Correlation between Mental Health and Obesity
Info: 9118 words (36 pages) Dissertation
Published: 8th Jun 2021
Tagged: HealthNutritionMental Health
Correlation between Mental Health and Obesity in West Virginia
Abstract
West Virginia has consistently suffered from the highest rates of obesity and mental health in the United States. The population has been affected by longstanding socioeconomic disparity impacting the treatment of both physical and mental well-being. This study seeks to find a connection between mental health and obesity in West Virginia by examining confounding social and economic factors and provide a recommendations to begin to remedy this public health epidemic.
I. Introduction
West Virginia has the highest percentage of adults in the United States who are overweight or obese. In a survey done by the West Virginia Department of Health and Human Resources’ Division of Health Promotion and Chronic Disease in 2014, approximately 17.1% of adults reported poor physical health for at least 14 days in the last 30, as well as 15.5% of respondents reporting poor mental health for at least 14 of the last 30 days. Both statistics are significantly higher than the national prevalence, 12.1% and 11.4%, of each category. (Yabolonsky, 2017) From these statistics, it is seen that a significant portion of West Virginia’s population suffers from poor mental and/or physical health. This study seeks to answer the question of whether there is a link between obesity and mental health, and if so, why is there such a prevalence in West Virginia and what steps can be taken to remedy the problem. For the purposes of this study, obesity will be viewed as the physical result of an underlying mental health issue. Confounding social factors contributing to the impact of this public health issue for the state will be explored and analyzed for possible solutions to this problem.
For an individual to be classified as obese, they must have a body mass index (BMI) of 30 or higher. BMI measures body fat as a function of height and weight. Obesity contributes to an increased risk for chronic diseases, such as cancer, heart disease, and diabetes. (Amarasinghe et al., 2009) According to the 2016 West Virginia State Nutrition, Physical Activity, and Obesity Profile from the CDC’s Division of Nutrition, Physical Activity and Obesity, 34% of adults were overweight, 35.7% adults were obese, 15.5% of adolescents were overweight, 15.6% of adolescents were obese, 13.7% of children aged 2-4 in the WIC program were overweight, and 14.1% of children aged 2-4 in WIC were obese. (CDC, 2016)
A 2016 study investigating mental distress and functional health reported that West Virginia had the highest prevalence of reported limitation due to physical, mental, or emotional problems at 29.1% ± 0.7. (Charara et al., 2016) As stated previously, 15.5% of West Virginian adults reported having poor mental health for 14 of the last 30 days. Road to Recovery, a gateway program to mental health services, reports that only 46.9% of adults with mental illness diagnoses in West Virginia receive any type of treatment from the public health system or from private health care providers. The remainder of those with mental illness receive no mental health treatment. According to Mental Health America, West Virginia is 43rd in the nation in providing access to mental health services. (Laurel House, Inc., 2017) Rates of obesity and depression in the United States have continued to steadily increase. A 2017 study investigating the relationship between these two conditions found that there is a positive relationship between obesity and depression. Two findings of this study were that those who are obese are more likely to develop new-onset depression and vice versa, and as obesity worsens, so too does depression. Comorbid obesity and depression present increased levels of morbidity and disability than either on its own. They also exhibit the same health impacts, such as cardiovascular disease, and have interdependent negative effects on treatment compliance and quality of life. (Ma et al., 2017) According to the SAMHSA Behavioral Health Barometer for West Virginia in 2015, 5.5% of adults have a serious mental illness diagnosis, above the national average of 4.2%. (SAMHSA, 2017)
The cost of care for those who are obese is also placing a burden on the state. The following tables break down spending on health care in West Virginia due to obesity:
| Table 1: Obesity-Attributable Healthcare Spending in West Virginia (per Adult) | ||
| 2008 | 2013 | 2018 |
| $479 | $764 | $1,736 |
(WV DHHR, 2017)
| Table 2: Obesity-Attributable Healthcare Spending in West Virginia
(Millions of Dollars) |
||
| 2008 | 2013 | 2018 |
| $668 | $1,076 | $2,384 |
(WV DHHR, 2017)
According to The State of Obesity, obesity among the adult population has the following economic impacts: $1.4-$1.8 billion in preventable medical cost with half of these costs being for Medicare and Medicaid, another $5 billion in indirect costs; obese adults have a 42% increase in spending on direct health care; morbidly obese costs are an 81% increase over those of healthy adults; obesity costs employers $506 per obese worker per year; and medical claims costs for obese workers are $51,091, compared to $7,504 for healthy workers. (WV DHHR, 2017)
The public health epidemic of obesity in West Virginia is the complex result of several economic, social, and psychological factors. This study will narrow its focus to how the economic, social, and psychological factors all compound together into neglecting one’s personal health to the point at which they become obese. To address the economic stressors in the state, the problems created by low-income and poor access to care must be investigated. For people in West Virginia to view their personal health as an important component to maintaining a higher quality of life, the social paradigm must be shifted, and this can be done through community intervention and programs in the public education system. Lastly, psychological factors can be addressed as the result of correcting the social and economic conditions in West Virginia. These factors have an interdependent effect on an individual’s physical health (Fig.1.)
