Irish Healthcare System Work Practice Organisation Evaluation
Info: 8982 words (36 pages) Dissertation
Published: 16th Dec 2019
Tagged: Healthcare
Assessment title- Work Practice Portfolio

- Key Features of Work Practice Organisation
- Evaluate the work practice organisation in terms of status and size in relation to both the Irish economy and world economy (if applicable).
 The Irish Healthcare System is made up of public, private and voluntary health and social services. Irish citizens have access to free public healthcare. However if the individual would like private care they must pay their own costs or claim on private health insurance.
The Irish Healthcare System is made up of public, private and voluntary health and social services. Irish citizens have access to free public healthcare. However if the individual would like private care they must pay their own costs or claim on private health insurance.
 Simon Harris is the Minister for Health. He is responsible for the development, provision and funding for all health and social services in Ireland.
Simon Harris is the Minister for Health. He is responsible for the development, provision and funding for all health and social services in Ireland.
The Health Service Executive (HSE) was established in 2005. The
HSE replaced the old 8 health boards. All health and social services provided in Ireland is authorised by the HSE. Tony O’Brien the former Director General resigned after a health scandal. This meant John Connaghan was appointed to the Acting Director General of the HSE.
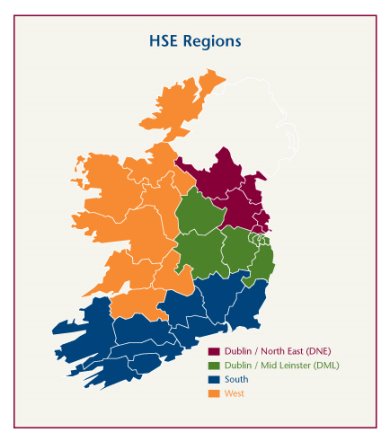
He reports directly to the Minister and the Department of Health. Mr. Connaghan is also in charge of all operational services of the HSE. The HSE delivers its services through public hospitals and local health offices throughout Ireland. There are four regions in the HSE. Each region has a
Regional Director. This person is in charge of the management of health and social services in that region. This regional director reports directly to the HSE director general.
There are four regions:
- Dublin/ North East– (County Cavan, County Louth, County Meath, County Monaghan and North Dublin)
- Dublin/ Mid Leinster-(County Kildare, County Laois, County Longford, County Offaly, County Westmeath, County Wicklow and South Dublin)
- South– (County Carlow, County Cork, County Kerry, County Kilkenny, County Waterford, County Wexford and South Tipperary.)
- HSE West- County Clare, County Donegal, County Galway, Country Leitrim, County Limerick, County Mayo, County Roscommon, Sligo and North Tipperary.
The HSE has over 127,000 direct employees such as doctors, nurses, physiotherapists, healthcare assistants, SALT’s, ambulance services, clerical, administration and housekeeping staff. This is making it the largest employer in the state.
In 2018 the HSE had the highest amount of money allocated at 14.4 million euro. Along with the 127,000 direct staff the HSE employs they also employ a large number of agency staff that are on temporary contracts.
The Minister for Health of Older People Services is Jim Daly. He is responsible for creating policies and delivering health and social services to older people throughout the country. In 2018 he has a budget of € 811 million, this being an increase of €48 million since 2017.
In comparison to Costa Rica which has around the same population as Ireland. They spend 5 billion on healthcare to whereas Ireland only spends 811 million.
The Work Practice Organisation (WPO) contributed €990 million from health services to government through direct taxation.
The Healthcare System is made up of 3 tiers:
Primary: this is the care a patient receives when in first contact with healthcare system.
Secondary: the treatment by specialists to who a patient has been referred by primary care providers such as doctors.
Tertiary: this is the treatment that is given in a health care centre. This includes treatment by highly trained specialists and sometimes advanced technology.
The private nursing home sector provides most of the residential care services for older people. There are 22,000 private nursing home beds in 440 nursing homes. Due to the demand for care this number is increasing all the time. Cost of care in the private nursing homes range from €900 to 1600 euro. The Nursing Home Support Scheme gives the majority of these residents assistance towards the weekly cost of care.
These nursing homes are inspected by HIQA and they must comply with the 32 Standards for Residential Care Settings for older people.  The HSE along with the government deliver the Nursing Home support scheme. This scheme reduces the cost of the persons care in a private or public nursing home. This assessment is means tested and is based on their income. This calculation will tell how much they will get towards the cost of their care each week. There has been €1.1 billion allocated to this scheme in 2018. This is an increase of €70 million since 2017.
The HSE along with the government deliver the Nursing Home support scheme. This scheme reduces the cost of the persons care in a private or public nursing home. This assessment is means tested and is based on their income. This calculation will tell how much they will get towards the cost of their care each week. There has been €1.1 billion allocated to this scheme in 2018. This is an increase of €70 million since 2017.
HIQA:
Health Information and Quality Authority
This is an independent authority that was established to enforce high quality and safe care for the people that use the health and social care services in Ireland.
HIQA reports across public, private and voluntary services. They are responsible for reporting to the Minister of Health and the Minister for Children and Youth Affairs. 
