue, where they are then stored. A deficiency of these types of vitamins might be the result of a lack of intake. Also it could be as a result of a defect in absorption resulting from the overlapping of certain kinds of drugs or diseases. High doses of fat-soluble vitamins cause a risk of poisoning in the human body (3).
Vitamin A (Retinol, ß-Carotene)
There are several biological functionsof vitamin A including sensory performance, cell differentiation, immune functions, hematopoiesis, embryonic development, development of tumor resistances, reproduction and growth. Retinol is created inside the body from carotene, the majority of which is manufactured by plants and to lesser extent manufactured by microorganisms (32). Vitamin A deficiency is one of the most common nutritional deficiency diseases and is a major threat to children of preschool age. In addition, it is one of the diseases where the necessary treatments should be carried out immediately, because it is considered the main cause of blindness in children of developed countries (32). Also, it can lead to keratomalacia (degeneration of the cornea), skin keratomalacia and follicular hyperkeratosis xerophthalmia (3). High doses of vitamin A lead to skin exfoliation, hypertension, ataxia, dermatitis, alopecia, cheilitis, conjunctivitis, hyperlipidemia and pain in the muscles and bone (3).
Vitamin D (Cholecalciferol)
Vitamin D is produced naturally in the skin by exposure to sunlight. Also, it is obtained from foods, whether they contain vitamin D naturally or are fortified with vitamin D (34). There are several physiological functions of vitamin D in the body. The most important one is to maintain the concentration of calcium and phosphorus levels in the blood, that have a significant role in bone metabolism, transcription regulation and a variety of metabolic functions (34). In addition, vitamin D has an essential impact in increasing the efficiency of calcium and phosphorus absorption in the small intestine through the interaction with vitamin D receptor (VDR). Moreover, vitamin D motivates the absorption of calcium from the glomerular filtrate in the kidneys (34). A deficiency of vitamin D is one of the most prevalent health problems worldwide, and occurs in about 30-50% of the world’s population and in all age groups (32). Vitamin D deficiency leads to Rickets in children and osteomalacia in adults. Also it causes pathological fractures, bone deformation and low calcium and phosphate concentration in serum (3).
Vitamin D deficiency is one of the most common causes of rickets in children. The appearance of clinical signs of rickets in children begins between 6 months to 1.5 years, which include widening of the epiphyseal plates at the end of long bones, rachitic rosary and bowing deformities of the legs in newborns. Sweating is the most common symptom, which is because of neuromuscular irritability (34).
Rickets in Europe was common in the mid-twentieth century and was known as the English disease, due to its large spread within England. Because of public awareness, supplements and clean air legislation, the cases of rickets have become very few in the UK. In contrast, recently several cases of rickets in the UK have been recorded amongst children of migrant families from Asia and Africa, and there are fears of increased cases in the future (35). This is maybe due to the lack of awareness of rickets in these cultures. On the other hand, despite the abundant sunshine in the Middle East and Africa, rickets rates are also too high in these areas. Low levels of vitamin D are caused by low socioeconomic status, the winter season and conservative clothing style (36). For these reasons, one should not rely on the natural formation of vitamin D from sunlight, and it should added to by fortified nutrition with this vitamin especially for kids.
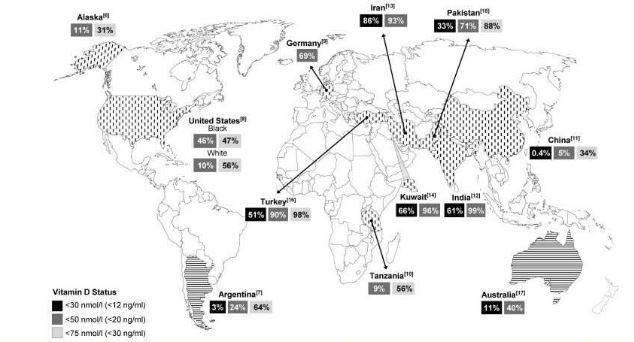
Figure 2 Prevalence rates of vitamin D deficiency in infants around the world. It has been found in 12 studies: 1 in Europe, 3 in America, 6 in Asia, 1 in Oceania and 1 in Africa. The highest prevalence rate of vitamin D deficiency has been found in newborn infants in the Middle East (3).
Vitamin E (Tocopherol)
Vitamin E has an essential role in protecting polyunsaturated fatty acids (PUFAs), low-density lipoproteins and other cell membrane contents. The deficiency of this vitamin occurs very little in humans, except in certain circumstances relating to the metabolism of vitamin E (32). Vitamin E deficiency could lead to hemolytic anemia, ophthalmoplegia, peripheral neuropathies and serious neurological disorders (rarely happens). However, overdoses of vitamin E are dangerous and could lead to rise in the occurrence of hemorrhagic strokes (3).
