National Early Warning Score (NEWS) for Patients with an Exacerbation of Chronic Obstructive Pulmonary Disease (COPD)
Info: 17633 words (71 pages) Dissertation
Published: 11th Dec 2019
Tagged: Medical
A service evaluation to discover if the use of the National Early Warning Score (NEWS)for patients with an exacerbation of Chronic Obstructive Pulmonary Disease (COPD) during hospital admissionis causing unnecessary observation recording and inappropriate escalation of care.
CONTENTS I
Acknowledgements IV
Abbreviations V
Abstract 1
Chapter 1:Introduction 2
Chapter 2: Background 5
Early Warning Scores and the deteriorating patient
The National Early Warning Score
The Impact of COPD
The National Early Warning Score in relation to COPD patients
Chapter 3: Literature Review 9
Support for the use of NEWS in hospitalised patients
Concern about the use of NEWS in respiratory patients
Support for the use of NEWS specifically in COPD patients
Lack of evidence for the use of NEWS in COPD patients
Chapter 4: Aims and Objectives15
Chapter 5: Ethical Considerations16
Chapter 6: Methodology and Methods17
Methodology
Study Setting
Sample
Inclusion/Exclusion criteria
Data Collection
Chapter 7:Findings 22
Patient characteristics
Exclusions from the Study
How often did the NEWS result in increased frequency of observation recording when normal COPD parameters were recorded?
How often was care escalated to the medical team when NEWS was high although observations were within normal parameters for COPD patients?
How often was the protocol for the NEWS overruled because the patient has COPD?
Chapter 8: Discussion 26
How often did the NEWS result in increased frequency of observation recording when normal COPD parameters were recorded?
How often was care escalated to the medical team when NEWS was high although observations were within normal parameters for COPD patients?
Trigger Fatigue
Compliance
Limitations of the Study
Future considerations
Chapter 9: Conclusion 32
Appendices 34
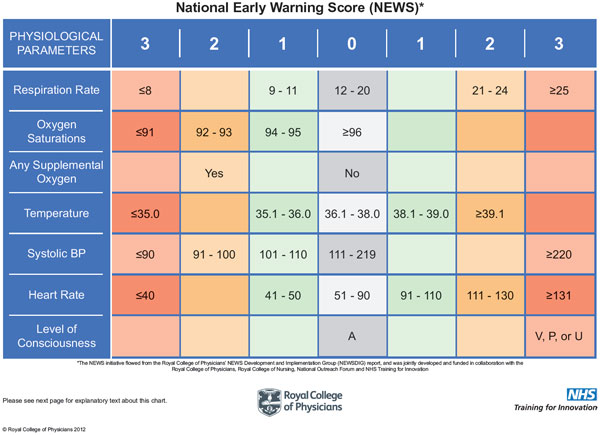
Appendix 1. National Early Warning Score (NEWS)
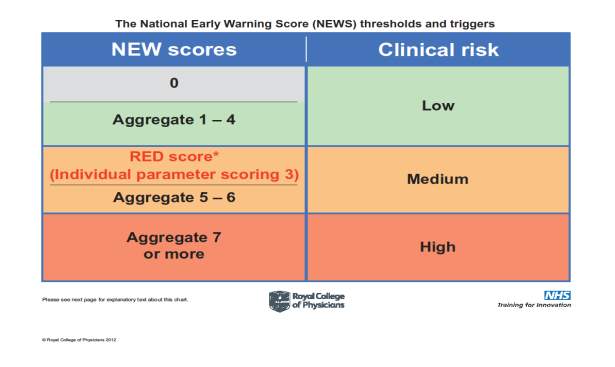
Appendix 2. National Early Warning Score (NEWS) Thresholds and triggers
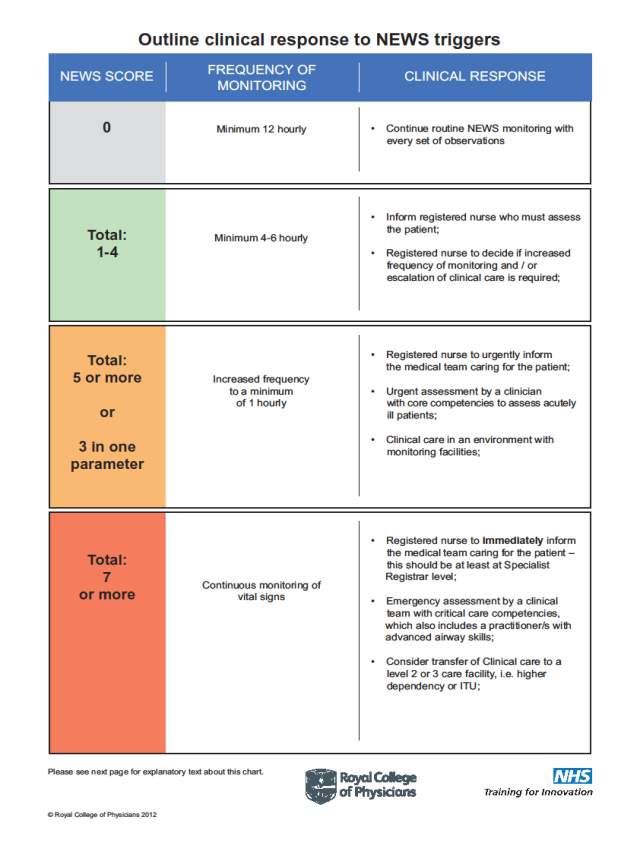
Appendix 3. Outline clinical response to NEWS triggers
Appendix 4. Modified Early Warning Score for COPD patients
Appendix 5. Literature Search Strategy
Appendix 6. Data Analysis
Appendix 7. Data Analysis continued.
Appendix 8. Journal Article
Appendix 9. Journal article link
References 43
Abbreviations
COPD Chronic Obstructive Pulmonary Disease
DOH Department of Health
ED Emergency Department
EWS Early Warning Score
LTOT Long Term Oxygen Therapy
mNEWS Modified National Early Warning Score
NEWS National Early Warning Score
NHS National Health Service
NICE National Institute for Clinical Excellence
RCP Royal College of Physicians
SIGN Scottish Intercollegiate Guidelines Network.
UK United Kingdom
WHO World Health Organisation
Abstract
Background
The NEWS is an assessmenttool developed to assist healthcare professionals to detect a deteriorating patient in order to allow them to intervene and prevent critical illness and preventable death. It incorporates guidelines on the care standards required for the deteriorating patient and informs the health care professional on how frequently to measure observations and when to escalate care to the medical team. The tool is designed to be used for all adult patients in secondary care regardless of diagnosis or co-morbidities with the exception of pregnant women.
It is the researcher’s intention to perform a service evaluation to determine if this is a tool and guideline which should be used for patients admitted to hospital with a COPD exacerbation. COPD patients are of particular interest to the researcher who is a Respiratory Specialist Nurse in an Acute NHS Trust.
Aim
The researcher aims to discover if the NEWS tool is fit for purpose for use with COPD patients. COPD patients have altered baseline parameters due to their diagnosis and it is the researcher’s suggestion that this prevents the NEWS from being suitable for this patient group. This alteration from the ‘norm’ leads to the over escalation of the patient and unnecessary observation recording.
Method
The researcher has chosen to perform a retrospective service evaluation with a quantitative design. 10% of the COPD admissions within a 12 month period have been analysed during this study. To each set of observations recorded for each patient a mNEWS has been applied which incorporates the altered baseline parameters for patients with COPD. The researcher has then compared the frequency of observation recording that the NEWS and the mNEWS have indicated. The frequency in which the NEWS has indicated escalation is necessary has also been recorded and then compared to the results that the mNEWS achieved. The medical and nursing notes have been interrogated to determine if escalation was indeed necessary, if the treatment/management plan was subsequently changed following escalation.
Findings
The results showed that the NEWS led to unnecessary observation recording 52% of the time. The NEWS also indicated patients should be escalated to the medical team 48% of the time, compared to the mNEWS which identified escalation was necessary just 8% of the time.
The researcher did discover that 48% of the timethe observations were not being recorded as frequently as the NEWS indicated and 96% of escalations were not being performed as indicated. Little documentation was found to explain lack of compliance with the guidance. Just 4 sets of medical/nursing notes had documented justification of the variance from the guidelines.
Conclusion
The researcher concludes that the NEWS tool and the guidance accompanying it are not suitable for use with patients admitted to hospital with exacerbation of COPD. If used as instructed the guidance leads to higher than needed frequency of observation recording and high levels of unnecessary escalation to the medical team. The fact that the guidance is not being used correctly a large proportion of the time supports the researcher’s argument that the tool is not fit for purpose.
Chapter 1. Introduction.
The NEWS was published by the Royal College of Physicians (RCP) in 2012. It was to replace the EWS previously in use in the NHS. Its sole purpose was to identify hospital patientswhose condition was deteriorating to enable health care professionals to intervene quickly and prevent patient death. It was initially adopted by 60% of NHS organisations with a further 20% expected to start using it in practice(Sprinks, 2013).
The NEWS is widely used in all adult inpatient areas except maternity. Evidence shows that the NEWS is safe and effective for reducing inpatient cardiac arrests and reducing preventable inpatient deaths (Smith, Prytherch, Meredith, Schmidt, & Featherstone, 2013).However, there is little research into the use of the NEWS for patients with specific medical conditions. It is used regardless of presenting complaint or previous medical history.
As Health Care professionals we are tasked to provide high quality, evidence based care for our patients. The Nursing and Midwifery Council Code of Conduct (2015)states that care should be based on research and best practice, but if there is no evidence for the use of the NEWS specifically in the patient group we are caring for we should not just assume that it will be ok.It is important that we discover what does happen when we use a tool that is not appropriate for the patients we are looking after.
This study is a retrospective service evaluation with the aim of determining if the NEWS is fit for purpose in the care of COPD patients admitted to hospital with an exacerbation.
Chapter 2. Background.
Early Warning Scores and the deteriorating patient.