Their role is to:
- Develop standards
- Inspect and Review health and safety care services
- Support informed decisions on how services are delivered
The work place I carried out my work experience is part of the Irish Healthcare System. It is part of the private healthcare sector.
The Irish Healthcare System is made up of many different sectors. In Ireland there are over 360 NHI members throughout Ireland that are key healthcare providers in local communities. They have invested in this to provide high standards of care which they are regulated to.
The NHI is an important part of Irelands Healthcare System. Both private and public nursing homes should be a ‘home from home’ for both men and women who need continuous, specialist care nursing homes in Irish communities.
 The private and voluntary nursing homes are key employers and also make a great contribution to the local economy.
The private and voluntary nursing homes are key employers and also make a great contribution to the local economy.
In the private and voluntary nursing homes there are over 22,000 beds. This number accounts for over 80% of the country’s long term care. Nearly 50% of the beds in Irish hospitals are for people aged 65 and over.
Due to delayed discharges, 243,394 hospital day beds were lost in 2013. Over 75% of these delayed discharges were people waiting nursing home care.
There is over 24,000 staff employed throughout Ireland in both private and voluntary nursing homes. The private and voluntary nursing homes facilitate nearly 24,000 staff around Ireland. These healthcare settings make a huge contribution to local economies as they are lead employers within Irish communities.
The NHI has a clearly defined, departmental coordinated strategy. This strategy is developed along with the sector. Per year 900 new jobs could be created by the sector.
The private and voluntary nursing home sector is necessary for the provision of long term residential care throughout the country. Over a period of five years the number of people aged 65 and over increased by 14%. The CSO predicts that the old population will rise suddenly in the coming years. 22% of people aged 85 and over require care in nursing homes. It is predicted that this number will increase to 46% in 2021. The BDO report Health’s Aging Crisis: Time for Action (February 2014) states there may be a need of up to 8,000 nursing home beds by 2021.
The ESRI has said that from 2007 to 2021 there will be a need of an additional 13,324 long term residential care places, this is 888 per year.
The Centre for Ageing Research and Development in Ireland (CARDI) agrees and  confirms ESRI predictions.
confirms ESRI predictions.
The ESRI also predicts that people aged 65 and over with severe disabilities will increase by 56% from 2006-2021.
A strategy that helps both private and voluntary nursing homes to meet the growth and demand for care must be a government priority. This will help the sector meet the growing needs for long term residential care.
My WPO is part of NHI (Nursing Homes Ireland). It is located in Mountnugent, Cavan on the shores of Lough Sheelin. 
It accommodates up to 38 residents, both male and female and generally 65 years or older. The building consists of 24 ensuite single rooms, 4 twin rooms and 2 three bedded rooms all with ensuite.
Cost of living per week in the nursing home is 890 euro per week. This is a quite reduced rate than a local HSE home ST. Vincent’s Care Centre at 2,399 euro per week.
There is over 30 staff working in the nursing home. There are 2 staff nurses and 5 carers on per day shift. During the night shift there is one staff nurse and 2 carers.
Staff must have a minimum of level 5 award in Healthcare. It is important for staff to have their immunisations done. Training days are provided to staff to update them on any changes made to the system.
Most staff is local and travel to work each day. The wages the staff get benefits the local community as they are spending their wages there. Staff will purchase groceries in local shops. People with families may also send their child to school locally.
The nursing home helps the local community as it buys its fresh food produce from local shops, this will help it boost the local economy.
The nursing home also uses the local doctors if required along with the pharmacy to get residents prescriptions.
If residents are required to attend any appointments the nursing home gets a local taxi service to bring them to and from.
The government support care they have different schemes to help people and the nursing home. The Property Based Incentive Scheme allows nursing homes to claim tax reliefs on buildings and extensions.
- Summarise the work practice organisations’ structure, main aims, and, overall objectives.
I carried out my placement in Sheelin Nursing Home. This is a family run business. It prides itself on its homely and friendly atmosphere and its dedication to all its residents.
 It is located on the peaceful shores of Lough Sheelin in Mountnugent. It has a wide range of views of Mullaghmeen forest park and Lough Sheelin. It is a converted hotel and is based over three levels. The main dining room is on the middle floor, opposite the nurses’ station. There is a second dining room on the upper floor. There is also a visitor’s lounge and hairdressers. The building consists of 24 ensuite single rooms, 4 twin rooms and 2 three bedded rooms all ensuite.
It is located on the peaceful shores of Lough Sheelin in Mountnugent. It has a wide range of views of Mullaghmeen forest park and Lough Sheelin. It is a converted hotel and is based over three levels. The main dining room is on the middle floor, opposite the nurses’ station. There is a second dining room on the upper floor. There is also a visitor’s lounge and hairdressers. The building consists of 24 ensuite single rooms, 4 twin rooms and 2 three bedded rooms all ensuite.
We can accommodate up to 38 residents both male and female usually aged 65 and over. There are 2 staff nurses and 5 carers per day shift. During the night shift there is 1 staff nurse and 2 carers. The Director of Care is on site Monday-Friday from 9-5.