Vitamin K (Phylloquinone)
Vitamin K is necessary to posttranslational chemical correction of glutamic acid residues in a group of proteins. In addition, vitamin K acts as a coenzyme for blood clotting enzymes. A deficiency of vitamin K causes a defect in blood clothing, fat malabsorption in adults and hemorrhagic diseases in newborn babies. In contrast, high doses of this vitamin lead to flushing collapse of the cardiovascular system and dyspnea (3).
Table 9 Recommended Daily Allowances of Fat-soluble Vitamins for Children (3).
| Fat-soluble vitamins | RDA (per day) |
| A (Retinol, ß-Carotene) | 400-500 (µg) |
| D (Cholecalciferol) | 5 (µg) |
| E (Tocopherol) | 5-7 (mg) |
| K (Phylloquinone) | 15-25 (µg) |
Vitamins and Minerals Fortification:
According to The Codex Alimentarius, “which is part of the Food and Agriculture Organization / World Health Organization Food Standardization Program”, consolidated general principles of adding nutrients to the food in countries (37) :
- Basic nutrients must be present in the specified levels, without resulting in excess or deficiency.
- Adding the essential nutrients for food should not adversely affect the metabolism of other nutrients.
- The basic nutrients should be stable enough in the food during usual conditions of packing, distribution, storage and use.
- The basic nutrients in the food must be biologically available.
- The basic nutrients must not add undesirable properties, and must not unduly restrict the shelf life.
- Processing facilities and technology used to add nutrients in a satisfactory manner should be available.
- Adding any essential nutrients to the diet should not be used in consumer deception in regards to nutrient merits of the product.
- The cost of adding nutrients must be suitable for the intended recipients.
- It is necessary to provide ways to measure and monitor the levels of essential nutrients which are added to the food.
- When food standards require adding essential nutrients for food and they are available, specific provisions must be inserted to determine the required nutrients and their concentrations which must be present in the food to achieve the desired goals.
There are many challenges facing food fortification. For example, mineral fortification of milk is difficult because at the normal PH of its soluble phase it is saturated. So, adding more minerals is challenging. Therefore, it is very important to choose the appropriate source of mineral for a particular application. In dairy applications mineral salts are mostly used (38).
Table 10 Some salts of Calcium, Magnesium and Zinc Approved for Fortification in Europe (38).
| Compound | Mineral content | Solubility | Taste |
| Calcium carbonate | 40% | Insoluble | Soapy, lemony |
| Calcium lactate. 5H2O | 14% | 90g/l | Bitter at high concentration |
| Tricalcium phosphate | 40% | Insoluble | Sandy, bland |
| Magnesium carbonate basic.5H2O | 24% | 4g/l | Earthy |
| Magnesium sulfate.7H2O | 10% | 710g/l | Saline, bitter |
| Trimagnesium phosphate.5H2O | 21% | Insoluble | Neutral |
| Zinc citrate | 31% | 3g/l | Slightly bitter |
| Zinc oxide | 80% | Insoluble | Bitter |
| Zinc sulfate.7H2O | 23% | 960g/l | Astringent, bitter, metallic |
Soluble mineral salts can affect the taste and increase the PH where there is a high level of fortification. While insoluble mineral salts can influence mouth feeling which includes chalkiness and grittiness, in addition, they could lead to sedimentation in some products. To solve these problems, micronised mineral salts are considered as a great option. For example, reducing the particle size to ultrafine particles can decrease the speed of sedimentation. Thus, one could achieve higher levels of fortification by using particles smaller than 20µm than by using dissolved minerals (38)
Nanotechnology is one of the modern methods which are essential for food and dairy manufacturers. Nanotechnology has a significant impact on the development of functional foods. “Nanotechnology is defined as the design, production and application of structures, devices and systems through control of the size and shape of the material at the nanometer (10-9 of a meter) scale where unique phenomena enable novel applications” (39). Nanotechnology applications in the food and dairy industry are divided into two main sections: food additives (nano inside) and food and dairy packaging (nano outside).
Food additives (nano inside):
The different physical and molecular forms (polarities, molecular weight, physical state) of functional ingredients (such as vitamins) are pure forms. Therefore, it is rare to utilize these ingredients directly. Instead, they are mostly combined into a delivery system, which includes association colloids, biopolymeric nanoparticles and nanoemulsion (39).
Methods of fortification:
1- Encapsulation
Encapsulation is a type of technology which forms a capsule by coating an active micronutrient, in order to enhance the retention time of micronutrients in the food and allow control of its release in the gastrointestinal tract. In addition, it can hide the disgusting flavor of some minerals and vitamins and increase their stability during the food storage process (3). Nanoencapsulation is a type of technology that protects the bioactive compounds and drugs from inappropriate conditions such as degradation through coating by a core material. Methodologies of encapsulation can be divided into physical processes, physicochemical processes and chemical processes(3).