It is widely accepted that physical deterioration of the patient occurs before the patient becomes critically ill (Cuthbertson & Smith, 2007). There is evidence to show that vital signs deteriorate in the hours leading up to a cardiac arrest and early detection and intervention can reduce the likelihood of deterioration, improving outcomes for the patient and reducing the likelihood of cardiac arrest(Smith et al., 2013).
The National Patient Safety Agency (NPSA, 2007) reviewed approximately 1500 inpatient deaths to see if there were any avoidable factors contributing to patient deaths. They suggested that 11% of all deaths are related to deterioration of the patient not being recognised and acted upon early enough.
EWS were first used in Liverpool, Australia and were designed to monitor a patient’s condition and trigger a review if the condition deteriorated (Cuthbertson& Smith 2007). The aim was to attempt to prevent critical illness or reduce the severity of the illness by early intervention. This initial EWS was only based on 1 parameter. Over the past few years healthcare professionals have recognised themerits of using these “track and trigger systems” and have tried to develop fail safe tools for themselves(Lee, Bishop, Hillman, & Daffurn,1995).
In 2007NICE published its guidance on managing acutely ill patients in hospital. The guidance was written following the NPSA (2007) report. The guidance recommended the use of anEWS in the management of the acutely ill patient although it stopped short of choosing which tool should be used. Mortality rates in hospitals have been shown to be reduced by the use of EWS (Smith,2013).
A systematicliterature review in 2008 by Smith, Prytherch, Schmidt and Featherstoneidentified 33 EWS tools being used in the UK alone. The review recognised that the physiological parameters measured in each tool were similar but felt that there was a lack of consistency with the scoring systems used. It was also found that the performance of the systems tested was poor when used to try to discriminate between survivors and non-survivors. The use of so many different EWS tools reduces their validity(Subbe, 2010).
The National Early Warning Score
In 2012 the RCP introduced the NEWS. Its aim was to standardise the assessment of the acutely ill patient across the UK. They wanted a standardised assessment tool to ensure consistency of assessment and equality of care.
The NEWS was designed to be used for all adults over the age of 16 with the exception of pregnant women. It monitors baseline parameters of Blood Pressure (BP), Heart Rate (HR), Oxygen saturations, Temperature, Respiratory rate and consciousness level. For each parameter measured the patient scores 0 for a measurement within normal baseline limits and 1-3 depending on how far away from the baseline the measurement is. The patient also scores 2 if they have supplemental oxygen in place. The scores for each parameter are then added together to give a NEWS(See Appendix 1).The higher the score the poorlier the patient(See Appendix 2).(Royal College of Nursing, 2012).
Once the NEWS is calculated the score is used to guide the healthcare professional on how frequently the patient should be reviewed and monitored and when to escalate care to the medical team. It also informs the healthcare professional on the seniority of the member of the medical team that the patient should be escalated to (See Appendix 3).
The NEWS is not advised to be used in the care of pregnant women and children. This is due to the fact that these patient groups react differently when acutely ill to adults and their baseline observations do not follow the same patterns as non-pregnant adults (RCP, 2012).Except for these two groups, the NEWS is promoted to be used for all other adult patients regardless of presenting complaint or past medical history. Much of the literature supports its use in general but there is little evidence evaluating the use of the tool in specific conditions.
The Impact of COPD
COPD is a condition that affects approximately 3 million people in the UK, of these only 900,000 will have a formal diagnosis. COPD accounts for 115,000 hospital admissions per year in England, 10% of which are in previously undiagnosed COPD patients. (NHS England 2014)
COPD is the second most common cause of emergency admission to hospital and the fifth biggest killer with more than 30,000 deaths a year (Department of Health, 2011).With such large numbers of patients involved it is imperative that we are using assessment tools that are fit for purpose and safe for this patient group.
The National Early Warning Score in relation to COPD patients
The pathophysiology of COPD causes patients suffering with the condition to have altered baseline parameters as a norm for them (Currie, 2007). Not all of the parameters measured for NEWS are affected by COPD but enough to potentially make the score an inaccurate reflection of how unwell the patient is.
Due to remodelling and mechanical failure of their lungs the patient with COPD will likely have constant progressive breathlessness and a higher than normal respiratory rate (Mitchell, 2015).They may also have chronic hypoxaemia which they can live with quite comfortably but their oxygen saturations will usually be lower than the norm. Patients with COPD may also have Long Term Oxygen Therapy (LTOT) at home(Holmes & Scullion, 2015). The NEWS for a COPD patient who is on LTOT at home will already be 2 before any observations have been recorded. These chronic changes result in 3 of the 6 parameters for NEWS being affected by the condition in the patient’s stable state. The health care professional then has the task to decide if the parameters are altered because the patient is ill, or if they are altered because the patient has COPD.
O’Driscoll (2012) suggests that NEWS is dangerous for COPD patients as the targets saturations are too high and health professionals may be encouraged to inappropriately administer oxygen therapy in order to achieve higher target saturations. High oxygen saturations in COPD patients are associated with increased risk of death from hypercapnia and respiratory acidosis. (Abdo & Heunks, 2012). This suggests that the use of NEWS for COPD patients may be dangerous and have the opposite effect to the desired aim.
Stable patients with COPD may be scoring high NEWS and triggering false reviews. This may lead to trigger fatigue whereby a genuine deterioration in condition goes unnoticed as it is assumed that the trigger is a false alarm again (Cvach, 2012). Trigger fatigue puts the patient in danger of missed deterioration and missed opportunity for intervention, which could prove to be fatal.
The RCP acknowledge that healthcare professionals should take into account long term conditions which alter baseline parameters when interpreting NEWS but they do still recommend the use of the NEWS for this patient group (Rees & Calverley, 2002).
The researcher is a Respiratory Specialist Nurse working in an Acute NHS Hospital Trust. The researcher has 19 years’ experience in the field of Respiratory Medicine. As part of the researchers nursing role Early Supported Discharge is offered to patients admitted with COPD exacerbations who fulfil certain criteria. The researcher has found on many occasions that patients who fulfil the criteria for Early Supported Discharge have high NEWS score and the ward staff have escalated care to the Critical Care Outreach Nurse for review, delaying the Early Supported Discharge until this review has taken place.
Patients on the Respiratory ward frequently complain to the researcher of being woken during the night for observation recording and the NEWS is consistently high for many patients. For these reasons the researcher has decided to focus on the use of the NEWS for this particular patient group.
Chapter 3. Literature Review
Literature reviews are essential before commencing any research project. They can inform the researcher if the research is necessary or if it has already been done before. It can help the researcher design the research project by seeing what has been done before and how it was carried out(Clifford, 1997). The researcher can critique existing research and identify strengths and weaknesses in the design and adapt their own design accordingly (Boote & Beile, 2005).Bowling and Ebrahim (2005) suggest that a good literature review can ensure that research is both balanced and comprehensive ensuring that there is not a plethora of research on the same issue with the same results being found.
A literature review was carried out using the University Database Summon. The term NEWS generated a return of 30,515 articles. The researcher did a Boolean search using NEWS AND COPD which reduced the number to 3,433. Limiting the search to journal articles reduced the results to 530 articles. The researcher also looked at NEWS AND/OR EWS AND COPD which still returned 530 articles. Limiting the search to articles in the last 10 years returned 430 results and limiting to scholarly and peer reviewed articles reduced the number to 422. By limiting the search terms to title and abstract this reduced the search results to just 10 articles. The researcher read the abstract of these articles and decided that 7 were relevant to the project and warranted further discussionSee Appendix 5.
The researcher went on to search CINAHL and MEDLINE databases at the Acute Hospital TrustLibrary using the same search methods.Only 1 new relevant article was found See Appendix 5.Some key themes emerged from the literature review which we will discuss.
All research is graded or given a level which indicates its quality. There are some discrepancies over the grading systems used but all agree that the highest level of recommendation should inform clinical decisions and help to make clinical guidelines. High quality randomised control trials achieve the highest level of recommendation but these are not always achievable(Haber, Whitehead, Schneider & LoBiondo- Wood, 2012).
Support for the use of NEWS in hospitalised patients.
The literature review showed that there was a plethora of evidence supporting the use of the NEWS tool in hospital patients in general but when COPD was added to the search the results reduced considerably.
A systematic review on the use of EWS was carried out by the National Early Warning Score Development and Implementation Group (Jones,2012) before they developed the NEWS tool (RCP 2012). Melnyk and Fineout-Overholt (2011) suggest that systematic reviews or meta-analysis are a good starting point to developing such a tool as they produce strong levels of evidence to support evidence based practice.
NICE performed a systematic literature review before recommending the use of EWS in 2007. In the hierarchy of evidence a literature review is a level III recommendation (Burns, Rohrich & Chung, 2011). Subsequently NHS England supported the use of the NEWS following its own review. It reviewed the evidence for NEWS in conjunction with the NICE and SIGN guidelines.
Concern about the use of NEWS in respiratory patients.
Eccles, Subbe, Hancock & Thomson (2014) were the first researchers to look at the NEWS in relation to COPD patients. The CREWS study (Chronic Respiratory Early Warning Score) was a small study in which one of the NEWS parameters was modified for COPD patients and retrospectively appliedto the NEWS score of patients admitted to hospital with an exacerbation of COPD. The results showed that using CREWS reduced false triggers and unnecessary recording of observations and was therefore more efficient and effective. It also proved that the modification was safe by maintaining the sensitivity of the tool. However, the generalisability of this study ispoor due to it being a very small study with only two centres in Wales being included in the sample. The demographics of the population were very similar. It cannot be assumed that the same results would have been found if it had been a large multi-centred study (Robertson, 1994).
The study design itself was very simple and therefore reproducibility would be achievable.This would make further research easier as the study design can be repeated.
Eccles et al. (2014) recommended the use of a modified NEWS for COPD patients. This was a level 3 recommendation as it came from a retrospective observational study with control (Burns, Rohrich & Chung 2011). This is not a high level of recommendation and would not be strong enough evidence to change practice on its own.
Lobo, Lynch, & Casserly, (2015) suggested that NEWS is not as useful in determining the deteriorating patient with chronic hypoxaemia. The study was not limited to COPD as Eccles et al.’s (2014) study was but included other causes of chronic hypoxaemia also. The study was a cross sectional audit which looked retrospectively at the medical records of patients with chronic hypoxaemia. It specifically looked at patients with a NEWS of 7 or more.