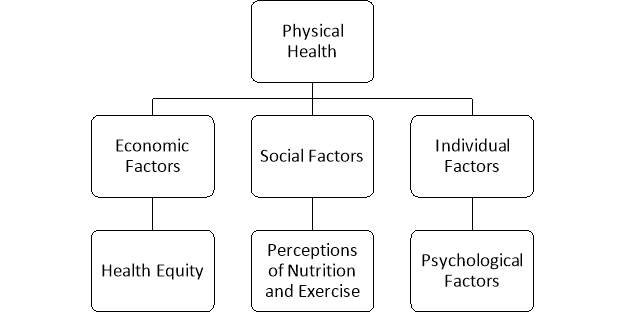
Figure 1: Confounding Factors on an Individual’s Physical Health
The first factor to address is economic stressors on West Virginians. According to the Appalachian Regional Commissions findings on “Disparities and Bright Spots” in 2017, the median household income in West Virginia is 25% lower than the national average, the household poverty rate is 18.4%, higher than the national average 15.6%, 9.1% of West Virginians receive disability benefits where the national average is 5.1%, and only 53.1% of adults between 25 and 44 have some post-secondary education, lower than the national rate of 63.3%. Also, the percentage of uninsured people under the age of 65 is 17.1%, higher than the national average of 16.8%. With respect to access to care, West Virginia is 3% higher than the national average in primary care physicians per 100,000 people, 21% lower than the national average in specialty physicians per 100,000, and 45% lower than the national average in mental health providers per 100,000. (Appalachian Regional Commission, 2017) With the number of uninsured people in West Virginia being higher than the national average, it can be inferred that seeking medical care, both for treatment and preventative reasons, is difficult for a significant portion of the population as those who are uninsured are also often unable to afford out-of-pocket costs for care. There is also a correlation in greater physical and mental health and levels of education. Those who have a post-secondary education are less-likely to suffer from chronic diseases and will be able to seek medical care when needed. (Knickman & Kovner, 2015)
Addressing social factors may be more difficult than addressing economic factors. These result from long-standing perceptions about lifestyles. They are part of the culture. However, the most accessible vessel for addressing these factors is education. The health curriculum in the public education system stands as one of the largest potential solutions to the obesity problem in West Virginia by shaping students’ outlooks on exercise and nutrition from an early age. In the CDC report on nutrition, physical activity, and obesity in West Virginia it was found that 39.4% of adolescents reported eating fruit less than once per day, 37.5% eat vegetables less than once per day, 31.0% were physically active for at least one hour per day for the previous week, 15.5% were overweight, and 15.6% were obese. (CDC, 2016) For the adult population, community level interventions through the county health departments would provide support for individuals who are overweight or obese and access to resources to help them remedy their conditions.
The final piece of the problem is to address the resulting mental states created by the combination of economic and social factors. Chronic stress can lead to deteriorating physical and mental health. As stated previously, 15.5% of West Virginian adults reported having poor mental health for 14 of the last 30 days, with only 46.9% of those with mental health diagnoses receiving treatment. With West Virginia being 45% lower than the national average in access to mental health services, the state is at risk for a large-scale mental health problem as West Virginia residents are less likely to receive the care that they need in order to manage any mental health diagnoses or to simply cope with stress cause by any number of the previously mentioned social and economic factors. Using depression as an example, a study mentioned previously showed that those who are overweight or obese are more likely to develop new-onset depression, and vice-versa, and as obesity worse, depression worsens as well.
Unfortunately, obesity has become a frontrunner in public health concerns in West Virginia over the past few decades. However, by addressing the above factors collectively, the impact of obesity and chronic conditions that result from it can be lessened and, over time, the damage can be repaired.
II. Policy Evaluation/Alternatives
Action can be taken to address the concerns regarding obesity and mental health by reevaluating policies and standards that could be contributing to the declining health of the population in West Virginia. As prior stated, economic, social, and psychological factors are all relative in the contribution to the obesity epidemic in the state. Changing current policies within the state could create a positive series of events that could lead to the decline of the overwhelming obesity population.
With a large portion of the state’s population living in poverty or close to poverty, it can be assumed that a large portion of the state’s population also qualifies for food assistance from the state in the form of the Supplemental Nutrition Assistance Program (SNAP). According to the United States Department of Agriculture, there are 34,269 households who receive benefits from the Supplemental Nutrition Assistance Program in West Virginia. (United States Department of Agriculture, January 2017)
Currently, any food item within a grocery store that can be brought home for consumption can be purchased with SNAP benefits. There is no limit to what types of food they can purchase monthly. This can include candy, energy drinks with nutritional labels, soda, and processed foods. (United States Department of Agriculture, 2017) One policy alternative would be to limit the amount of unhealthy foods a SNAP household can purchase monthly. A study conducted by the United States Department of Agriculture showed that sugary beverages, frozen prepared foods, and prepared desserts were part of the top 5 categories purchased by SNAP benefit recipients. (United States Department of Agriculture, 2016) A gradual reduction in amount of benefits used on unhealthy food and drink options over the course of 5 years could be beneficial in fighting obesity. In the first year, limit the amount of unhealthy foods purchased to 70% of benefits received. Decrease the amount of unhealthy purchases a SNAP recipient can make in a month by 10 percent yearly. By the end of the five-year transitional period, the ability to purchase unhealthy food options would be reduced to 30% of the allotted benefits. By doing so, this would gradually introduce a healthy lifestyle change into the program to help beneficiaries transition. Reducing the amount of unhealthy purchases one can make would encourage recipients to purchase healthier food options that would lead to a better diet. If implemented in West Virginia, it could encourage other states to do the same and start a movement that has the possibility to reduce obesity across the entire country. This alternative could possibly overstep a boundary in regards to an individual’s right to freely choose what they feel is the best diet for their family.