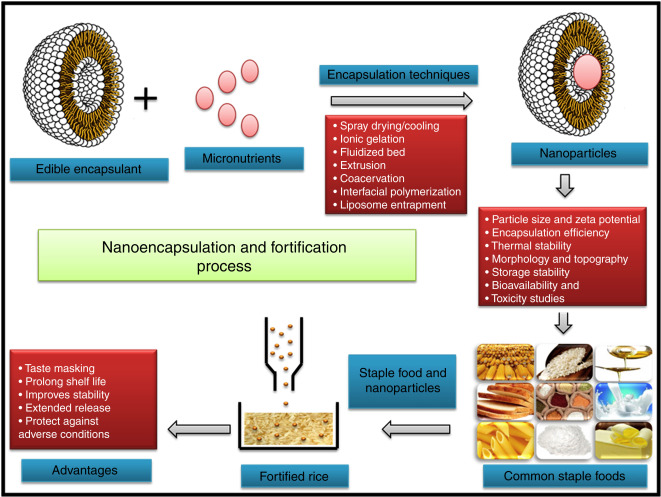
Figure 3 Schematic Representation of Nanoencapsulation and Fortification Processes (3).
2- Direct Addition:
It is one of the alternative methods that can protect the effective functional micronutrients from some conditions. In this method, nutrients are added directly to the food before consumption. Also, in this way, the degradation of micronutrients through heat processing of food is avoided, while it is added to the final product (3).
Conclusion:
Since milk is a staple food for infants during the first two years of life, it must contain all the essential minerals and vitamins for normal growth and development. For this reason, the most appropriate method of fortification must be chosen for adding micronutrients, so that, it will be effective and inexpensive in order to ensure its use in various parts of the world, especially in developing countries.
References:
1. World Health Organization, Infant and young child feeding, 2016, http://www.who/int/mediacentre/factsheets/fs342/en/ .
2. L.Allen, B.deBenoist, O.Dary, R.Hurrell, World Health Organization and Food and Agricultural Organization of the United Nations, 2006. ???
3. S.Juveriya Fathima, I.Nallamuthu, F.Khanum, Nutrient Delivery, 2017, doi: 10.1016/B978-0-12-804304-2.00012-3, 457-496.
4. World Health Organization, 10 Facts on breastfeeding, http://www.who.int/features/factfiles/breastfeeding/facts/en/index1.html .
5. E.Blanchard, P.Zhu, Handbook of Food Powder: Process and Properties, 2013, doi: 10.1533/9780857098672.3.465, 465-477.
6. M.Samaniego-Vaesken, E.Alonso-Aperte, G.Varela-Moreiras, Food & Nutrition Research, 2012, 56, doi: 10.3402/fnr.v56iO.5459.
7. F.Bronner, D.Pansu, The Journal of Nutrition, 1999, 129 (1), http://m.jn.nutrition.org/content/129/1/9.full , 9-12.
8. S.Fairweather-Tait, Nutrition Research Reviews, 1996, 9, doi:10.1079/NRR19960016, 295-324.
9. S.A.Abrams, Nutrients, 2010, 2(4), doi:10.3390/nu2040474, 474-480.
10. S.A.Abrams, I.J.Griffin, P.M.Davila, The American Journal of Clinical Nutrition, 2002, 76(2), http://m.ajcn.nutrition.org/content/76/2/442.full , 442-446.
11. J.M.Pettifor, The American Journal of Clinical Nutrition, 2004, 80 (6), 1725S-9S.
12. National Institutes of Health, Calcium, https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
13. I.Griffin, M.Domellöf, J.Bhatia, Dr Anderson, N.Kler, Early Human Development, 2013, 89, doi:10.1016/j.earlhumdev.2013.08.001, S29-S34.
14. H.Tapiero, D.M.Townsend, K.D.Tew, Biomedicine & Pharmacotherapy 2003, 57 (9), doi:10.1016/S0753-3322 (03) 00012-X, 386-398.
15. M.Olivares, R.Uauy, The American Journal of Clinical Nutrition, 1996, 63 (5), https://shib2idp.ntu.ac.uk/idp/profile/SAML2/Redirect/SSO?execution=e1s1&_eventId_proceed=1, 791S-796S.
16. R.Danzeisen, M.Araya, B.Harrison, C.Keen, M.Solioz, D.Thiele, H.McArdle, British Journal of Nutrition, 2007, 98 (4), doi: 10.1017/S0007114507798951, 676- 683.
17. CA.Palmer, JA.Gibert, Academy of Nutrition and Dietetics, 2012, 112 (9), doi: 10.1016/j.jand.2012.07.012, 1443-1453.
18. Y.Zheng, J.Wu, J.Ng, G.Wang, W.Lian, Toxicology Letters, 2002, 133 (1), doi: 10.1016/S0378-4274 (02) 00082-6 , 77-82.
