Anatomy of the Posterior Orbit and Orbital Apex
Info: 3982 words (16 pages) Dissertation
Published: 9th Dec 2019
Tagged: Neurology
Question:
An adult patient is found to have a small lesion located within the lateral aspect of the posterior orbit. Give a detailed account of the anatomy of the posterior orbit and orbital apex (75%). With reference to your account, describe sequentially the clinical signs and symptoms that may manifest as the lesion increases in size (15%). With reference to orbital anatomy, discuss a surgical approach that may be appropriate for removal of such a lesion (10%).
Introduction
The bony orbit houses many important ocular tissues that makes visual perception and movement of the globe possible(1). Specifically, the eye is enclosed by a series of connective tissue, musculature, vasculature, nervous tissue and fat tightly contained within a cavity (2). The trajectories of these structures is possible by way of openings located within skeletal tissue that adjoin one-another (1). This essay will outline the gross anatomy of the orbit with specific reference to the apex and its related structures, followed by the discussion of compromise of the posterior orbit secondary to mass effect and describe surgical interventions pertaining to management.
Anatomy of the orbit and orbital apex
The orbit comprises of seven bones, namely, the frontal, maxilla, ethmoid, sphenoid, palatine, zygomatic and lacrimal bones (3). The concave roof is formed by the orbital plate of the frontal bone anteriorly and the lesser wing of the sphenoid bone posteriorly (2, 3). The thin and oblong medial wall is formed by the lacrimal bone, orbital plate of the ethmoid bone, frontal process of the maxilla and body of the sphenoid bone (2-4). The thick lateral wall is formed by the interaction of the orbital surface of the greater wing of the sphenoid bone posteriorly and the zygomatic bone anteriorly, projecting approximately 45
⁰postero-medially in relation to the sagittal plane (2, 3). The triangular floor of the orbit is formed a combination of maxilla (orbital plate), zygomatic (orbital surface) and palatine (orbital process) bones, which projects postero-superiorly (2-4). The resulting four sided structure resembles a pyramid, measuring approximately 3.5cm in height, 4cm in width and 4-5cm in length with its base located anteriorly and apex posteriorly (2-4).
The posterior orbit is mainly formed by the body, greater and lesser wings of the sphenoid bone (posteriorly and laterally), palatine bone (inferiorly) and the posterior portion of the orbital plate of the ethmoid bone (laterally) (3, 5). The orbital apex located within the posterior orbit, comprises of the optic canal (OC), superior orbital fissure (SOF) and the posterior margin of the inferior orbital fissure (IOF) (4). These orifices provide a means of communication between the orbit and cranium, allowing for the entrance of neurovascular structures (3). Enclosing these components within the orbit are connective tissues formed by the periorbita, Tenon’s capsule, medial and lateral check ligaments, superior suspensory ligament (of Whitnall), and inferior ligament (of Lockwood) (2, 3). The combination of neurovascular, connective and soft tissue structures gives rise to intra-orbital spaces which are occupied by fat pads, forming a tightly contained cavity (1, 5).