According to the West Virginia Department of Health and Human Resources, 35 out of West Virginia’s 55 counties have farmer’s markets that accept SNAP benefits (West Virginia Department of Health and Human Resources, 2016) Extending the amount of farmer’s markets that accept SNAP benefits would provide benefit recipients with another option in purchasing healthy food alternatives. As previously stated, roughly 38% of adolescents reported eating less than one serving of fruits and one serving of vegetables daily. (CDC, 2016) If the state could provide every local farmer’s market in the state with the equipment to accept Electronic Benefit Transfer (EBT) cards, it would increase the access to locally grown foods for the benefit recipients. Introducing an incentive program to SNAP benefit recipients who shop at local farmer’s markets could encourage them to purchase more locally grown fruits and vegetables. For example, providing an extra 10 dollars a month to be used in a local farmer’s market would encourage recipients to buy from farmer’s market so that they can obtain an extra 10 dollars’ worth of food for their family. Providing such an incentive to each household that receives benefits could potentially cost the state an extra four million dollars a year. This could lead to a reduction of people who are able to receive benefits to make up for the difference.
Diet isn’t the only contributing factor to obesity within the state. Key findings from the Appalachian Regional Commission state that 32 percent of the West Virginia population states that they are physically inactive. That is 10 percent higher than the United States. (Appalachian Regional Commission, 2017) As it stands, there is a limited amount of physical education taught to school aged children in West Virginia. Elementary aged children are only required to have 90 minutes of physical education. Middle school children have a daily requirement of physical education for at least one semester. In high school, a student must earn one physical education credit in order to graduate with his/her diploma. (Shape of the Nation | State Profile, 2016) One can infer that there is little amount of physical education within the curriculum of West Virginia. Improving these policies could help increase the amount of physical activity school aged children receive.
Changing the amount of physical education can start at the yearly level. Requiring West Virginia to enforce a year-round physical education policy for every grade can help keep students active for more than just a portion of the school year. Regarding the amount of time spent on physical education, change would be needed at the elementary, middle, and high school level. Increasing the amount of physical education at the elementary aged level by one hour would increase the time spent to 150 minutes. This would ensure that there is at least 30 minutes of physical education being taught at the elementary aged level. Middle school requirements differ slightly. Requiring an increase from daily for one semester to three times a week every semester would give students a break every other day, but continue physical education throughout all middle school years. Increasing the credit requirement for graduation from 1 credit to 1 credit for each grade level would ensure that students are participating in physical education at least one semester every year of high school. Going one step further and implementing the need for strength and aerobic exercise within each physical education course would help the state align more with Healthy People 2020 objectives. (“Physical Activity | Healthy People 2020,” 2017) The increased amount of physical activity provided by changing these policies could lower the number of children, grades K-12, who are considered obese. This could help condition them to exercise regularly so that they continue these healthy behaviors beyond these school years. Providing this much physical activity could also reduce the risk of mental health disorders for children this age. A study found in the American Academy of Pediatrics News & Journals suggests that there is a positive correlation between physical activity and mental health in the younger population. Participating in physical activity can improve a child’s self-esteem, therefore having a positive influence on their overall mental health. (Biddle et al., 2016) The amount of physical education this alternative provides could take away from necessary curriculum already implemented in West Virginia. This much physical activity could also have an adverse effect on school aged children and make them grow tired of it, causing them to not want to take part in physical activity after high school.
More than twenty chronic diseases can be contributed to obesity. These include diabetes, heart disease, high cholesterol and hypertension. A high Body Mass Index (BMI) puts individuals at risk for many health complications. (“STOP Obesity Alliance,” 2017) One can infer that if the obesity epidemic can be reduced, the reduction of other chronic diseases would soon follow.