Lobo et al. (2015) wanted to see if the higher NEWS resulted in any change in medical management or discharge outcomes. A modified NEWS score was applied taking into account altered baseline parameters for patients with chronic hypoxaemia and determined if it changed the trigger thresholds for this group of patients. The findings were that the high NEWS did not change the medical management in 64.6% of these cases and 94.1% of these patients were discharged home. By adjusting the NEWS to take into account the altered baseline parameters of chronic hypoxaemic patients the number of reviews would have been reduced by 70.3%. The study concluded that NEWSs are poor discriminators of deterioration in chronic respiratory patients.
However the study was on a small scale and in one centre, a Model 2 hospital setting which reduces its generalisability (Robertson, 1994). A Model 2 hospital is one in which there are no emergency departments or critical care facilities such as intensive care or high dependency. The study alone would not be strong enough evidence to change practice and further evidence would be needed to support the findings.
It is interesting to note that the Irish NEWS applies a score of 3 to supplemental oxygen, whereas the UK NEWS applies a score of 2. The RCP suggests that the NEWS should be interpreted with caution in the case of patients with chronic hypoxaemia, some of whom may have supplemental oxygen at home and this is their baseline (RCP, 2012).
This study supports that suggestion that Eccles at al. (2014) made in that the NEWS needs modifying for specific patient groups. The two studies together suggest that the NEWS is inefficient and ineffective for COPD patients and was a poor discriminator of deterioration in COPD patients.
Kane, Decalmer, Murphy, Turkington & O’Driscoll (2012) suggest in their article that the use of the NEWS for COPD patients may encourage inappropriate and potentially fatal use of oxygen as Health Care Professionals attempt to achieve target saturations by giving supplemental oxygen increasing the risk of hypercapnic respiratory failure. As Lobo et al. (2015) suggest that the NEWS is not a good indicator of the deteriorating hypoxaemic patient; Kane et al. (2012) suggest that the NEWS can actually put the patient in danger as Healthcare Professionals strive to achieve target saturations. Kane et al. (2015) also promote the idea of using a modified NEWS to assess COPD patients; however their article is based on expert opinion and experience rather than any thorough research methods such as Lobo et al.’s (2015) study. This makes it a level 4 recommendation. Research would be needed to back up this opinion before practice should be changed.
Hodgson, Dimitrov, Congleton, Venn, Forni, &Rodrick (2017) acknowledged that NEWS predicted mortality rate in general medical admissions but wanted to see if the same was true for COPD admissions. This study was a retrospective analysis of patient observations in an acute Trust,comparing NEWS scores in general medical admission of patients over the age of 50 with NEWS scores of COPD admissions in the same age range in a 12 month period. The study concluded that in the general medical patient group there was a correlation between an increased NEWS and patient mortality, however in the COPD group patients with lower NEWS of 2-4 had a higher mortality rate than those with a higher NEWS of 5-6 in the general medical group. COPD patients had a mortality rate equal to that of the general medical patients but higher NEWS.
Hodgson et al. (2017) concluded that NEWS for COPD should take into account lower oxygen saturation targets to reduce the risk of over-estimating mortality risk and causing unnecessary concern for this patient group. Target saturations for COPD patients were modified and applied to the NEWSand then compared with the traditional NEWS. The study found that in COPD patients NEWS was not as sensitive to patient deterioration as it was for general patients but the modified NEWS was more sensitive and still as valuable in predicting mortality (Hodgson et al. 2017).This was a reasonable sized study with 13,291 general medical patients and 1119 COPD patients, approximately 7% of the overall admissions. It took place in one acute medical Trust which reduces its external validity (Subbe, 2010). A multi-centred study would have made the research more valid and the evidence base would have been stronger.
All of the above studies support the argument that the NEWS should be modified for COPD patients in order to make the tool more efficient, effective and safer for the patient. A meta-analysis or systematic review of the studies would help to inform practice for the future. (Doolen, 2017).
Support for the use of NEWS specifically in COPD patients.
Murphy, Mydin, Fatah & Antunes (2010) suggest that the NEWS can be used as a tool to help predict mortality in COPD patients. The study involved case reviews of patients who had died in hospital from exacerbation of COPD and compared the medical records on the admission when they died to the penultimate admission. The results showed that the Respiratory rate did not change between the admissions but the EWS was higher on final admission than penultimate admission. The EWS did not respond to treatment on final admission and this was attributed to systemic physiological disturbances rather than respiratory specific variables which did not change. The study concluded that EWS is a predictor of mortality in COPD.
This study may support the argument that NEWS can be modified for COPD patients without compromising safety as even in the admission leading to patient death the respiratory variables did not change.However the external validity of this study was compromised due to it being conducted in one hospital and the sample size was small. As a stand-alone piece of work it would not be strong enough evidence to support a change in practice.
Bilben, Grandal & Sovik (2016) agree that using NEWS in patients admitted to ED with an exacerbation of COPD can be used as a marker of disease severity to predict 90 day mortality. A small prospective observational study was performed in a Scandinavian emergency department. The study included all patients admitted to the ED within a 4 month time period with respiratory distress not just COPD exacerbations.The external validity of this study is compromised due to the sample size and demographics of the study subjects and therefore further large scale multi-centred studies would improve the validity of the research (Jolley, 2013).
Murphy et al. (2010) and Bilben at al. (2016) agree that the NEWS is a good predictor of mortality but the tool was designed to detect the deteriorating patient not predict mortality. Murphy et al.’s study suggests that the NEWS could be modified for COPD patients without reducing its ability to predict mortality as the respiratory variables did not change between penultimate admission and final admission. This would support the arguments from Eccles et al. (2014), Lobo et al. (2015), Kane et al. (2012) and Hodgson et al. (2017) that the NEWS should be modified for COPD patient. The modification of the NEWS tool could enhance patient safety; make the tool more time efficient and effective whilst maintaining sensitivity and the ability to predict mortality. A large scale multi-centred study looking at all the outcomes, meta-analysis or systematic review of the literature would help to confirm the findings of all the studies and assist in the decision making process in order to develop a modified NEWS.
Lack of evidence for the use of NEWS in COPD patients.
It is essential that when we are developing guidelines that we use the highest levels of recommendations that are available in order to make the best decisions (Parahoo, 2006). There was very little research performed around the use of the NEWS specifically in the care of patients experiencing an exacerbation of COPD. What evidence there was didn’t really confirm if NEWS was doing what it was intended which is to identify the deteriorating patient. Some of the research suggests that NEWS identifies a COPD patient as deteriorating when in fact they are stable. Other research suggested that NEWS may be a good predictor of mortality this is not what NEWS was intended to be used for.A meta-analysis of all the literature reviewed together would produce a higher level of evidence in which to inform practice and produce guidelines (Gerrish & Lacey, 2006).
The literature review supports the researcher’s view that this project is worthwhile and necessary. At the moment there is insufficient evidence to show whether the NEWS should or should not be used to assess COPD patients without modification. None of the studies undertaken looked at all the NEWSs for the whole period of admission for the patients involved in the study. They all looked at certain points during admission or took an average NEWS for the admission period. Many of the studies were concerned with mortality but this study solely focuses on unnecessary observation recording and inappropriate escalation of care. None of the studies have discussed inappropriate escalation of care although the concept of trigger fatigue has been mentioned (Eccles et al. 2014).
Chapter 4. Aims and Objectives
The aim of this research is to evaluate the use of the NEWS in patients admitted to hospital with an exacerbation of COPD to determine if its use leads to unnecessary recording of observations and inappropriate escalation of care. As a secondary objective it will discuss if the use of the NEWS in this patient group does lead to trigger fatigue.
Objectives
- How often did the NEWS result in increased frequency of observation recording when normal COPD parameters were recorded?
- How often was care escalated to the medical team when NEWS was high although observations were within normal parameters for COPD patients?
- How often was the protocol for the NEWS overruled because the patient has COPD?
- Are there any recommendations which could make the use of the NEWS safer for this patient group?
Chapter 5.Ethical Considerations
Research should demonstrate new evidence or inform good practice. It should be used to benefit the individual and the wider population without causing any distress or harm to anyone involved in the process (Polit & Beck, 2014). As a retrospective service evaluation this piece of research does not directly affect any individual but may inform best practice for the future. There is no intervention to patient care therefore the research can cause no harm. Gallagher & Boyd (1991) argue that research should be morally right and the researcher should ensure that it is carried out by the right person in the correct manner.
The researcher did not need to gain formal ethical approval from the Research Ethics Committee for the study as there was no direct contact with individuals and there was no intervention to patient care; however the researcher did obtain permission from the Acute Trust’s Research and Development Department to gain access to patients medical records included in the review (Fry & Johnstone 2008). The researcher discussed the project with the Acute Trust’s Caldecott Guardian to ensure that the Caldecott guidelines were followed and that patient information was accessed and used appropriately and anonymised to protect patient confidentiality (Caldecott, 2013).The research has been anonymised and no patient identifiable data will be included.
The researcher did obtain ethical approval from the University ethics committee demonstrating that the research was justifiable in that it will inform best practice and benefit the healthcare profession rather than being performed for personal gain.The research was carried out in partial fulfilment for a Master’s degree in Health Studies (Long Term Conditions). The researcher has not gained any financial reward for completing the project. The researcher does not have any association with the Royal College of Physicians responsible for the publishing of the NEWS, therefore there is no conflict of interest. The researcher has completed the piece of work in their own time.
Chapter 6. Methodology and Methods
Methodology
A service evaluation was chosen for this project. Service evaluations are useful in assessing if a service can achieve its intended aims (Clifford, 1997). It can help service users judge the success or failure of the service as it is and can assist decision making (Roe & Webb, 1998). A service evaluation may shape the way a service is run and can help services develop into more effective or efficient services. In some cases service evaluations may prove that the service cannot achieve its aim and the service must be adapted or even discontinued (National Research Ethics Service [NRES], 2013).The results of service evaluations are mostly used to generate information that can be used to inform local decision-making (Twycross & Shorten 2014).