 They are able to provide care for all dependencies that need general care, young chronic care, brain injury, mild confusion and respite.
They are able to provide care for all dependencies that need general care, young chronic care, brain injury, mild confusion and respite.
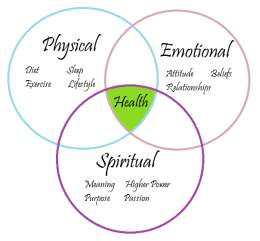
The staff are committed to making sure that the best possible care is given to clients. They ensure that all aspects of their well-being are catered for (mental, physical and spiritual) in a professional and safe environment. 
They aim to promote dignity, respect and independence as much as possible. The care team are there to support clients and families to ensure that quality care is given with trust and compassion all of the time.
With continuous staff training they aim to re  cognise and implement any improvements that are required. This is to ensure that the standard of care given is resident led and resident centred. The nursing home can accommodate people with different ranges of dependency ranging from low to maximum dependency.
cognise and implement any improvements that are required. This is to ensure that the standard of care given is resident led and resident centred. The nursing home can accommodate people with different ranges of dependency ranging from low to maximum dependency. 
Sheelin Nursing Home strives to provide a high quality service to all residents.
Visiting the nursing home is advised prior to admission so clients and families can familiarise themselves with the layout and to make an informed decision regarding committing to the facility. The WPO are aware that this is a huge change and transition in a persons life, and they are very open to discussions to how we can make the move as smooth as possible.
The Director of care is available by appointment to answer any concerns clients or families may have. Visiting residents in the nursing home is encouraged and non-restrictive with exception of meal times and after 9pm. Meal times are stated on a notice as you enter the nursing home foyer and a sign in/out book must also be completed by every visitor, in accordance with fire safety precautions.
Sheelin Nursing Home does reserve the right to impose restrictions on visiting arrangements where the visit or time of visit is deemed to pose a risk or where the resident requests restrictions. 

 Sheelin Nursing Home offers many services and activities for clients. The hairdresser attends the home every Thursday. Mass is held every 3rd Sunday for Roman Catholics, it is also held additionally on holy days. Residents are motivated to take part in the recreational activities from Monday-Friday and some weekends. The residents enjoy the full afternoon of live music on the last Friday of every month. Some residents go on outings with the OAP social club monthly. A professional physiotherapist and occupational therapist attends the home weekly to assess client’s needs.
Sheelin Nursing Home offers many services and activities for clients. The hairdresser attends the home every Thursday. Mass is held every 3rd Sunday for Roman Catholics, it is also held additionally on holy days. Residents are motivated to take part in the recreational activities from Monday-Friday and some weekends. The residents enjoy the full afternoon of live music on the last Friday of every month. Some residents go on outings with the OAP social club monthly. A professional physiotherapist and occupational therapist attends the home weekly to assess client’s needs.
They achieve these aims by adhering to HIQA’s standards at all times. They also provide regular training for staff. They also give clients choice of clothing, different food types etc. Residents also have the right to refuse to do some activities, if they don’t want to participate.
Structure of the Organisation
Owner

Manager/ DON

Assistant DON



Administrator
Housekeeping


CNM 1



Head chef
CNM 2
Activities co-ordinator


Staff Nurses
Maintenance

Kitchen assistant
HCA
- Determine the organisations culture and values as demonstrated by management practices and staff client engagement.
My WPO is a family run business. They work on trying to create a ‘home from home’environment for its residents. Sheelin Nursing Home can accommodate up to 38 residents both male and female usually aged 65 and over.
This is a family ran business so it is quite flat in management structure. It has a mission statement explaining that they aim to care for clients using a person centred care approach.
‘Sheelin Nursing Home and its staff are committed to ensuring that the best possible care is given to you or your loved one.
We endeavour to ensure that all aspects of your well-being are catered for (Mental, Physical and Spiritual) in a professional and safe environment. We strive to promote dignity, respect and independence as much as is possible, in an environment that we would hope for you would become a home from home.
Our strong care team are here to support you and each other to ensure that quality care is given with trust and compassion at all times.
With continual investment in staff training we strive to recognise and implement improvements where needed, ensuring that the standard of care given is resident lead and resident centred.’
The culture of the organisation is domiciliary model. They focus on the person not their illness. They care for clients and do their best to make it feel like home. Each client has their own individual care plan.
On clients birthdays they receive a birthday sash to wear for the day. The head chef makes a fresh cake for the client’s birthday, after the dinner we bring out the cake and all staff and other residents join in and sign happy birthday. They then have a little party with tea and music along with the cake. Families are encouraged to be involved and attend these occasions.
The hairdresser attends the nursing home every Thursday allowing people to get their hair done. This will allow people to remain in a routine as they were when they were living at home.
 Mass is held every 3rd Sunday for Roman Catholics, it is also held additionally on holy days. Holy water is always available to residents whenever they want it. Many residents say their own prayers to themselves, they are let finish their prayers before we interrupt them.