The Cabell-Huntington Health Department currently has a Chronic Disease Self-Management Program in place to help individuals succeed in management of their chronic diseases. The program length is 6 weeks and requires a weekly 2-hour meeting over the course of the program. It is led by two leaders who are trained in managing chronic diseases. Some of the topics covered within the program are nutrition, medication, decision making, and ways to deal with the frustrations that are associated with chronic diseases. (Cabell-Huntington Health Department, 2017) Restructuring this program to focus solely on obesity could, in turn, have a positive effect on the other chronic diseases that this program strives to manage. Utilizing coordinated care between a doctor, nutritionist, psychologist, and fitness coach could increase the success of the program because all of these are aspects of obesity that should be addressed and discussed between all health professionals to provide the best support possible for program participants. Structuring the program so that it follows the transtheoretical model stages of change could prove to be effective. A study conducted by the Cochrane Metabolic and Endocrine Disorders Group showed that using transtheoretical model stages of change had positive effects on dietary habits and physical activity. Although weight loss because of using this model was inconclusive, the positive effects along with the utilization of coordinated care could provide the program enough resources to help participants reverse their obesity. (Garasky, Mbwana, Romualdo, Tenaglio, & Roy, 2016) The program length should be increased to 16 weeks and meet at least 3 times a week to ensure that all program participants are following the advice from their coordinated care professionals. This also ensures that if problems arise or the participant has any questions, they won’t need to wait a week before seeking help. Increasing the length by 10 weeks would also ensure that the practices learned are maintained longer. Therefore, it will be easier for a participant to transfer the knowledge learned to life after the program ends. The redesigned program would strive to reduce the number of people with obesity by giving them the necessary knowledge and tools to help reach their weight loss goal.
With the increased amount of time that would need to be dedicated to this restructured program, people might not have the time to dedicate to it. This could lead to a decreased amount of participants willing to enroll in the program; therefore, limiting the amount of individuals that receive obesity counseling. According to the Centers for Disease Control, approximately 10.5 percent of the grants allotted to chronic disease prevention and health promotion in West Virginia are used on nutrition, physical inactivity, and obesity. (Centers for Disease Control, 2016) If this alternative program is implemented, the state would need to reevaluate their grant distribution to allow for more money to be used on the promotion of nutrition, physical activity, and obesity.
According to the United States Department of Agriculture, roughly 700 thousand people in West Virginia live in a rural area. Only 15 percent of the 700 thousand have a college degree, and 18.7 percent are living in poverty. (United States Department of Agriculture, 2016) As previously stated, the presence of chronic diseases is less regarding individuals who have post-secondary education and these same individuals are more often able to pursue medical care if needed. (Knickman & Kovner, 2015) A study completed by the World Health Organization shows that poor mental health can happen at any time in life and can be attributed to a combination of economic, social, and physical environments. The greater inequality an individual has, the greater the risk for a mental health disorder. (WHO and the Calouste Gulbenkian Foundation, 2014) While trying to provide access to care for the rural communities, one of the hardest types of care to provide is mental health. More often, primary care physicians try to take on mental health responsibilities, but often are challenged with low financial reimbursement and little time to provide appropriate care to these rural patients. (“Healthcare Access in Rural Communities Introduction – Rural Health Information Hub,” 2017) Obesity as a result of depression and vice versa has already been previously discussed, so the need to address all of these compounding factors is greatly needed.
Access to care, as well as what types of care are provided, are greatly needed to increase the health of the rural population in West Virginia. The Health Wagon is a mobile health unit that provides care to rural populations in southern Virginia. They provide services such as primary, preventative, mental, and dental care. In addition to providing care within the mobile unit, they also offer telemedicine as a means of providing their patients with an alternate form of care. The Health Wagon asks every patient to make a ten-dollar donation as part of their visit, but is unnecessary if unable to do so because the services they provide are free. Most of their patients make too much to qualify for Medicaid, but too little to purchase private insurance on their own. They provide a patient centered medical service to the rural communities that they wouldn’t otherwise have this type of access to care. (“About Us: The Health Wagon,” 2017) Implementing mobile services like The Health Wagon to rural areas of West Virginia could greatly improve the overall health of the population. By providing mobile services instead of immobile clinics, this would give the ability to freely travel to areas who are in need of medical care the most. This would insure that all parts of the rural community in West Virginia would have the ability to access care that otherwise wouldn’t be available to them. In turn, obesity and mental health within this population could be addressed and monitored regularly. This would help the obesity epidemic in West Virginia, as well as mental health well-being for the undeserved population.
The ability to start a mobile health program like this would require donations or grant funding to get started. There could also be a lack of interest from medical providers in the area to participate in this kind of program due to the lack of profitability that is associated with serving a low-income population. The resistance from such providers could doom the mobile program before it ever has a chance to get started. As one can see, many alternatives to programs and policies already implemented could help reverse the obesity epidemic in West Virginia and improve mental health. In turn, this could greatly reduce other chronic diseases and healthcare expenditures within West Virginia.
III. Recommendations
An effective way to address the physical and mental health issues plaguing West Virginian is through statewide public assistance programs policy changes. Poor nutrition decisions are a major cause of problems for many of the health issues reportedly being treated here. The government Supplemental Nutrition Assistance Program (SNAP) should be restructured so its recipients can only purchase food meeting favorable nutritional value criteria. Participation in a thirty-minute health nutrition education class yearly would be a stipulation for all new recipients and for those who currently enrolled in the program to receive benefits. This mandatory class presents a perfect opportunity to offer SNAP program users important information for making good food choices and allowing them to ask questions about food purchase practices. A survey report from the Physicians Committee for Responsible Medicine, conducted via telephone interviews by ORC International May 2012, reports that a national survey of 1,015 adults revealed there are large gaps in America’s basic nutrition knowledge. The survey participants were adults (18 years and older) who proved to have very little knowledge of the basic nutritional content of dietary foods like milk, eggs and beef of which directly contributes to some of the nutrition-related diseases that kills millions of people every year. The obesity epidemic in West Virginia raises the risk of the population developing heart disease, cancer and diabetes that could be managed or prevented if they knew which foods were the healthiest for them (Committee, 2012).