The researcher chose to perform a retrospective service evaluation using a quantitative research design to answer the objectives set, using the numerical data of patient observations and NEWSs in a structured and systematic way. The data was analysed scientifically and objectively ensuring that results were both reliable and valid (Maltby, Williams, McGarry& Day, 2010).A qualitative research design would have been appropriate for this study if the researcher was investigating how health care professionals felt about using the NEWS for COPD patients and wanted their opinions and experiences on the subject. Qualitative research can provide depth and richness of information that quantitative data lacks (Holloway & Wheeler, 2010). The focus of this study was more aligned to a quantitative approach. Gerrish and Lacey (2006) argue that research methods should be consistent and reproducible and good quality service evaluations produce results which are valid and reliable.
A Population Intervention Comparison Outcome Time (PICOT) framework was used to develop the research question. This format helps to ensure that the information needed to answer the research question is identified so that the research is both effective and efficient (Melnyk & Fineout-Overholt, 2011).
Study Setting
The research was carried out in an Acute Hospital Trust with 3 hospital sites although the third hospital site does not have medical inpatient beds. The Acute Trust was accessible to the researcher who is an employee of the Trust and has access to the systems needed to obtain the data required for the study and is familiar with using these systems. The Acute Trust has approximately 500 admissions due to COPD exacerbation each year so has the requisite patient group. This is an example of purposive convenience sample as it contains the relevant patient group and is easily accessible to the researcher (Brink & Wood, 2001).Using a convenience sample reduced generalisability of the study which was further compromised by the fact that all the patients were admitted to the same Acute Hospital Trust and were likely to have similar demographics (Robertson, 1994).
The internal validity of the study was guaranteed as the researcher completed the project alone ensuring the same data collection process was followed each time using the same assessment tools. This meant that no other variables could influence the results (Melnyk & Fineout-Overholt, 2011). The external validity however was reduced due to the fact that the research was confined to one healthcare setting and involved a relatively small sample size (Jolley, 2013). By using their own Acute Trust the researcher should be aware of their own views and opinions and previous experience. The process can be biased at any stage and this should be taken into account (Aveyard & Sharp, 2009). The risk of bias was minimised by ensuring transparency in the research process (Malicki & Marusic, 2014).
Sample
The researcher made a request to the Information Management department at the Acute Hospital Trust for a list of hospital numbers for patients admitted between April 2015 and March 2016 whose admission has been given the following code:
J44.1 COPD with acute exacerbation unspecified.
The code required for the search was identified by the coding department at the researcher’s request. From the search results 10% of the hospital numbers identified were randomly selected and the medical and nursing records interrogated further for these patients. By looking at the hospital numbers in isolation to select the patients the researcher did not know the gender, age or any other demographics of the sample group. This reduced bias in the sample selection. Reducing bias increases the impact of the research (Smith & Noble, 2014).
Randomisation of the sample will ensure that the research is more robust by again eliminating bias (Jolley, 2013). The randomisation of these hospital numbers was achieved by cutting each number on the list out and pulling them out of a box. There are many ways to randomly select subjects to be included in a study. Some researchers use computer programmes to randomly select the sample but the researcher didn’t have access to these programmes. Each subject was given equal chance of being chosen from the box, increasing the generalisability of the study (Holzemer, 2010).
The researcher chose to review just 10% of the sample given in the list. The Trust admitted 487patients in this time period and the average length of stay for these patients was 6days. To look at all the admissions would have equated to too a large number of recorded observations to accurately review and this was not achievable in the time limit given.
Inclusion/Exclusion Criteria
All patients admitted to the Acute Hospital Trust between April 2015 and March 2016 with the following read code:J44.1 COPD with acute exacerbation unspecified,were eligible for inclusion in the study. Observations were analysed for the admission period only, meaning that A&E observations were not included. This was due to the researcher using the VitalPac system to interrogate the patient records. A&E in this Acute NHS Trust currently use paper observation charts. The VitalPac records are then uploaded into WinDip once the patient is discharged along with all the medical and nursing records for the patient.
If a patient had had more than one admission during this time period and was chosen more than once, each admission was included in the research and each episode of care was reviewed separately. The admission code was cross-referenced with the patient discharge letter to ensure that the coding was correct. Any patient whose diagnosis did not match the coding given was excluded from the study.
Consent was not obtained from the patients included in the study as only patient data was used and there were no changes to patient care meaning that consent was not necessary (Fry & Johnstone, 2008).
Data Collection.
A password protected excel database was used to input the data required for analysis. The data was captured using the Acute NHS Trust Information Technology systems, WinDip and VitalPac. Password protecting the data ensured that the researcher complied with the Data Protection Act (1998) and adhered to the Caldecott principles as promised to the Caldecott guardian at the Trust when ethical approval was granted (Caldecott, 2013).
The researcher recorded the NEWS at each observation measurement for each patient on the excel database and documented the frequency of observation recording indicated by the NEWS. The researcher also recorded if the frequency of observation recording indicated by the NEWS was adhered to.
If the patient care was escalated because of the NEWS this was also noted. When care was identified as needing to be escalated the medical and nursing recordswere checked to see if the escalation took place, if it was escalated to the correct level of seniority on the medical team and if the treatment/management of the patient was changed after review of the patient following escalation of care.
The NEWS was retrospectively adjusted to take into account the modified targets for COPD patientsandthe frequency of observations indicated by the mNEWSwas calculated and recorded to identify if the frequency differed from that indicated by the NEWS. The researcher also calculated if the mNEWS would have indicated escalation was necessary. (See Appendix 4).
Data Analysis
The researcherused the mNEWS alongside their clinical judgement and experience to determine if observations were recorded too frequently and if the mNEWS would have resulted in any trigger scores being missed by recording the observation less frequently.
When patient care was escalated the researcher documented if this was appropriate by looking at the medical and nursing notes and reviewing if the treatment/management of the patient had been changed or frequency of observations had been changed following review. An assumption was made that the patient medical and nursing notes were accurate and any escalation performed was recorded. The researcher accepts that there may have been occasions when care was escalated but not recorded in the medical/nursing notes.
The researcher scrutinised the medical/nursing notes to determine if any variation to the NEWS protocol was documented and explained or rationalised. For example if the nurse documented that care was not escalated due to the patient having altered target oxygen saturations.
At the end of the data collection period the researcher collated all the information to answer the objectives set out.
Chapter 7. Findings
Patient characteristics
48 sets of medical and nursing notes for patients admitted to hospital with COPD exacerbation between April 2015 and March 2016 were interrogated during the study.This equated to 10% of all the admissions coded as J44.1 COPD with acute exacerbation unspecified.
The patient location was recorded each time. 27 of the patients chosen for the study were admitted to hospital Site A and 21 were admitted to Hospital Site B. No patients were admitted to hospital site C as there are no medical inpatient beds.
Out of 48 patients 23 were cared for on a Respiratory Ward, less than 50% of the admissions analysed. 23 were admitted to other medical wards but 2 patients were admitted to surgical wards. See table 1.
Total days in hospital for this patient group were 186 days with an average length of stay of 4 days. A full breakdown of the data collected can be seen in Appendix6.
6 of the patients included in the study had LTOT at home prior to admission. Each time observations were recorded they scored 2 points for having oxygen even though it was “normal” for them.
All of the patients included in the study recovered from their exacerbations and were safely discharged home.
Table 1. Patient Characteristics
| Location of patients | ||
| Hospital Site A – 27 patients | Respiratory Ward No 1 | 7 |
| Respiratory Ward No. 2 | 12 | |
| Medical Admission Unit | 5 | |
| Short Stay Medical Ward | 1 | |
| Medical extra Capacity Ward | 1 | |
| Stroke/neurology Ward | 1 | |
| Hospital Site B – 21 patients | Respiratory Ward | 4 |
| Medical Admission Unit | 7 | |
| Short Stay Medical Ward | 6 | |
| Elderly Medical Ward | 2 | |
| Female Surgical Ward | 1 | |
| Male Surgical Ward | 1 | |
| Number of patients with LTOT at home prior to admission | 6 | |
Exclusions from the Study.
22 sets of medical notes were excluded from the study due to the patients having a different diagnosis on the discharge letter from hospital. See Table 2.
Table 2. Patients excluded from study
| Number of patients excluded from study | Reason for exclusion |
| 8 | Patients discharged from A&E. |
| 2 | No case notes available for study |
| 8 | Patients diagnosed with pneumonia as presenting complaint, COPD was co-morbidity |
| 2 | Patients diagnosed with asthma as presenting complaint |
| 1 | Patient diagnosed with Congestive Cardiac Failure, COPD was co-morbidity |
| 1 | Patient diagnosed with Bronchiectasis, COPD was co-morbidity |
| Total excluded : 22 | |
How often did the NEWS result in increased frequency of observation recording when normal COPD parameters were recorded?
A total of 789 sets of observations were analysed and the mNEWS applied to each one.The average NEWS for all the patients was 3.6 whereas the average mNEWS for all the patients was 1.9 (See Appendix 7.)
The mNEWS indicated that on 135 occasions the observation recording was unnecessary and the frequency of recording was too often, this equated to 17% of the observations recorded.
The researcher noted that observations were only recorded on time as indicated by the NEWS 52% of the time. However if observations were all taken on time as indicated by the NEWS the number of unnecessary observations would have increased to 409, 52% of the observations. See table 3.
Each time the mNEWS changed the frequency of the observation recording the researcher checked the subsequent NEWS to see if the mNEWS would have missed deterioration in the patient. On no occasion would the mNEWS have missed deterioration in the patient.
Table 3. Breakdown of results from data collection
| Data collected | |
| Total number of days in hospital for all 48 patients | 186 |
| Number of observations analysed for all 48 patients | 789 |
| Number of unnecessary observations indicated by NEWS according to mNEWS | 409 (52% of observations recorded) |
| Number of unnecessary observations recorded according to mNEWS | 135 (17% of observations recorded) |
| % of observations recorded on time | 52% |
How often was care escalatedto the medical team when NEWS was high although observations were within normal parameters for COPD patients?