Mass is held every 3rd Sunday for Roman Catholics, it is also held additionally on holy days. Holy water is always available to residents whenever they want it. Many residents say their own prayers to themselves, they are let finish their prayers before we interrupt them.
Residents are motivated to take part in the recreational activities from Monday-Friday and some weekends. Residents have the opportunity to take part in many activities. There is bingo, skittles, darts, snakes and ladders, music, hoop games, ball throwing, book reading, listening to music or watching a film.
The residents enjoy the full afternoon of live music on the last Friday of every month. This is where a local singer attends the nursing home to play m usic for the residents. Some of the residents enjoy this as they can sing and dance to their hearts desire. Some residents go on outings with the OAP social club monthly. They take them to different places every month.
usic for the residents. Some of the residents enjoy this as they can sing and dance to their hearts desire. Some residents go on outings with the OAP social club monthly. They take them to different places every month.
A professional physiotherapist and occupational therapist attends the home weekly to assess client’s needs. A chiropodist comes to the nursing home every 2-3 months to do the clients feet.
There is a choice of two meals at dinner time and two more for tea. Residents get their own choice and if they dislike both there is no problem to get something else for them.
 The residents rooms are done up to such a way that their feels they are still at home. Resident’s pictures, cushions, blankets etc. from home are placed in their room to make it feel more like home.
The residents rooms are done up to such a way that their feels they are still at home. Resident’s pictures, cushions, blankets etc. from home are placed in their room to make it feel more like home.
There is a good staff support system from management. Staffs are provided with subsidised meals. There is a service available to get discounts on uniforms for work. Staffs get some in house training of different areas of working in this sector. They receive fire training, infection prevention and control etc. regularly.
Staff are easily approachable as everyone is calmed and relaxed. By speaking to staff it is clear they use a person centred care approach.
Management is easily accessed. Management is available Monday- Friday from 9-5. However if it is necessary management can be contacted outside of these hours by phone for any major issues.
Management runs the place but they also take part in residents care. They have easy access to the work floor. They speak to residents on a regular basis to see if there is anything they would like changed or something they are not happy about.
The work place is very task orientated, we tend to get the work done in the mornings and afternoons so there is time to spend with the residents every evening to see if they are comfortable and just speak to them to see how they are.
 Communication among staff is very good. We all work really well as a team. At the start of the day we organise the tasks the senior care assistant hands out and we share them equally ensuring all work is carried out efficiently.
Communication among staff is very good. We all work really well as a team. At the start of the day we organise the tasks the senior care assistant hands out and we share them equally ensuring all work is carried out efficiently.
When a resident passes away there is a number for any staff to ring if required after the loss to receive bereavement therapy. Family members who lost their loved one are reassured and looked after in the nursing home.
 The WPO operates a policy of openness and honestly, and welcome any feedback from clients or family members to ensure that the services provided are continually reviewed and modified in line with the best practice and resident choice. There is a structured process in place for receiving and acting upon comments, compliments and complaints.
The WPO operates a policy of openness and honestly, and welcome any feedback from clients or family members to ensure that the services provided are continually reviewed and modified in line with the best practice and resident choice. There is a structured process in place for receiving and acting upon comments, compliments and complaints.
The WPO complaints statement and policy is prominently displayed in the nursing home foyer, and if individuals have a complaint or comment the management will aim to respond to the complaint as soon as possible. They encourage family participation in clients care and welcome comments/suggestions from anyone acting on resident’s behalf. They always will of course check if they have resident’s permission.
- Key factors which impact the work practice organisation
- Evaluate the impact of globalisation, new technology and science on the Work Practice organisation.
What is globalisation?
‘Globalization is a process of interaction and integration among the people, companies, and governments of different nations, a process driven by international trade and investment and aided by information technology. This process has effects on the environment, on culture, on political systems, on economic development and prosperity, and on human physical well-being in societies around the world.’
 http://www.globalization101.org/what-is-globalization/
http://www.globalization101.org/what-is-globalization/
Global Health
The Irish Forum for Global Health (IFGH) is an independent network of people. This group of people are concerned looking at a global level of the heath and development of populations. They are particularly concerned with populations that live in low income countries.
The IFGH was established in 2004. There are over 800 members in the committee. The IFGH welcomes any individuals or groups who have an interest in promoting global health related education, research, policies and advocacy.
The IFGH offers their members many opportunities for learning, collaboration and action in these areas. This works in order to create and improve national and international links that are within the global health community.
The Irish Forum for Global Health aim for a healthy global society free of poverty, inequity and social injustice. Their mission is to create and sustain community of individuals, sectors and organisations in Ireland. They are collaborating to improve global health and recognising health as a basic human right. They strive to achieve equity of access and quality in healthcare for all. They are promoters of gender equality and social development. They work with different partners and advocate and collaborate for sustainable development.
https://globalhealth.ie/about/
My WPO is not part of the global company but is a part of the global health services.
There are many global issues in relation to health.
Some of these disease/ illnesses are:
- Cancer
- Diabetes
- Obesity
- High cholesterol
- Cardiovascular disease
- AIDS/ HIV
- Malnutrition
- Tuberculosis
- Meningitis
- Malaria
- Sepsis
- Pneumonia
The two major diseases that I am going to speak about is Alzheimer’s and high cholesterol.