A self-help booklet given to all SNAP benefit recipients after their nutrition class would include several web address links for them to recollect the information shared in the class. The first link is the United States Department of Agriculture where they provide the USDA Food Composition Database for people to research food products. The database includes the proximate principle analysis list such as proteins, fats, carbohydrates, mineral salts, and water found in the foods to show the effects of them on the body according to the nutritional value of each. It reports all ingredients and nutrients in brand named foods found in grocery stores across the country, a useful resource for those who are pursuing a healthy lifestyle (USDA, 2017). Another website in the booklet would be for the Food and Drug Administration’s Resources for Consumers for helping people learn to read nutrition fact labels on food products. There is a healthy diet guide for those with medical conditions like heart disease and high cholesterol to make the right choices for making a positive impact on their health. The self-testing tool helps consumers measure their understanding of the material on the web page and what eating nutritious food means to their health (USFDA, 2016). The last website directs consumers to “Self-Nutrition Data: know what you eat” which serves as a nutrition meal planning tool. It provides healthy recipes that has the ingredients, directions and the nutritional values per serving including calories, fat, carbohydrates, sugar, fiber and protein. For those who ever purchased sugary, frozen prepared food with their SNAP benefit card, this website shows them just how poor their decisions were as the percentage of the nutrients lost in processed food methods like freezing, drying, cooking and reheating are clearly displayed (Know What You Eat, 2014).
Although it is often cheaper to purchase processed foods, policy changes in the way SNAP benefits are spent will help limit the amount of these foods by recipients to 70% of the monthly benefits received and by the end of the five-year transitional period, the purchases unhealthy food options would be further reduced to 30% or less of the allotted benefits. As previously discussed, about 38% of adolescents reported eating less than one serving of fruits and one serving of vegetables daily. The need for farmer’s markets in all 55 West Virginia counties to have EBT card readers available for the purchase of fresh fruits and vegetables will be a part of the policy changes as well. The Farmers Market Coalition states that market retailers must complete an application and be licensed by the Food and Nutrition Service (FNS) to accept EBT SNAP benefits through a centralized point of sale. The state will require that within the next five years, all farmers must have obtained a license and have installed an EBT card reader for point of sale purchases (SNAP Advocacy, 2017).
Combating obesity involves more than monitoring food consumption as limiting fats and calories goes along with physical exercise and strengthening of the body and mind. Some children and adolescents are only active for the 90 minutes of physical education they participate in school. This is not nearly enough as the Center for Disease Control recommends children get at least 60 or more minutes of physical activity each day including three days of aerobic activity. With the limited amount of exercise time given in school about 90 minutes per week, policy changes in curriculum must be made so that physical education class returns the same results as a child exercising in a gym would receive, minus the weight lifting (Physical Activity, 2015) The change includes recommendations for three 45-minute physical education classes and two 30-minute yoga sessions per week from first grade to twelfth grade. Reports from the American Osteopathic Associate indicates that performing yoga focuses on the body’s tendency toward health and self-healing and its purpose, through breathing exercises, meditation and posture posing is to create strength, awareness and harmony with the body and mind. Besides lower blood pressure and reducing insomnia, yoga also helps to manage stress through the development of calming and coping skills (The Benefits of Yoga, 2017). Parents can set an example for their children by be active along with them by making a walk or a game a part of their daily routine before or after dinner. They can also take advantage of cost sharing opportunities with their employer for discount YMCA and gym memberships where they can attend exercise and yoga classes as a family. Participation in regular exercise routines can effectively prevent the onset on chronic disease caused by lack of physical activities seen in in almost 80% of adults over 65 years old.
In 2017, West Virginia ranked as having the highest adult population rate of obesity in the United States and The State of West Virginia Department of Health and Human Resources (DHHR) Bureau for Public Health reports that adults in this state are obese due to genetics, slowing metabolism, sedentary lifestyles, poor nutrition and environment which makes it easy to gain weight and hard to lose it. Chronic health condition is recognized as a growing problem in the state and organizations need work toward integrated health care to create a measurably healthier future environment for the population by 2020, but the effort is too low to realize that goal (Obesity and Related Chronic Diseases, 2016). The county health departments throughout the state must have a program better than the Chronic Disease Self-Management Program currently in place. Offering a two-hour meeting for 6 weeks to educate those with chronic illnesses will not have an overall lasting effect on lifestyle changes. The program should be staffed with experts in chronic disease management, a nutritionist for healthy diet management and a psychologist to help participants cope with lifestyle issues preventing success. The individual’s primary care physician should be responsible for the health plan describing which chronic condition should be addressed and the results tracked periodically. The new plan will increase the program length to a six-month period for learned participant practices to take hold and for any measurable disease management achievements to be noted by their physician. This addresses the challenging problems of physician’s taking on their patient’s mental health for which they have little time to offer the appropriate care needed along with low financial reimbursement rates from insurance companies.