The study showed that on 381 occasions the NEWS indicated that care should be escalated to the medical team. This is an astounding 48% of the time. 338 occasions were due to NEWS being above 5 and 43 due to NEWS being 3-4 with 3 in one domain. The mNEWS reduced the total number of escalations indicated by 82% to just 70. See table 4.
How often was the protocol for the NEWS overruled because the patient has COPD?
It was noted during the study that patient care was actually escalated on just 17 occasions, 4% of the escalations indicated by NEWS and 25% of the escalations indicated by mNEWS.However on 364 occasions care was not escalated as indicated by the NEWS. See table 4.
No unnecessary escalations were performed. Each time an escalation was performed the management/treatment plan for the patient was altered following the escalation therefore the researcher recorded the escalation as appropriate.
The researcher only found 4 sets of medical/nursing records out of the 48 analysed in which the variance from the NEWS protocol was explicitly explained/ justified.
Table 4. Breakdown of results from data collection continued.
| Number of escalations indicated by NEWS 5+ | 338 |
| Number of escalations indicated by mNEWS 5+ | 67 |
| Number of escalations indicated by NEWS 3-4 (3 in one domain) | 43 |
| Number of escalations indicated by mNEWS 3-4 (3 in one domain) | 3 |
| Total Number of escalations indicated by NEWS | 381 (48%) |
| Total Number of escalations indicated by mNEWS | 70 (8% of observations, 18% of escalations indicated by NEWS) |
| Number of escalations performed | 17 (4% of escalations indicated by NEWS, (25% of escalations indicated by mNEWS) |
| Number of unnecessary escalations performed | 0 |
| Number of escalations indicated by NEWS but not carried out | 364 |
| Number of triggers missed by mNEWS | 0 |
The NEWS and mNEWS were recorded at discharge for each patient. On 7 occasions patients were discharged home despite having a NEWS of 5+. The mNEWS was within the escalation range on only one occasion. See table 5.
The discharge NEWS’s were noticeably higher than the discharge mNEWS’s. Only 4 patients had a discharge NEWS of 0, indicating all observations were within normal parameters, whereas 17 patients had a mNEWS of 0.
Table 5. NEWS v mNEWS on discharge from hospital
| Score | No. of patients with Discharge NEWS | No. of patients with Discharge mNEWS |
| 0 | 4 | 17 |
| 1 | 9 | 16 |
| 2 | 8 | 5 |
| 3 | 11 | 6 |
| 4 | 9 | 3 |
| 5 | 4 | 0 |
| 6 | 2 | 0 |
| 7 | 0 | 1 |
| 8 | 1 | 0 |
Chapter 8. Discussion
Thisservice evaluation representshow the NEWS is used for patients with an exacerbation of COPD admitted to the Acute NHS Hospital Trust.
The NEWS did result in increased frequency of observation recording when normal COPD parameters were recorded.
The researcher proposed that the NEWS in patients with COPD exacerbation resulted in unnecessary observations being recorded and aimed to prove this with the service evaluation. What the evidence actually showed was that only 52% of the observations were being recorded on time as suggested by the NEWS. This meant that 48% of the time observations were being missed in this patient group. It was apparent from the results that the observations were not being recorded as frequently as the NEWS indicated that they should be, but there was little documentation as to why this was happening. On only 4 occasions was the variance from the guidance justified. This is not a finding which has been discovered within the previous studies discussed.
It could be assumed that the nursing staff recognised that the observations didn’t need recording as frequently because the patient observations were within the target range for COPD patients. However it could just as easily be assumed that the observations were missed due to workload pressures or the nursing staff didn’t understand the guidance or just blatant disregard for the guidelines. Without documentation supporting the decision not to record the observations as frequently as indicated we should not assume anything.
In practical terms a COPD patient could be admitted to hospital with observations within target range for their condition but because of the NEWS they could be having observations recorded hourly. This may be a little annoying through the day but would be very disturbing at night. The nursing staff can override the frequency of observation recording but should document why the variance is occurring so that other healthcare professionals understand the rationale behind the decision to override the guidance. Guidelines are used to inform best practice in an effort to maintain patient safety and deliver high quality patient care. If we are to deviate from the guidelines we must ensure that patient care and safety is not compromised and that we are working within the patients best interests (Tingle, 2002).
It is essential that the nursing staff document carefully any variance from protocols or guidance. This is to protect their registration and protect them from litigation. If a nurse does not work within the guidance and does not document the reason that their practice is outside of the guidance then they could be considered to be negligent. Any variance from guidelines should be recorded and justified (Tingle, 2002).
The researcher did show that the mNEWS would have resulted in a reduction in the frequency of observations recorded, 48% of the time. This would have led to the staff needing to record observations less frequently without the need to justify the variation to the guidance. This in itself is more time efficient and protects the staff from criticism in relation to disregarding guidelines and protocols. This finding supports the evidence from the CREWS study in 2014 (Eccles et al.). On no occasion would the reduction in frequency of the observation recording indicated by the mNEWShave led to a missed deterioration of the patient. This confirms that the mNEWSis both safe and time efficient. Eccles, Subbe, Hancock and Thompson (2013) also considered the modification of the NEWS to be safe for COPD patients. The mNEWS tool would need to be validated in order to be adopted officially and further validation studies would be required.
Escalation was indicatedto the medical team when NEWS was high despite observations being within normal parameters for COPD patients.
The NEWS recommends escalation of the patient to the medical team if the score is 3-4, with 3 in one domain or 5+. The researcher demonstrated that the NEWS indicated escalation was necessary 381 times out of the 789 sets of observations recorded, which equates to 48% of the time. This is a significant number of escalations and would take up a large amount of time for the medical team. The mNEWS reduced the number of escalations needed by 82% to 70, 18% of all the observations recorded.The escalations were actually carried out just 17 times, 4% of the time indicated. The researcher checked the medical and nursing notes to determine if the escalations performed were necessary. In every case where the escalation was carried out the patients treatment/management plans were changed due to the deterioration identified.This suggests that the patients escalated were appropriate.
The researcher checked the notes of the patients not escalated and the treatment/management plans were not changed at the next routine review, indicating that the escalation would not have been appropriate if it had been performed. This finding supports the evidence from Lobo et al. in 2015 where it was discovered that high NEWS did not necessarily result in treatment/management change for the patient. It could be assumed that the nursing staff recognised that the patients did not need escalation and so didn’t request review by the medical team. However on only 4 occasions did the nursing staff explicitly justify not escalating the patients in the patient records. Although the evidence showed that escalations were not performed as often as indicated, if the guidance was followed to the letter this should have happenedevery time or the variance from the guidance should have been documented and justified.
The evidence supports the researcher’s argument that the NEWS leads to inappropriate escalation of care in COPD patients and is therefore not an appropriate assessment tool for this patient group.
Trigger Fatigue.
It could be assumed that the nursing staff assessed the patients and taking into account the diagnosis of COPD and realising the observations were within target range decided not to escalate care. The fact that the patient treatment/management plan was not altered at next review visit supports this theory. However this may not actually be the case in every situation. We know that 48% of the time this patient group hit the trigger scores. The researcher suggests that trigger fatigue could also be a reason for the lack of escalation of patients with a NEWS 5+ or 3 in one domain.
Sendelbach and Funk (2013) suggest that 72-99% of alarms are false and this leads to desensitisation of the healthcare professional. This could be happening to the COPD patients in this study who are ‘alarming’ 48% of the time. The concern is that this desensitisation leads to critical illness and preventable death as the window of opportunity to intervene and save the patient is missed when the escalation to the medical team is not identified and the “alarm” is assumed to be false(Cvach, 2012).
Compliance
Guidelines are developed to support nurses to provide evidence based care. They help the nurse to explain and justify any interventions they make. The use of guidelines strengthens patient treatment quality and contributes to professionalism. Working outside of guidance may be acceptable if there is clear rationale and justification for the variance from the guidance. In this service evaluation on only 4 occasions were the variances from the guidance explained or justified (Senn, Kobleder & Schiess, 2014).
The researcher fully expected to find that observations were recorded too frequently and patient care was escalated unnecessarily but what the researcher didn’t expect was the frequency in which the guidance was not followed. Compliance with the NEWS guidance was poor with only 52% of observations being recorded on time and escalations being carried out just 4% of the time indicated by the tool. This would support the researcher’s argument that the tool is not appropriate for this patient group. It compromises the safety of the patient and the nurse’s registration.
The RCP (2012) does acknowledge that there are times when healthcare professionals should consider long term conditions when interpreting NEWS in case baseline parameters are altered by the condition, butwe should not be using a guideline which requires adjustment for a particular patient group all the time. It is essential that we acknowledge that there will be healthcare professionals with different levels of experience and knowledge using the NEWS tool. Not all patients with COPD exacerbations will be looked after by Respiratory Nurses. Newly qualified nurses or healthcare assistants may be measuring observations and not have the experience to interpret the scores with caution. We have seen that 2 patients were cared for on surgical wards; do they have the knowledge and experience to interpret NEWS for COPD patients?
Whilst the debate may continue for some time on the appropriateness of the NEWS in COPD patients, for the immediate future the researcher intends to present the findings of the study to the Acute Trust. The lack of compliance with the guidance is a huge concern for the researcher and it is important that for the protection of the patient and staff we appropriately use the guidance or document any variances from the guidance. This is the only way we can ensure the safety of the patient and protect the staff. Documenting the variance will ensure that the staff are considering the situation fully and will reduce the risk of trigger fatigue.
The research was completed in one Acute Trust and other Acute Trusts may have a higher rate of compliance with the guidance.
Limitations of the Study.
Some of the limitations of the study have been discussed earlier in the methodology section.
The researcher acknowledges that the study is limited in its application as only one Acute Trust was used with a relatively small sample size. It is likely that most of the staff using the NEWS in this Trust received the same training unless they have moved into the Trust from another healthcare setting and had received previous training. The generalisability of the study is therefore reduced (Robertson, 1994).