Alzheimer’s:
Dementia is described by the World Health Organisation as “…a syndrome due to disease of the brain, usually of a chronic or progressive nature, of which there is impairment of multiple higher cortical functions…”
The symptoms of dementia are caused by a number of conditions that affect the cerebral cortex of the brain. These symptoms affect the cognitive functions such as thought, memory, understanding, perception and logic. The symptoms also affect the sensory functions like hearing, seeing, touching, tasting and sense of smell.
There are over 400 types of dementia; Alzheimer’s being the most common form. 60-80% of dementia cases accounts for Alzheimer’s. This is not a normal part of aging however it is the greatest risk factor. Most people with Alzheimer’s are 65 years or older.
It is not just associated with old age, 200,000 Americans under 65 have early onset Alzheimer’s. This disease worsens over time. It is known as a ‘progressive’ disease where the symptoms gradually worsen over a number of years. It is also the 6th leading cause of death in the USA.
People who suffer with Alzheimer’s live an average of 8 years. However survival can range from 4-20 years depending on the persons age and other health conditions.
Alzheimer’s has no cure but there are treatments that you can get to reduce the effect of the symptoms of the disease.
According to Irish Health Alzheimer’s disease will reach ‘epidemic proportions within 40 years unless new therapies can be developed.’
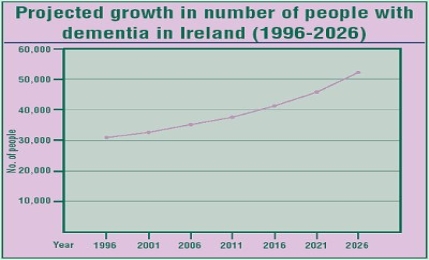
Following studies Alzheimer’s and related dementia currently affects around 38,000 people in Ireland. Due to Ireland’s rapidly ageing population, that number is predicted to rise to 58,000 by 2021 and 104,000 by 2036.
Alzheimer’s disease is the most common form of dementia. This is a progressive and irreversible disease of the brain; it causes loss of intellectual function, chronic memory loss, language deterioration and personality change.
Short term memory is usually one of the earliest signs of Alzheimer disease.
Internationally, while death rates declined for most major diseases including heart disease and stroke between 2000 and 2004, Alzheimer’s deaths increased by 33%.
Prof Brian Lawlor, consultant psychiatrist for the elderly at St Patrick’s and St James’s, told a recent conference that unless awareness of the disease is increased and the state funds research and innovation on cause, care and cure, Alzheimer’s disease will cause a global health crisis.
He also stated that “Unless disease modifying treatments that delay the onset of the disease or its rate of progression can be developed, by 2050 one in 85 people will have Alzheimer’s disease. More than 40% of cases will require a high-level of care, and the burden of caregivers will also have a huge impact on the healthcare system.”
http://www.irishhealth.com/article.html?id=13433
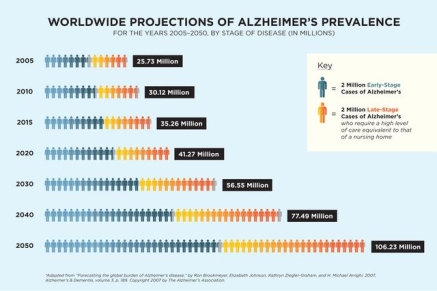
Someone in the world develops dementia every 3 seconds. In 2015, there was an estimated 46.8 million people worldwide living with dementia. In 2017 this number is believed to be close to 50 million people. These numbers will almost double every 20 years, reaching 75 million in 2030 and 131.5 million in 2050. Much of the increase will be in developing countries. 58% of people with dementia live in low and middle income countries, but by 2050 this is said to rise to 68%. The fastest growth in the elderly population is taking place in China, India, and their south Asian and western Pacific neighbours.
Ageing is a worldwide process that shows how successful health care has been over the last century. Many people are now living longer and healthier lives and so the world population has a greater population of older people. Dementia mainly affects older people, although there is a growing awareness of cases that start before the age of 65.
There are over 9.9 million new cases of dementia each year worldwide.
The World Alzheimer Report 2015 updates ADI’s global estimates of the prevalence, incidence and costs of dementia based on systematic reviews. The report makes key recommendations to provide a global framework for action on dementia. The report also includes a review of the evidence for and against recent trends in the prevalence and incidence of dementia over time, as well as an analysis of the broader societal impact of dementia.
The total estimated worldwide cost of dementia is US$818 billion in 2015, which represents 1.09% of global GDP. By 2018, the global cost of dementia will rise above a US$ trillion.
This figure includes costs attributed to informal care (unpaid care provided by family and others), direct costs of social care (provided by community care professionals, and in residential home settings) and the direct costs of medical care (the costs of treating dementia and other conditions in primary and secondary care).