The West Virginia Clinical and Translational Science Institute (WVCTSI) has recently expanded its Extension for Community Healthcare Outcomes (ECHO) project to combat chronic condition cases in rural areas. This chronic pain program connects a primary care physician (PCP) with treatment specialists at academic medical centers through video conferencing for patient case sharing and treatment option discussions of the best practices for chronic conditions like hepatitis C. Unicare Health Plan of West Virginia, Inc., the state’s largest provider of Medicaid managed health care benefits for more than 130,000 Medicaid beneficiaries throughout the communities is a big supporter of project ECHO (Moore, 2017). The federal and state grants that are allotted to the prevention of chronic disease and the promotion of health in West Virginia need to have a larger portion of funding being used for programs like ECHO, providing rural areas with access to health care. Improving access to healthcare in rural areas includes expanding the number of mobile clinics to include at least one unit serving no more than two to three counties in West Virginia. Services provided by these rural mobile units will include medical, dental, vision, pharmaceutical, behavioral health and addiction therapy along with health education information brochures.
A relatively new approach for providing access to care to people living in rural areas is through telemedicine, virtual patient visits where the doctor consults with a patient through a secure HIPAA-compliant videoconference. This treatment allows more accessibility to chronic disease patients who have transportation issues or have health problems limiting mobility, making attending regular appointments at the physician’s office problematic for them. Health insurance providers, including Medicaid, states that providers must still satisfy the federal requirements of efficiency, economy and quality of care to receive reimbursement requirements of efficiency, economy and quality of care to receive reimbursement for services for telemedicine diagnosis and treatment of patient conditions. Medicaid recognizes this as a cost-effective alternative to patient office visits to obtain a diagnosis and treatment plan, but there is still no commercial insurance coverage law for this service (Telemedicine, 2017). In March 2016, West Virginia Governor Earl Ray Tomblin signed a new bill into law (House Bill No. 4463) implementing telemedicine practice standards and remote prescribing rules, creating a new section in the West Virginia Code (§30-3-13a and 30-14-12d) applying to physicians who are appropriately licensed in the state. A patient-physician relationship previously established by an office visit can now be done through a review of health systems and health history performed via teleconference. Communities will set up state funded storefronts consisting of private rooms having teleconferencing equipment such as a webcam and computer with internet connection for patients who do not have this ability at home or who cannot travel to a physician’s office. Using telemedicine in conjunction with mobile units to educate and treat patients with chronic disease living in rural areas would help the state recognize their goals in reducing the number of obese people, increasing physical activity in the community and having fewer reported new cases of chronic illnesses (Lacktman, 2016).
IV. Discussion
Though this study makes an attempt at diagnosing and remedying the epidemic of obesity and mental illness created by social and economic factors in West Virginia, it is far from being a totally comprehensive analysis. Focusing on the combination of low income, low education, and elevated prevalence rates of mental health diagnoses and chronic obesity on overall health could overlook a portion of the population that does not suffer from all of these contributing factors but still suffers from being chronically overweight. While a large percentage of the West Virginian population suffers from at least one of these factors, this study represents only a piece of the larger overall picture. This study also assumes that those who suffer from these conditions will recognize the benefits of positive lifestyle changes and begin to take steps to address their conditions. It is also assumed that most West Virginians would be able to travel to the sites for the proposed alternatives. Those in the less rural areas of the state would most likely be able to do so. Those in the rural areas of West Virginia may not have access to the facilities proposed in these recommendations. For example, finding a fitness center that is both in a convenient location and able to support a program like the one proposed above could prove to be a hindrance to the proposed self-help program.
The policies proposed would all require acquisition of funding from either applying for grants or reallocation during the budgeting process in the state legislature. Expanding EBT benefits to include farmer’s markets would provide a boost to the local economy and result in more people having access to affordable, healthy nutrition options, however there could be hesitation from farmers because they would have to obtain a license to accept EBT transactions. Also, there could be an initial negative reaction from the program’s beneficiaries in response to limiting spending on more convenient processed foods. Restructuring the physical education curriculum would result in a more active and healthier population by forming life-long constructive perceptions of physical exercise and providing a foundation for dietary habits. The major hurdle in this proposition is the reconfiguration of the public education curriculum to allow for the required physical education time. If classes were shortened to allow for extended physical and health education classes, there would be less time allotted to other educational standards. However, if the school day was lengthened, the students’ families could react negatively due to time conflicts between school, work, and extracurricular activities. A longer school day could also increase the risk of fatigue and burnout in students. The proposed self-help program coordinated by county health departments could be a success in West Virginia. The programs would teach adults how to manage their weight, choose a healthy exercise program, and monitor their overall health. The program could experience growth that would result in decreased effectiveness because the demand could grow larger than the supply. However, a poor result could make the state legislature hesitant toward funding projects of this type because they would view it as wasted funding. The final proposed recommendation is mobile clinics and telemedicine. This could drastically improve access to health care in rural areas of West Virginia. The negative implications of this proposition are similar. Physicians would need to find time in their busy schedules to provide this care, and, as with the self-help program, the demand could greatly exceed the resources allotted to the program.