The study was performed by one person and although the internal validity is good as the aims and objectives of the study were achieved, there is an argument that the study may have been biased. The researcher interrogated the notes independently and having more than one person completing the study may have reduced the concern about bias. However having more than one person can reduce reliability and therefore it is necessary to have strict parameters and inter-rater reliability must be checked(Heale &Twycross, 2015).
Future considerations.
A multi-centred study looking at the use of the NEWS in COPD patients would help to confirm if the findings at this acute NHS Trust were representative of the rest of the country or if they were particular to this Trust. If this trend is found elsewhere it would support the researcher’s argument that the NEWS is not suitable for this patient group.
It may be that this particular Trust is unique and the findings here are not representative of the rest of the UK. The findings may represent a training need for the healthcare professionals using the NEWS.
It would be useful to perform a qualitative study to discover staff experience of using the NEWS and explore why the guidance wasn’t followed as directed. It may be that the staff are very good at interpreting the NEWS for COPD patients and were confident that the observations didn’t need recording more frequently and they didn’t require escalation. However we cannot just assume that this is the case. It could equally be possible that the staff don’t understand the guidance.
Only further research can explain and support the findings of this study.
Chapter 9. Conclusion
The researcher suggests that this service evaluation supports their view that the use of the NEWS for patients in exacerbation of COPD is not fit for purpose. However the researcher acknowledges that this study is not powerful enough to stop using the NEWS for COPD patients at this Trustjust yet and certainly not for the UK. Further research is absolutely necessary.
If the NEWS guidelines are strictly adhered to, the researcher has shown that the NEWS leads to over escalation of patients and unnecessary observation recording. Modifying the NEWS tool for this group of patients would reduce the frequency of observations needed and reduce the number of patient escalations.
The researcher has also shown that using the NEWS tool for COPD patient may put patient safety at risk from non-compliance of the tool and trigger fatigue and may put the nursing staff at risk from litigation for negligence.
The researcher proposes that a modified NEWS should be adopted which takes into account the altered baseline parameters for COPD patients and usual LTOT prescriptions.
This study has looked at the literature available on the use of the NEWS in COPD patients. It has identified the findings from other studies and has built on them. It has taken research where the NEWS has been modified for COPD patients and developed that modified tool. It has looked at different outcomes than the individual studies and found evidence which supports previous studies.
The researcher suggests that further research should be performed to discover the merits of continuing to use the NEWS for COPD patients. The researcher has discussed some of the research that may be useful going forward. A meta-analysis of all the research performed in this area would also be beneficial.
The researcher has chosen to submit this study as a journal article to the Nursing Times. Although the study subject is focused on a respiratory diagnosis, the NEWS is used by all nurses in secondary care and this study is relevant to all healthcare professionals working with this patient group. It is more relevant to nursing staff that may not have respiratory experience and may not be as aware of the need to take into account altered baseline parameters.
Appendix 1.
Appendix 2.
Appendix 3.
Appendix 4.
|
Physiological Parameters |
3 |
2 |
1 |
0 |
1 |
2 |
3 |
|
Respiration Rate |
≤8 | 9-11 | 12-23 | 23-25 | >25 | ||
| Oxygen saturations | ≤85 | 86-87 | 88-89 | ≥90 | |||
| New/ altered supplementary oxygen | Yes | No | |||||
|
Temperature |
≤35.0 | 35.1-36.0 | 36.1-38.0 | 38.1-39.0 | ≥39.1 | ||
|
Systolic BP |
≤90 | 91-100 | 101-110 | 111-219 | ≥220 | ||
|
Heart Rate |
≤40 | 41-50 | 51-90 | 91-110 | 111-130 | ≥131 | |
|
Level of Consciousness |
A | V,P or U |
Modified Early Warning Score for COPD patients
Appendix 5. Literature Search Strategy
| No. | Database | Search Terms | Results | Advanced search |
| 1 | CINAHL | (NEWS) | 40,241 | Title, abstract |
| 2 | CINAHL | (COPD) | 8732 | Title, abstract |
| 3 | CINAHL | (NEWS) AND (COPD) | 27 | Title, abstract |
| 4 | CINAHL | (‘National Early Warning Score’) | 16 | Title, abstract |
| 5 | CINAHL | (COPD) AND (‘National Early Warning Score’) | 0 | Title, abstract |
| 6 | CINAHL | (‘Modified national early warning score’) | 1 | Title, abstract |
| 7 | CINAHL | (observations) | 28,792 | Title, abstract |
| 8 | CINAHL | (COPD) AND (observation) | 114 | Title, abstract |
| 9 | CINAHL | *“Pulmonary Disease, Chronic Obstructive”/ OR *“Lung Diseases, obstructive”/ | 8839 | |
| 10 | CINAHL | (‘National Early Warning Score’) AND (*“Pulmonary Disease, Chronic Obstructive”/ OR *“Lung Diseases, Obstructive”/) | 0 | Title, abstract |
| 11 | CINAHL | (‘modified national early warning score’) AND (*“Pulmonary Disease, Chronic Obstructive”/ OR *“Lung Diseases, Obstructive”/) | 0 | Title, abstract |
| 12 | CINAHL | *“Pulmonary Disease, Chronic Obstructive”/ OR *“Lung Diseases, Obstructive”/ | 7256 | Nursing |
| 13 | Medline | *“Pulmonary Disease, Chronic Obstructive”/ | 22743 | |
| 14 | Medline | (‘National Early Warning Score’) | 88 | Title, abstract |
| 15 | Medline | *“Pulmonary Disease, Chronic Obstructive”/ AND (‘National Early Warning Score’) | 0 | Title, abstract |
| 16 | CINAHL | (‘Early Warning Score’) | 124 | Title, abstract |
| 17 | CINAHL | (COPD) AND (‘Early Warning Score’) | 0 | Title, abstract |
| 18 | CINAHL | (chronic hypoxaemia’) | 4 | Title, abstract |
| 19 | CINAHL | ((COPD) AND (‘early warning score’)) AND (‘chronic hypoxaemia’) | 0 | Title, abstract |
| 20 | Medline | (‘Chronic hypoxaemia’) | 597 | Title, abstract |
| 21 | Medline | (‘early warning score’) | 440 | Title, abstract |
| 22 | Medline | (‘chronic hypoxaemia’) AND (‘early warning score’) | 1 | Title, abstract |
| 23 | Summon | (‘National Early Warning Score’) | 30,515 | |
| 24 | Summon | (‘National Early Warning Score’) AND (COPD) | 3433 | |
| 25 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 3433 | |
| 26 | Summon | *“National Early Warning Score”/OR “Early Warning Score” AND (COPD) AND (‘Trigger Fatigue’) | 241 | |
| 27 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 530 | Journals |
| 28 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 509 | 2000-2017 |
| 29 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 430 | 2007-2017 |
| 30 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 422 | 2007-2017, scholarly articles, peer reviewed. |
| 31 | Summon | (‘National Early Warning Score’) AND ((COPD)/ OR (‘Early Warning Score’)) | 10 | Title, abstract, Journals, 2007-2017, scholarly articles, peer reviewed. |
Appendix 6. Data Analysis
| A | B | C | D | E | F | G | H | I | J | K | L |
| 1 | 2 | 5 | 0/2 | 0/0 | 0/0 | 0 | 0 | 0 | 80% | 0 | N |
| 2 | 3 | 7 | 0/1 | 1/0 | 0/0 | 0 | 0 | 1 | 14% | 0 | N |
| 3 | 3 | 17 | 3/3 | 4/1 | 0/0 | 0 | 0 | 4 | 94% | 0 | N |
| 4 | 2 | 6 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 5 | 9 | 36 | 6/14 | 12/1 | 1/0 | 0 | 0 | 12 | 36% | 2 | N |
| 6 | 4 | 11 | 1/8 | 3/0 | 0/0 | 0 | 0 | 3 | 36% | 0 | N |
| 7 | 8 | 24 | 2/20 | 13/0 | 0/0 | 0 | 0 | 13 | 16% | 0 | Y |