Direct medical care costs account for roughly 20% of global dementia costs, while direct social sector costs and informal care costs each account for roughly 40%. The contribution of informal care is greater in the African regions and lowest in North America, Western Europe and some South American regions, while the reverse is true for social sector costs.
https://www.alz.co.uk/research/statistics
This relates to my WPO as we as carers look after older people in resident settings. Some of these people either have dementia or it is slowly progressing.
High Cholesterol:
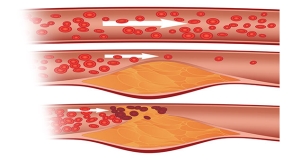
Cholesterol is a waxy substance that’s found in the fats in your blood. Your body needs cholesterol to build healthy cells, having high cholesterol can increase your risk of heart disease.
When you have high cholesterol, you may develop fatty deposits in your blood vessels. These deposits make it difficult for enough blood to flow through your arteries. Your heart may not get as much oxygen-rich blood as it needs, this increasing the risk of a heart attack. Decreased blood flow to your brain can cause a stroke.
High cholesterol can be inherited, but it’s often the result of unhealthy lifestyle choices, and meaning it can be preventable and treatable. A healthy diet, regular exercise and sometimes medication can go a long way toward reducing high cholesterol.
Serum Cholesterol levels in normal Irish adults: Age and
Gender distribution.
MAL ES FEMALES TOTAL
Age N Mean (sd) N Mean (sd) N Mean (sd)
<25 74 4.47 (0.88) 77 4.31 (0.83) 151 4.39 (0.86)
25-34 147 4.99 (1.00) 113 4.44 (0.77) 260 4.75 (0.95)
35-44 189 5.46 (0.96) 95 4.92 (0.76) 284 5.28 (0.93)
45-54 139 5.46 (0.92) 50 5.67 (I.10) 189 5.52 (0.94)
55-64 55 5.67 (0.96) t5 6.20 (0.81) 70 5.78 (0.95)
TOTAL 604 5.24 (1.01) 350 4.79 (0.98) 954 5.08 (1.02)
https://link.springer.com/article/10.1007%2FBF02940246
Researchers in the Mater Hospital in Dublin carried out a study into cholesterol levels of 1,000 people. They expected Irelands level of cholesterol would be high than the US and UK. However their findings showed the opposite.
The average cholesterol among the Irish is ‘high’. Dr Declan Sugrue from the Mater Hospital and his colleagues carried out this study of ‘Cholesterol Levels in Normal Irish Adults the Mater Hospital Cholesterol Screening Survey’. This was published in the Irish Journal of Medical Science.
The average level of serum cholesterol for men and women aged 25-65 in the study was 5.1 mmol/l. For men aged 55-64 years, the average was 5.7 mmol/l. For women aged 55-64 years, the mean level was 6.2 mmol/l.
Dr Sugrue describes these levels as being “not too bad“. However some experts would say that 5.7 mmol/l for a man in his late 50s to early 60s is far too high. At the other extreme, there are experts who believe the importance of cholesterol levels has been exaggerated.
Dr Sugrue, says the survey results are encouraging because they indicate cholesterol levels may be dropping slightly. The reason for the decline remains unproved, but Dr Sugrue tends to agree with the moderate view that two factors are equally at play improved diet and medical technologies such as bypasses.
https://www.irishtimes.com/news/health/cholesterol-count-1.77993
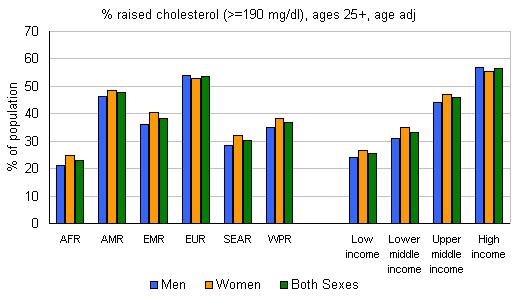
Having high cholesterol increases the risks of heart disease and stroke. A third of people with heart disease is because high cholesterol. Having high cholesterol is estimated to cause 2.6 million deaths (4.5% of total) and 29.7 million disability adjusted life years (DALYS), or 2.0% of total DALYS. High cholesterol is a major cause of disease in the developing world and the developed world. A 10% reduction in cholesterol in men aged 40 has been reported to result in a 50% reduction in heart disease within 5 years; the same cholesterol reduction for men aged 70 years can result in an average 20% reduction in heart disease occurrence in the next 5 years. In Ireland, a 30% reduction in the heart disease death rate has been attributed to 4.6% reduction of the population mean for total cholesterol. In Finland, 50% of the decline in IHD mortality has been explained by the reduction of population blood cholesterol level.
In 2008 the global prevalence of raised total cholesterol among adults (≥ 5.0 mmol/l) was 39% (37% for males and 40% for females). Worldwide the total cholesterol changed little between 1980 and 2008, falling by less than 0.1 mmol/L per decade in men and women.
The total cholesterol was highest in the WHO Region of Europe 54% for both male and female. This then followed by the WHO Region of the Americas which was 48% for both male and female. The WHO African Region and the WHO South East Asian Region showed the lowest percentages of 22.6% for AFR and 29.0% for SEAR.
http://www.who.int/gho/ncd/risk_factors/cholesterol_text/en/
High cholesterol is relevant to my WPO as there are a large group of residents in the nursing home with high cholesterol which is why it is important that we know about it.