V. Conclusion
The public health epidemic of obesity shows a strong correlation to the mental health conditions reported within the State of West Virginia. As stated in the introduction, the percentage of adults being overweight and/or classified as obese accounts for over 69.7% of the State’s population. West Virginia is the also the 43rd in the nation in providing access to mental health care which attributes to the fact that only 46.9% of adults with mental illness diagnoses receiving regular treatment. These alarming statistics definitively suggest that these two conditions are related. In addition, studies on mental health treatments for depression have proven that diet and exercise can help improve a patient’s condition, giving more reason to believe that the lack of diet and exercise is causing both the obesity epidemic and the poor mental health conditions of the state.
The answer to this correlated epidemic is multi-faceted; involving economic, educational & social paradigms and requiring bold changes to all three. Economically, the state must take measures to restructure the SNAP program, requiring additional funding from a state and federal level. Increasing the requirements of SNAP participants to engage in nutritional educational classes along with structuring the availability of funds to certain classes of foods would promote successful training and execution of the nutritional guidelines. While this could be considered as an infringement upon the rights of the participants, the excess cost of the participants’ medical care should be considered an unnecessary benefit and reduced to offset any participants who do not wish to follow the guidelines.
Educational adjustments to elementary and middle school curriculum as well as increased physical education requirements at a high school level are required to further affect the obesity epidemic as well as the mental well-being of children and adolescents within the state. Studies have shown a positive correlation between positive mental well-being and increased physical activity in adolescents. The effect of an improved overall mental well-being on the obesity epidemic could only be favorable considering the correlation between these two diseases.
Access to consistent medical care is also imperative in the effort to remedy the prevalence of mental health diagnoses and obesity and the chronic conditions that result from them. Providing access to primary care through mobile clinics and telemedicine has the potential for reducing the impact of socioeconomic disparities and increasing the quality of life of all West Virginians. While this effort alone would be of great benefit to those in disadvantaged areas, the most impactful use would be if it were coupled with a widespread public health education campaign. The solution to the public health epidemic of obesity and mental health diagnoses in West Virginia can only come to fruition through the combined efforts of medicine, public health, and state legislature to address the health, economic, and social disparities of the state.
Bibliography
About Us : The Health Wagon. (2017). Retrieved from https://thehealthwagon.org/hwwp/about-us/
Amarasinghe, A., D’Souza, G., Brown, C., Oh, H., & Borisova, T. (2009, August 19). The Influence of Socioeconomic and Environmental Determinants on Health and Obesity: A West Virginia Case Study. Retrieved October 24, 2017, from http://www.mdpi.com/1660-4601/6/8/2271/htm
American Osteopathic Association. (2017).The Benefits of Yoga. Retrieved from American Osteopathic Association: http://www.osteopathic.org/osteopathic-health/about-your-health/health-conditions-library/general-health/Pages/yoga.aspx
Appalachian Regional Commission. (2017). Creating a Culture of Health in Appalachia- Disparities and Bright Spots- Key Findings: West Virginia. Retrieved October 26, 2017, from https://www.arc.gov/images/appregion/fact_sheets/HealthDisparities2017/WVHealt hDisparitiesKeyFindings8-17.pdf
Biddle, D. L., Justin, R., Charles, H., Guy, F., Mark, B., Michael, N., . . . Stuart. (2016). Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. doi:10.1542/peds.2016-1642
Cabell-Huntington Health Department (2017). Chronic Disease Self Management – Cabell-Huntington Health Department. Retrieved from https://www.cabellhealth.org/chronic-disease-self-management/
CDC. (2015) Physical Activity. Retrieved from Center for Disease Control and Prevention: https://www.cdc.gov/physicalactivity/basics/children/index.htm
CDC. (2016). West Virginia State Nutrition, Physical Activity, and Obesity Profile (Rep. No. CS266743-AU). Retrieved October 24, 2017, from https://www.cdc.gov/nccdphp/dnpao/state-local-programs/profiles/pdfs/west-virginia- state-profile.pdf
Centers for Disease Control (2016). Centers for Disease Control and Prevention Fiscal Year 2016 Grants Summary Profile Report for West Virginia. Retrieved from https://wwwn.cdc.gov/FundingProfilesApp/Report_Docs/PDFDocs/Rpt2016/West- Virginia-2016-CDC-Grants-Profile-Report.pdf
Charara, R., El Bcheraoui, C., Kravitz, H., Dhingra, S. S., & Mokdad, A. H. (2016). Mental distress and functional health in the United States. Preventative Medicine, 89, 292-300. Retrieved October 24, 2017, from http://www.elsevier.com/locate/ypmed
Committee, P. (2012, May 1). Survey Finds Americans Lack Basic Nutrition Information. Retrieved from Physicians Committee for Responsible Medicine: http://www.pcrm.org/health/reports/survey-americans-lack-basic-nutrition-info
CMS. (2017) Telemedicine. Retrieved from Medicaid: https://www.medicaid.gov/medicaid/benefits/telemed/index.html
Farmer’s Market Coalition. (2017) SNAP Advocacy. Retrieved from Farmers Market Coalition: https://farmersmarketcoalition.org/advocacy/snap/
Garasky, S., Mbwana, K., Romualdo, A., Tenaglio, A., & Roy, M. (2016). Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP). Retrieved from https://fns-prod.azureedge.net/sites/default/files/ops/SNAPFoodsTypicallyPurchased.pdf.