| 8 | 18 | 35 | 6/17 | 27/13 | 0/0 | 0 | 0 | 27 | 43% | 0 | N |
| 9 | 4 | 26 | 6/19 | 19/0 | 0/0 | 0 | 0 | 19 | 50% | 0 | N |
| 10 | 3 | 11 | 0/8 | 5/0 | 0/0 | 0 | 0 | 5 | 18% | 0 | N |
| 11 | 7 | 23 | 5/7 | 1/0 | 0/0 | 0 | 0 | 1 | 70% | 0 | N |
| 12 | 2 | 4 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 0% | 0 | N |
| 13 | 10 | 62 | 9/34 | 40/9 | 7/0 | 3 | 0 | 37 | 37% | 0 | N |
| 14 | 10 | 35 | 0/17 | 17/3 | 4/0 | 0 | 0 | 17 | 14% | 0 | N |
| 15 | 1 | 2 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 16 | 4 | 38 | 9/26 | 29/5 | 1/0 | 1 | 0 | 28 | 37% | 5 | Y |
| 17 | 2 | 4 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 18 | 2 | 7 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 19 | 8 | 26 | 8/26 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 20 | 2 | 3 | 0/0 | 0/0 | 0/0 | 0 | 0 | 0 | 0% | 0 | N |
| 21 | 2 | 6 | 0/1 | 1/0 | 0/0 | 0 | 0 | 1 | 80% | 0 | N |
| 22 | 7 | 31 | 7/13 | 1/0 | 0/0 | 0 | 0 | 1 | 68% | 0 | N |
| 23 | 5 | 31 | 12/20 | 22/6 | 2/0 | 0 | 0 | 22 | 68% | 0 | N |
| 24 | 3 | 23 | 8/14 | 11/0 | 3/0 | 0 | 0 | 11 | 73% | 0 | N |
| 25 | 5 | 20 | 1/8 | 8/2 | 3/0 | 1 | 0 | 7 | 42% | 0 | N |
| 26 | 2 | 9 | 0/3 | 1/0 | 0/0 | 0 | 0 | 1 | 67% | 0 | N |
| 27 | 6 | 19 | 1/15 | 17/4 | 2/0 | 4 | 0 | 13 | 17% | 0 | N |
| 28 | 4 | 40 | 12/29 | 27/5 | 1/1 | 0 | 0 | 27 | 49% | 0 | N |
| 29 | 1 | 5 | 1/1 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 30 | 3 | 10 | 3/8 | 0/0 | 3/0 | 0 | 0 | 0 | 44% | 0 | N |
| 31 | 4 | 17 | 0/2 | 3/1 | 1/0 | 0 | 0 | 3 | 65% | 0 | N |
| 32 | 1 | 7 | 1/2 | 2/0 | 0/0 | 0 | 0 | 2 | 50% | 0 | N |
| 33 | 3 | 16 | 3/5 | 5/0 | 0/0 | 0 | 0 | 5 | 80% | 0 | N |
| 34 | 1 | 7 | 0/5 | 5/0 | 1/1 | 0 | 0 | 5 | 17% | 0 | N |
| 35 | 4 | 26 | 14/18 | 3/0 | 1/0 | 0 | 0 | 3 | 73% | 0 | N |
| 36 | 4 | 18 | 0/6 | 6/0 | 0/0 | 0 | 0 | 6 | 35% | 0 | N |
| 37 | 1 | 2 | 0/2 | 2/0 | 0/0 | 0 | 0 | 2 | 0% | 0 | N |
| 38 | 1 | 1 | 0/1 | 0/0 | 0/0 | 0 | 0 | 0 | 100% | 0 | N |
| 39 | 3 | 21 | 3/13 | 16/6 | 0/0 | 2 | 0 | 14 | 43% | 0 | Y |
| 40 | 1 | 3 | 0/0 | 2/2 | 1/1 (BP) | 0 | 0 | 0 | 0% | 0 | Y |
| 41 | 2 | 7 | 0/3 | 3/0 | 0/0 | 0 | 0 | 0 | 17% | 0 | N |
| 42 | 1 | 4 | 0/1 | 2/1 | 0/0 | 0 | 0 | 2 | 0% | 0 | N |
| 43 | 4 | 21 | 3/8 | 5/0 | 6/0 | 0 | 0 | 5 | 70% | 0 | N |
| 44 | 5 | 25 | 3/11 | 12/6 | 4/0 | 6 | 0 | 6 | 46% | 0 | N |
| 45 | 1 | 4 | 1/2 | 0/0 | 1/0 | 0 | 0 | 0 | 100% | 0 | N |
| 46 | 2 | 11 | 2/5 | 4/0 | 0/0 | 0 | 0 | 4 | 55% | 0 | N |
| 47 | 3 | 13 | 3/7 | 8/2 | 0/0 | 0 | 0 | 8 | 58% | 0 | N |
| 48 | 3 | 10 | 2/4 | 1/0 | 1/0 | 0 | 0 | 1 | 44% | 0 | N |
| 186 | 789 | 135/409 | 338/67 | 43/3 | 17 | 0 | 316 | 52% | 7 | Y=4 |
Key to results columns:
A Patient number
B Days in Hospital
C Number of observations analysed
D Number of unnecessary observations according to mNEWS
E Number of escalations indicated NEWS/mNEWS (score 5+)
F Number of escalations indicated by NEWS/mNEWSscore 3-4 in one domain
G Number of escalations performed
H Number of unnecessary escalations performed
I Number of escalations indicated but not acted upon or needed
J % of observations recorded on time as indicated by NEWS
K Triggers missed by mNEWS
L Variance to the NEWS protocol justified/explained in the medical records.
Appendix 7. Data Analysis continued.
| Patient | Location of patient on discharge | Average NEWS | Average mNEWS | Discharge NEWS | Discharge mNEWS |
| 1 | Hospital Site B – Short Stay Medical Ward | 2.6 | 1 | 2 | 0 |
| 2 | Hospital Site A – Respiratory Ward No. 1 | 2 | 2 | 2 | 2 |
| 3 | Hospital Site B – Medical Admission Unit | 3.76 | 2.58 | 8 | 7 |
| 4 | Hospital Site B – Medical Admission Unit | 1.17 | 0.5 | 1 | 0 |
| 5 | Hospital Site A – Respiratory Ward No. 1 | 3.86 | 2.55 | 5 | 4 |
| 6 | Hospital Site A – Respiratory Ward No. 2 | 3.73 | 1 | 3 | 0 |
| 7 | Hospital Site A – Respiratory Ward No. 2 | 4.92 | 1.42 | 4 | 0 |
| 8 | Hospital Site A – Respiratory Ward No. 1 | 6 | 4.51 | 3 | 2 |
| 9 | Hospital Site A – Stroke Ward | 4.85 | 2.27 | 6 | 3 |
| 10 | Hospital Site A – Respiratory Ward No. 1 | 3.82 | 1.82 | 2 | 0 |
| 11 | Hospital Site A- Respiratory Ward No. 1 | 1.48 | 0.83 | 0 | 0 |
| 12 | Hospital Site A- Extra Medical Capacity | 1 | 1 | 1 | 1 |
| 13 | Hospital Site A – Respiratory Ward No. 2 | 6.11 | 3.21 | 3 | 1 |
| 14 | Hospital Site A – Respiratory Ward No. 2 | 4.57 | 2.63 | 2 | 1 |
| 15 | Hospital Site A – Medical Assessment Unit | 1 | 0.5 | 2 | 1 |
| 16 | Hospital Site A – Respiratory Ward No. 2 | 5.39 | 2.47 | 5 | 3 |
| 17 | Hospital Site B – Short Stay Medical Ward | 0 | 0 | 0 | 0 |
| 18 | Hospital Site B – Medical Admission Unit | 2 | 1.7 | 1 | 1 |
| 19 | Hospital Site B – Elderly Medical Ward | 1.81 | 0.73 | 1 | 0 |
| 20 | Hospital Site B – Medical Admission Unit | 1.6 | 1 | 3 | 1 |
| 21 | Hospital Site A – Medical Assessment Unit | 3.67 | 2 | 4 | 3 |
| 22 | Hospital Site A – Respiratory Ward No. 1 | 1.87 | 0.84 | 1 | 0 |
| 23 | Hospital Site A – Respiratory Ward No. 2 | 5.23 | 3 | 4 | 2 |
| 24 | Hospital Site B – Respiratory Ward | 4.78 | 1.74 | 2 | 0 |
| 25 | Hospital Site A – Respiratory Ward No. 2 | 4.2 | 2.7 | 3 | 1 |
| 26 | Hospital Site A – Medical Admission Unit | 2.2 | 1 | 3 | 1 |
| 27 | Hospital Site A – Respiratory Ward No. 1 | 5.79 | 3.16 | 4 | 1 |
| 28 | Hospital Site A – Respiratory Ward No. 2 | 5.73 | 2.23 | 3 | 1 |
| 29 | Hospital Site B – Short Stay Medical Ward | 2.6 | 1.8 | 4 | 3 |
| 30 | Hospital Site A – Respiratory Ward No. 2 | 5.4 | 0.7 | 3 | 0 |
| 31 | Hospital Site B – Respiratory Ward | 3.12 | 2.7 | 3 | 1 |
| 32 | Hospital Site B – Short Stay Medical Ward | 3.29 | 2.29 | 0 | 0 |
| 33 | Hospital Site B – Short Stay Medical Ward | 4.06 | 2.81 | 4 | 3 |
| 34 | Hospital Site B – Medical Admission Unit | 4.86 | 2.71 | 4 | 4 |
| 35 | Hospital Site B – Female Surgical Ward | 3 | 0.62 | 1 | 1 |
| 36 | Hospital Site A – Respiratory Ward No. 2 | 4.33 | 2.5 | 4 | 2 |
| 37 | Hospital Site B – Respiratory Ward | 5 | 2 | 5 | 1 |
| 38 | Hospital Site B – Medical Assessment Unit | 1 | 0 | 1 | 0 |
| 39 | Hospital Site B – Short Stay Medical Ward | 6.14 | 3.14 | 6 | 1 |
| 40 | Hospital Site B – Elderly Medical Ward | 4.6 | 4.6 | 4 | 4 |
| 41 | Hospital Site A – Medical Assessment Unit | 4.71 | 2.57 | 2 | 2 |
| 42 | Hospital Site A – Medical Assessment Unit | 3.75 | 2.5 | 0 | 0 |
| 43 | Hospital Site B – Male Surgical Ward | 3.19 | 1.57 | 3 | 1 |
| 44 | Hospital Site A – Respiratory Ward No. 2 | 5.64 | 3.12 | 1 | 0 |
| 45 | Hospital Site B – Medical Admission Unit | 1.5 | 0.5 | 1 | 0 |
| 46 | Hospital Site A – Respiratory Ward No. 2 | 4.09 | 1.36 | 3 | 1 |
| 47 | Hospital Site A – Short Stay Medical Ward | 4.77 | 3 | 5 | 3 |
| 48 | Hospital Site B – Respiratory Ward | 2.6 | 1.4 | 2 | 0 |
| 3.6 | 1.9 |
Appendix 8. Journal Article.
Appendix 9 Journal Article Link.
https://www.nursingtimes.net/home/author-guidelines
References
Abdo, W. F., & Heunks, L. M. A. (2012). Oxygen-induced hypercapnia in COPD: Myths and facts. Critical Care (London, England), 16(5), 323. doi: 10.1186/cc11475
Aveyard , H., Sharp, P. (2009). A beginners guide to evidence based practice in health and social care. Berkshire: Open University Press.
Bilben, B., Grandal, L., & Sovik, S. (2016). National early warning score (NEWS) as an emergency department predictor of disease severity and 90-day survival in the acutely dyspneic patient – a prospective observational study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 24(1). doi: 10.1186/S13049-016-0273-9
Boote, D.N., & Beile, P. (2005). Scholars before Researchers: On the Centrality of the Dissertation Literature Review in Research Preparation. Educational Researcher, 34 (6), 3-15. doi: 10.3102/0013189X034006003
Bowling, A., & Ebrahim, S. (2005). Handbook of health research methods: Investigation, measurement and analysis. Maidenhead: Open University Press.