19. NHS Digital, Child Dental Health Survey, 2013, http://content.digital.nhs.uk/catalogue/PUB17137, accessed 29th,December, 2016.
20. MB.Zimmermann, PL.Jooste, CS.Pandav, The Lancet, 2008, 372 (9645), doi: 10.1016/S0140-6736 (08) 61005-3, 1251-1262.
21. M.Conrad, J.Umbreit, American Journal of Hematology, 2000, 64(4), doi: 10.1002/1096-8652(200008)64:4<287::AID-AJH9>3.0.CO;2-L, 287- 298.
22. N.Abbaspour, R.Hurrell, R.Kelishadi, Journal of Research in Medical Science, 2014, 19(2), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999603/, 164-174.
23. M.Domellof, C.Braegger, C.Campoy, V.Colomb, T.Decsi, M.Fewtrell, D.Turch, Journal of Pediatric Gastroenterology and Nutrition, 58 (1), doi: 10.1097/MPG.0000000000000206, 119-129.
24. World Health Organization, Global anemia prevalence and number of individuals affected, http://www.who.int/vmnis/anaemia/prevalence/summary/anaemia_data-status-t2/en/, accessed 23th, December, 2016.
25. R.Swaminathan, The Clinical Biochemist Review, 2003, 24 (2), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1855626/, 47-66.
26. T.Peres, M.Aschner, Molecular, Genetic and Nutritional Aspects of Major and Trace Minerals, 2017, doi:10.1016/B978-0-12-802168-2.00030-0.
27. B.Santhosh Kumar, K.I.Priyadarsini, Biomedicine & Preventive Nutrition, 2014, 4 (2), doi:10.1016/j.bionut.2014.01.006.
28. D.Laubitz, F.K.Ghishan, P.R.Kiela, Molecular, Genetic and Nutritional Aspects of Major and Trace Minerals, 2017, doi: 10.1016/B978-0-12-802168-2.00040-3, 489-501.
29. L.R.McDowell, Minerals in Animal and Human Nutrition, 2003, doi:10.1016/B978-0-444-51367-0.50006-4, 101–128.
30. Q.Yang, Z.Zhang, E.V.Kuklina, J.Fang, C.Ayala, Y.Hong, F.Loustalot, S.Dai, J.P.Gunn, N.Tian, M.E.Cogswell, R.Merritt, Pediatrics, 2012, 130 (4), doi : 10.1542/peds.2011-3870, 611-619.
31. N.Roohani, R.Hurrell, R.Kelishadi, R.Schulin, Journal of Research in Medical Science, 2013, 18 (2), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3724376/, 144-157.
32. T.Baj, E.Sieniawska, Pharmacognosy, 2017, doi: 10.1016/B978-0-12-802104-0.00013-5, 281-292.
33. K.N.Nareen, V.V.Pai, P.Bagalkot, V.Kulkarni, P.Rashme, S.B.Athanikar, Nutrition, 2013, 29 (11- 12), doi: 10.1016/j.nut.2013.05.020, 1426- 1428.
34. A.Hossein-Nezhad,, M.F.Holick, Mayo Clinic Proceedings, 2013, 88 (7), doi: 10.1016/j.mayocp.2013.05.011, 720-755.
35. A.Prentice, The Journal of Steroid Biochemistry and Molecular Biology, 2013, 136, doi: 10.1016/j.jsbmb.2012.11.018, 201-206.
36. R.El-Rassi, G.Baliki, G.El-Hajj Fulheihan, International Osteoporosis Foundation, 2009, https://www.aub.edu.lb/fm/cmop/downloads/IOF-Vitamin_D-MEast_Africa.pdf, 1-4.
37. S.C.Liberato, H.M.Pinherio-Sant’Ana, Revista de Nutrição ( Rev.Nutr), 2006, 19 (2), doi: 10.1590/S1415-52732006000200009, 215-231.
38. M.Gerhart, M.Schottenheimer, Wellness Food Europe, 2013 http://www.jungbunzlauer.com/fileadmin/content/_PDF/Mineral_fortification_in_dairy_May13.pdf .
39. M.A.Qureshi, S.Karthikeyah, K.Punita, P.A.Khan, S.Uprit, U.K.Mishra, Pakistan Journal of Food Science, 2012, 22 (1),http://www.psfst.com/__jpd_fstr/28b7a72cf4eadd2186ba633ad826eceb.pdf, 23-31.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Food and Nutrition"
Food and Nutrition studies deal with the food necessary for health and growth, the different components of food, and interpreting how nutrients and other food substances affect health and wellbeing.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