In my WPO there are different forms of communication. We use email, internet, Skype and the phone.
A lot of residents use the phone to contact their families on a daily basis. Some clients use Skype to see family that is moved abroad.
New Technology:
There have been huge advancements made in technology over the past few years especially in the healthcare sector.
 Sensor pad:
Sensor pad:
Sensor pads can be used on chairs and beds it helps us keep track of the movement of a person. An alarm is activated if the person moves from the bed or chair to leave. This alarm usually is to alert a local carer.
These pads can also be placed at doorways so they will be alarmed if there is a risk of someone wandering or trying to exit the building.
More advanced sensor mat systems to prevent wandering can be connected to an auto-dialler which uses a regular landline to alert up to 6 pre-selected phone numbers. Each number is dialled in turn until an answer is received and the alarm de-activated. The systems are able to differentiate between an answer-phone message and a live response.
https://www.homecaretechnologies.ie/index.php/blog/37-sensor-pads-and-mats
This sensor mat relates to my WPO as a couple of confused clients tend to try and walk by themselves or get out of bed even though they are not mobile.
Electric beds:
Electric beds are another technology that has benefitted the healthcare industry. These beds can move top and bottom and be lowered and raised.
 This benefits everyone in a few ways. It improves the client’s circulation as their head and legs can be raised at any time. The bed also reduces the chance of pressure sores, excess fluid in the legs and back and joint strains.
This benefits everyone in a few ways. It improves the client’s circulation as their head and legs can be raised at any time. The bed also reduces the chance of pressure sores, excess fluid in the legs and back and joint strains.
Electric beds provide comfort for the patient. They allow for patients to change position for different tasks such as reading, watching and eating. These are all easily done from the bed without any physical effort, keeping the patients supported and comfortable.
Being a carer can be physical work at times, but thankfully due to the electric beds carers can now position clients more easily and also change dressings easily. This prevents less back injuries.
https://www.beechfieldhealthcare.ie/blog/post/5-benefits-of-an-electric-bed/
Science Breakthrough:
Alzheimer’s:
In 2017, the Alzheimer’s Drug Discovery Foundation made 29 new grants. This totalled to 16.6 million. This gives hope to people that is living with the disease and also breakthroughs for researchers that are working to find a cure. In 2017 they invested more of their resources in clinical trials, because other drug programs have made it that far.
The ADDF have made better biomarkers. These biomarkers are used to diagnose diseases, monitor their progression and help develop drugs for them. Very few biomarkers exist when 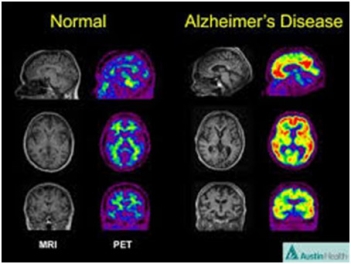 it comes to Alzheimer’s. This effecting drug development and may also cause patients to be misdiagnosed.
it comes to Alzheimer’s. This effecting drug development and may also cause patients to be misdiagnosed.
The ADDF help to support the first biomarker to diagnose this disease. It is called the ‘beta-amyloid PET scan’; they still continue to invest in these.
In 2017 they also supported blood tests for Alzheimer’s along with Dr. Sam Gandy (funded investigator) that were being developed at the Florey Institute in Australia along with the University of Calgary in Canada. This made great progress in his development of the PET scan to diagnose chronic traumatic encephalopathy in living patients.
www.alzdiscovery.org/news-room/blog/top-five-alzheimers-advances-in-2017
High cholesterol:
 A new class of LDL cholesterol lowering drugs are expected to be disruptors by next year.
A new class of LDL cholesterol lowering drugs are expected to be disruptors by next year.
These drugs are expected to lower cholesterol dramatically to abnormal levels.
The new class of drug is expected to lower levels by 75% when taken with a statin cholesterol lowering drug.
 Another innovation in 2017 was a small interfering RNA therapy to help lower LDL too. These were only given twice a year instead of the usual monthly or weekly dosages.
Another innovation in 2017 was a small interfering RNA therapy to help lower LDL too. These were only given twice a year instead of the usual monthly or weekly dosages.
Dr. Leslie Cho of the Heart and Vascular Institute in Cleveland says that we will continue to see a new class of drugs to lower LDL levels in 2018.
According to Dr. Cho she says that these statin drugs could be available over the counter someday.
- Review the impact of relevant government policy on the Work Practice Organisation.
 Fair deal scheme:
Fair deal scheme:
This scheme is operated by the Health Service Executive (HSE). It is a service that provides people with financial support that requires long term nursing home care.
 With this scheme the person that requires care makes a contribution towards the cost of care and that State pays the remainder. This scheme covers private nursing homes, voluntary nursing homes and public nursing homes. A list of approved nursing home can be found from the HSE.
With this scheme the person that requires care makes a contribution towards the cost of care and that State pays the remainder. This scheme covers private nursing homes, voluntary nursing homes and public nursing homes. A list of approved nursing home can be found from the HSE.