Healthcare Access in Rural Communities Introduction – Rural Health Information Hub. (2017). Retrieved from https://www.ruralhealthinfo.org/topics/healthcare-access#services
Knickman, J. R., & Kovner, A. R. (2015). Health Care Delivery in the United States. New York: Springer Publishing Company.
Lacktman, N. (2016, April 4). Health Care Law Today. Retrieved from foley & Lardner LLP: https://www.healthcarelawtoday.com/2016/04/04/west-virginias-new-telemedicine-practice-standards-remote-prescribing-laws/
Laurel House, Inc. (2017, March 07). Mental Health Resources in West Virginia. Retrieved October 25, 2017, from https://www.rtor.org/mental-health-west-virginia
Ma, J., Xiao, L., Rosas, L. G., Lewis, M. A., Goldhaber-Fiebert, J. D., Venditti, E. M., . . . Ward, E. (2017). Profiles of sociodemographic, behavioral, clinical and psychosocial characteristics among primary care patients with comorbid obesity and depression. Preventative Medicine Reports, 8, 42-50. Retrieved October 10, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5560114/.
Mastellos, N., Gunn, L. H., Felix, L. M., Car, J., & Majeed, A. (2017). Transtheoretical model stages of change for dietary and physical exercise modification in weight loss management for overweight and obese adults. doi:10.1002/14651858.CD008066.pub3
Moore, I. (2017, February 27). WVCTSI expands treatment of Chronic pain. Retrieved from West Virginia University School of Medicine: http://medicine.hsc.wvu.edu/News/Story?headline=wvctsi-expands-treatment-of-chronic-pain
Physical Activity | Healthy People 2020. (2017). Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/physical-activity/objectives
Self Nutrition Data. (2014, January 2). Know What You Eat. Retrieved from Self Nutrition Data: http://nutritiondata.self.com/mynd/myrecipes/welcome?returnto=/mynd/myrecipes
Shape of the Nation | State Profile. (2016). Retrieved from https://www.shapeamerica.org//advocacy/son/2016/upload/SON_-West_-Virginia_-2016.pdf
STOP Obesity Alliance. (2017). Retrieved from http://stopobesityalliance.org/
Substance Abuse and Mental Health Services Administration. Behavioral Health Barometer: West Virginia, 2015. HHS Publication No. SMA–16–Baro–2015–WV. Retrieved October, 25 2017, from https://www.samhsa.gov/data/sites/default/files/2015_West- Virginia_BHBarometer.pdf
United States Department of Agriculture (2016). State Data. Retrieved from https://data.ers.usda.gov/reports.aspx?ID=17854
United States Department of Agriculture (2017a). Profile of SNAP Households. Retrieved from https://fns-prod.azureedge.net/sites/default/files/ops/WestVirginia.pdf
United States Department of Agriculture (2017b). What Can SNAP Buy? | Food and Nutrition Service. Retrieved from https://www.fns.usda.gov/snap/eligible-food-items
USFDA. (2016, May 20). Using the Nutritional Facts Label: A How-To Guide for Older Adults. Retrieved from U.S. Food & Drug Administration: https://www.fda.gov/Food/ResourcesForYou/Consumers/ucm267499.htm
USDA. (2017, January 1). USDA Food Composition Databases. Retrieved from United States Department of Agriculture; Agricultural Research Service: https://ndb.nal.usda.gov/ndb/search/list
West Virginia Department of Health and Human Resources (2016). FARMERS ACTIVELY ACCEPTING SNAP AS OF JUNE 30, 2016. Retrieved from http://www.wvdhhr.org/ebt/Copy%20of%20WV%20FM%20and%20DF%20Sites%20as%20of%20June-2016%20With%20Formatting.pdf
West Virginia Supplemental Nutrition Assistance Program (SNAP) | Benefits.gov. (2017). Retrieved from: https://www.benefits.gov/benefits/benefit-details/1591
World Health Organization and the Calouste Gulbenkian Foundation (2014). Social Determinants of Mental Health. Retrieved from http://apps.who.int/iris/bitstream/10665/112828/1/9789241506809_eng.pdf
WV DHHR. (2016) Obesity and Related Chronic Diseases. Retrieved from WV DHHR; Division of Health Promotion and Chronic Disease: https://dhhr.wv.gov/hpcd/data_reports/Documents/Obesity%20Plan%20January%202016.pdf
WV DHHR. (2017). Addressing Obesity And Related Chronic Diseases: A Strategic Plan to Combat Obesity and Related Chronic Diseases in West Virginia (Rep.)
Yablonsky, T. (2017, March). West Virginia Behavioral Risk Factor Surveillance System Report 2014. Retrieved October 25, 2017, from http://www.wvdhhr.org/bph/hsc/pubs/brfss/2014/BRFSS2014.pdf
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Mental Health"
Mental Health relates to the emotional and psychological state that an individual is in. Mental Health can have a positive or negative impact on our behaviour, decision-making, and actions, as well as our general health and well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