Brink, P.J., & Wood, M.J. (2001). Basic steps in Planning Nursing Research. (5th ed.). London: Jones and Bartlett publishers.
Burns, P.B., Rohrich, R.J., & Chung, K.C. (2011). The levels of evidence and their role in evidence-based medicine. doi: 10.1097/PRS.0b013e318219c171
Caldecott, F. (2013).The Information Governance Review
Retrieved from https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/192572/2900774_InfoGovernance_accv2.pdf
Clifford, C. (1997). Nursing and Health Care Research. A skills-based introduction. (2nd ed.). Hemel Hempstead: Prentice Hall.
Currie, G. P. (2007). ABC of COPD. London: BMJ.
Cuthbertson, B.H., & Smith, G.B. (2007).A warning on early-warning scores!British Journal of Anaesthesia 98 (6): 704–6. doi: 10.1093/bja/aem121
Cvach, M. (2012). Monitor alarm fatigue: an integrative review. Biomedical Instrumentation and Technology, 46, 268-277. doi: 10.2345/0899-8205-46.4.268
Data Protection Act 1998 London: Stationery Office Ltd.
Department of Health. (2011). An Outcomes Strategy for Chronic Obstructive Pulmonary Disease (COPD) and Asthma in England. London: DH.
Doolen, J. (2017). Meta-analysis, systematic, and integrative reviews: An overview. Clinical Simulation in Nursing, 13(1), 28-30. doi:10.1016/j.ecns.2016.10.003
Eccles, S.R., Subbe, C., Hancock, D., & Thomson, N. (2014). CREWS: Improving specificity whilst maintaining sensitivity of the National Early Warning Score in patients with chronic hypoxaemia. Resuscitation,85(1), 109-111.doi:10.1016/j.resuscitation.2013.08.277
Eccles, S., Subbe, C., Hancock, D., & Thomson, N. (2013). M28 from NEWS to CREWS: The chronic respiratory early warning score for patients with chronic hypoxaemia. Thorax, 68, A207. doi:10.1136/thoraxjnl-2013-204457.438
Fry, S.T. & Johnstone, M-J. (2008). Ethics in Nursing Practice. (3rd ed.). West Sussex: Blackwell Publishing.
Gallagher, U. & Boyd, K.M. (1991). Teaching and Learning Nursing Ethics. Middlesex: Scutari Press.
Gerrish, K., & Lacey, A. (2006). The Research Process in Nursing. (5th Ed.). Oxford: Blackwell Publishing.
Haber, J., Whitehead, D., Schneider, Z. &LoBiondo-Wood, G. (2012). Nursing and midwiferyresearch: Methods and appraisal for evidence based practice. Mosby.
Heale, R., & Twycross, A. (2015). Validity and reliability in quantitative studies. Evidence-Based Nursing, 18(3), 66-67. doi:10.1136/eb-2015-102129
Hodgson, L.E., Dimitrov, B.D., Congleton, J., Venn, R., Forni, L.G., & Roderick, P.J. (2017). A validation of the national early warning score to predict outcome in patients with COPD exacerbation. Thorax, 72 (1), 23-30. doi:10.1136/thoraxjnl-2016-208436
Holloway, I. & Wheeler, S. (2010). Qualitative Research in Nursing and Healthcare. (3rd ed.). Oxford: Wiley-Blackwell.
Holmes, S. & Scullion J. (2015). A changing landscape: diagnosis and management of COPD. British Journal of Nursing, 24(8), 432-440. doi: 10.12968/bjon.2015.24.8.432
Holzemer, W.L. (2010). Improving health through nursing research. Oxford: Wiley-Blackwell.
Jolley, J. (2013). Introducing Research & Evidence-Based Practice for Nursing & Healthcare Professionals. (2nd ed.). Essex: Pearson Education Ltd.
Jones, M. (2012) NEWSDIG: The National Early Warning Score Development and Implementation Group.Clinical Medicine, 12(6), 501-503.
Kane, B., Decalmer, S., Murphy, P., Turkington, P., & O’Driscoll, B. (2012). S29 the proposed national early warning system (NEWS) could be hazardous for patients who are at risk of hypercapnic respiratory failure. Thorax, 67, A16. doi:10.1136/thoraxjnl-2012-202678.035
Lee, A., Bishop, G., Hillman, K.M., & Daffurn, K. (1995).The Medical Emergency Team. Anaesth Intensive Care, 2, 183-186.
Lobo., R., Lynch, K., & Casserly, L.F. (2015). Cross-Sectional audit on the relevance of Eleavated National Early Warning Score in medical patients at a Model 2 hospital in Ireland. Irish journal of medical science, 184(4), 893-898. doi: 10/1007/s11845-01401216-y
Maltby, J., Williams, G., McGarry, J., & Day, L. (2010). Research methods for nursing and healthcare. Oxon: Routledge.
Malicki, M., Marusic, A. (2014). Is there a solution to publication bias? Researchers call for changes in dissemination of clinical research results. Journal of Clinical Epiedemiology, 67(10), 1103-1110. doi:10/1016/j.jclinepi.2014.06.002
Melnyk, B.M., Fineout-Overholt, E. (2011). Evidence-Based Practice in Nursing and Healthcare. A Guide to Best Practice. China: Lippincott, Williams and Wilkins.
Mitchell, J. (2015). Pathophysiology of COPD: Part 1. Practice Nursing, 26(4), 172-178. doi: 10.12968./pnur.2015.26.4.172
Murphy, S.A., Mydin, H.H., Fatah, S., & Antunes, G. (2010). Predicting end-of-life in patients with an exacerbation of COPD by routine clinical assessment. Respiratory Medicine, 104, 1668-1674. doi: 10.1016/j.rmed.2010.04.025
National Patient Safety Agency. (2007). Safer care for the Acutely Ill Patient: learning from serious incidents. London: NPSA.
National Institute for Clinical Excellence. (2010). Management of Chronic Obstructive Pulmonary Disease in adults in Primary and Secondary Care. Retrieved from http://www.nice.org.uk/guidance/cg12
National Institute for Clinical Excellence. (2007). Acutely ill patients in hospital: Recognition and Response to acute illness in adults in hospital. NICE: London.
National Research Ethics Service (NRES).(2013). Defining Research.
Retrieved from http://www.nres.nhs.uk/EasySiteWeb/GatewayLink.aspx?alld=355
NHS England. (2014). A resource to support commissioners in setting a level of ambition on reducing premature mortality. London: NHS England.
Nursing and Midwifery Council (NMC), (2015). The Code: Standards of conduct, performance and ethics for nurses and midwives. Retrieved from http://www.nmc-uk.org/Publications/Standards/The-code/Introduction/
O’Driscoll, B.R. (2012).Acute Monitoring of patients with chronic respiratory disease during hospital admission. Clinical Medicine, 12, 79-81.doi: 10.7861/clinmedicine.12-1-79
Parahoo, K. (2006). Nursing Research: Principles, process and issues. (2nd Ed.). Hampshire: Palgrave Macmillan.
Polit, D., & Beck, C. (2014). Essentials of Nursing Research: Appraising Evidence for Nursing Practice(8thEd). Philadelphia: Lippincott, Williams and Wilkins.
Rees, P.J., & Calverley, P.M.A. (2002). Handbook of Chronic Obstructive Pulmonary Disease. London: Dunitz.
Robertson, J. (1994). Handbook of Clinical Research. Edinburgh: Churchill Livingstone.
Roe, B., & Webb, C. (1998). Research and Development in Clinical Nursing Practice. London: Whurr Publishers.
Royal College of Physicians. (2012). National Early Warning Score NEWS): Standardising the assessment of acute-illness severity in the NHS. Report of a working party. London: RCP.
Royal College of Nursing. (2012). National Early Warning Score online training resource. Retrieved from http://www.rcn.org.uk/development/practice/clinical_governance/quality_improvement/rcn_publications
Sendelbach, S.& Funk, M. (2013). Alarm Fatigue: A patient safety concern. AACN Advanced Critical Care, 24(4), 378-386. doi:10.1097/NCI.0b013e3182a903f9
Senn, B., Kobleder, A. & Schiess, C. (2014). Evidence-Based Guidelines as a Necessity for Advanced Practice Nurses. Annals of Nursing Practice, 1(2), 1010.
Smith, S. (2013). Early warning scores: effective use. Nursing Times, 107, (3). Retrieved from http://www.nursingtimes.net/Journals/2013/01/18/y/h/d/250111Early-warning-scores–effective-use.pdf
Smith, G. B., Prytherch, D.R., Schmidt, P.E., & Featherstone, P.I. (2008). Review and performance evaluation of aggregate weighted ‘track and trigger’ systems. Resuscitation, 77, 170-179. doi: 10.1016/j.resuscitation.2007.12.004
Smith, G. B., Prytherch D.R., Meredith, P., Schmidt, P.E., & Featherstone, P.I. (2013). The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. 84, (4), 465–470. doi: 10.1016/j.resuscitation.2010.04.014
Smith, J., & Noble, H. (2014). Bias in Research. Evidence Based Nursing, 17, 100-101. doi:10.1136/eb-2014-101946
Sprinks, J. (2013). Swift take-up of standardised early warning system across NHS Trusts. Nursing Standard 27 (21), 7. doi: 10.7748/ns2013.01.27.21.7.p10293
Subbe, C.P. (2010). Better ViEWs ahead? It is high time to improve patient safety by standardising Early Warning Scores. Resuscitation, 17(6), 349-358. doi: 10.1016/j.resuscitation.2010.05.013
Tingle, J. (2000) Clinical Negligence: The professional standard of care in clinical negligence. British Journal of Nursing, 11(21), 1375-1377. doi: 10.12968/bjon.2002.11.19.10758
Twycross, A. & Shorten, A. (2014). Service evaluation, audit and research: what is the difference? Evidence based Nursing, 17(3), 65-66. doi: 10.1136/eb-2014-101871
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medical"
The word Medical refers to preventing or treating injuries or illnesses, relating to the study or practice of medicine. Medical care involves caring for a patient and helping them through their journey to recovery.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