Anybody who is a resident in the State and gets the assessment resulting in them needing long term care can apply for this scheme.
During the assessment your care needs are assessed to confirm that you require long term nursing home care.
Your finances will also be assessed to see how much you will have to contribute to your own care. If your contribution is less than the sum of the fees the HSE pays the remainder.
When assessing your finance any savings and property is also taken into account. If you want to defer making the part of your contribution that is based on your home or other you can apply for the Nursing Home Loan.
This scheme only covers long term care it does not cover short term care. Long term care is defined in the act as maintenance, health and personal care services. The Department of Health has further clarified that this includes: bed and board, nursing and personal care that is appropriate to the level of care needs of that person.
Safeguarding Vulnerable Persons at Risk of Abuse 2014:
 Everyone has the right to be safe and live a life with no abuse. It is the service provider’s responsibility to make sure that service users receive support, and get treated with respect and dignity. It is important that every effort is made to promote welfare and to prevent abuse.
Everyone has the right to be safe and live a life with no abuse. It is the service provider’s responsibility to make sure that service users receive support, and get treated with respect and dignity. It is important that every effort is made to promote welfare and to prevent abuse.
This policy applies to all HSE and HSE funded services. It also outlines a number of principles to promote the welfare of these vulnerable people and safeguard them from abuse.
 All services must have a ‘No Tolerance’ approach that is publicly declared.
All services must have a ‘No Tolerance’ approach that is publicly declared.
Some of the principles are as follows:
- Respect for human rights
- A person centred approached to care and services
- Promotion of advocacy
- Respect for confidentiality
- Empowerment of individuals
- A collaborative approach
There are many different forms of abuse:
- Physical abuse
- Sexual abuse
- Psychological abuse
- Financial or material abuse
- Institutional abuse
- Neglect and acts of omission
- Discriminatory abuse
https://www.hse.ie/eng/about/who/socialcare/safeguardingvulnerableadults/
- Assess if social or ethical issues have affected the Work Practice organisation or may impact in the future.
 From carrying out my placement I can say all staff and residents are treated equal and there is no discrimination between race, religion or gender etc. Clients that are mobile are kept on the middle floor, whereas immobile clients are located on the bottom and top floor. Independent clients can go themselves to any part of the building.
From carrying out my placement I can say all staff and residents are treated equal and there is no discrimination between race, religion or gender etc. Clients that are mobile are kept on the middle floor, whereas immobile clients are located on the bottom and top floor. Independent clients can go themselves to any part of the building.
Client’s privacy and dignity is upheld as we always used the person centred care approach. We see the person not the illness. We try and get the person to remain as independent as they can. We do this by
letting them choose their own clothes, washing their face and teeth in the mornings etc.
Families are encouraged to visit regularly and take part in any occasions such as birthdays etc. This allows the family to be involved in the care of their family member.
 In my WPO restraints are not used. There is no tolerance for elder abuse either. When a person comes to needing end of life care they are moved to a separate large room. This gives the family time to spend time with the person in private.
In my WPO restraints are not used. There is no tolerance for elder abuse either. When a person comes to needing end of life care they are moved to a separate large room. This gives the family time to spend time with the person in private.
During admission and reviewing care plans clients are asked if they want to sign a DNR.
The aging population is putting huge pressure on the healthcare system. The population of Ireland is expected to increase by 14 to 23% adding 640,000 to 1.1 million people;
The population aged 65 and over is expected to increase from one in eight to one in six;
The total amount of people aged 85 and older is expected to double.
The demand for health and social care is expected to increase across all sectors; however the most that increased would be for older people.
The demand for home care and for residential care places in nursing homes and other settings is expected to increase by up to 54 per cent.
- Comment on any impact to the Work Practice organisation in relation to economic and population shifts.
The Irish health system is experiencing unprecedented reductions in public Spending. Cuts to the health budget are compounded by underlying cost pressures,
Some caused by weaknesses in the health system (high salaries, high drug prices, poorly developed primary care, means-tested benefits), some caused by factors beyond the health system’s control (substantial population growth, economic recession).
So far, cuts in public spending on health have been mainly achieved through reduced pay for staff, improved efficiency in service delivery and, to a lesser extent, increases in the financial burden falling on users.
Although there is scope to make substantial additional savings through efficiency gains, these cannot be made within the required timeframe without damaging patient care, unless high salaries and the high price of other inputs are seriously addressed.
If this is not feasible, the Government should consider establishing a mechanism to compensate the Department of Health and the Health Service Executive for unavoidable increased demand for health and long-term care.
Bibliography
- nursing home ireland. (2012). Key Facts. Available: http://www.nhi.ie/index.php?p=key-facts. Last accessed 13/08/18.
- (2018). HIQA. Available: https://www.hiqa.ie/about-us. Last accessed 16/08/18.
- www.sheelinnursinghome.ie
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Healthcare"
Healthcare is defined as providing medical services in order to maintain or improve health through preventing, diagnosing, or treating diseases, illnesses or injuries.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