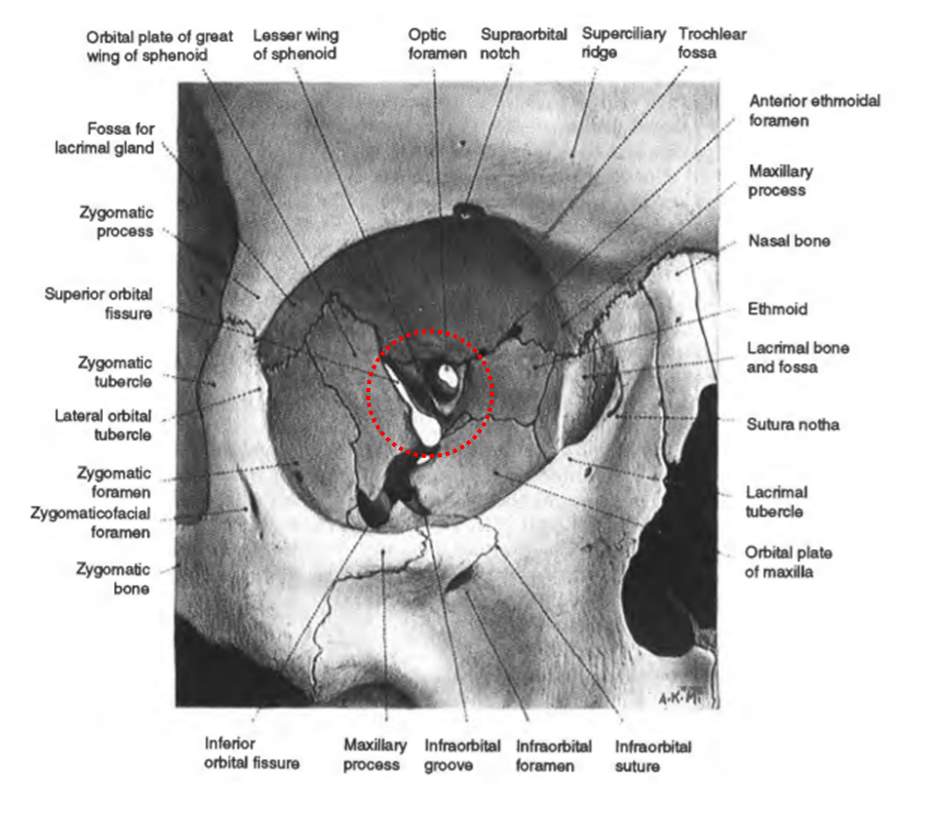
Figure 1. Diagram showing the labelled orbit (3). The diagram has been modified to outline the posterior orbit and orbital apex (represented by the dotted red circle).
Optic Canal
The OC is located within the superior part of the posterior orbital wall and is formed by the different elements of the sphenoid bone, where the body gives rise to the medial wall, the lesser wing gives rise to the roof and a bony strut between the body and anterior clinoid process gives rise to the lateral wall (3, 4). A variation of the medial wall (by extension of the posterior ethmoidal air cells into the medial wall) has been noted in up to 50% of the cases, and is associated with a longer OC (3, 4). The OC extends 8mm supero-medially (at an angle of 45⁰ and 15
⁰respectively) from its oval intraorbital orifice to its circular intracranial portion and allows communication between the middle cranial fossa and the orbit (3, 6). The canal transmits the optic nerve and its surrounding meninges which is responsible for the sense of vision (2, 3). The ophthalmic artery traverses infero-laterally to the optic nerve, and also carries a proportion of post-ganglionic sympathetic fibres (from the superior cervical ganglion) into the orbit (1, 6).
Superior orbital fissure
The SOF is moulded by the interaction between the greater and lesser wing of the sphenoid bone to form a comma shaped space separating the posterior roof and lateral orbital wall (3, 5, 7). The SOF is located below the OC, separated by the lesser wing of the sphenoid’s posterior root and anterior to the cavernous sinus (3, 4). Typically the SOF consists of a wide medial portion and narrow superotemporal portion, spanning approximately 22mm in length and allows for the orbit to communicate with the middle cranial fossa (3, 4). Reymond et al., (2008) showed there can be two broad variations with regard to SOF morphology, based on whether or not a clear narrowing is present within the fissure (8). The latter is also found to be shorter in length (8).
Over the medial aspect of the typical SOF is a fibrous ring, known as the annulus of Zinn which is the attachment site of the extraocular muscles (EOMs) (1, 9). This annulus is made up of the superior and inferior tendons located above and below the optic canal respectively (1). The superior tendon serves as an insertion for the superior rectus (SR) and superior head of the lateral rectus (LR), whereas the inferior tendon anchors the inferior rectus (IR), medial rectus (MR) and LR (1). The super oblique (SO) and inferior oblique (IO) muscles arise from the body of the sphenoid and medial orbital floor (lateral to the nasolacrimal canal) respectively (1, 5). Additionally, the levator palpabrae superioris (LPS) arises from the inferior surface of the lesser wing of the sphenoid bone, at the orbital apex (1, 5). All EOMs have variable insertions onto the sclera, in contrast to the LPS, which inserts onto the skin of the upper eyelid (skeletal muscle component) and superior tarsal plate of the upper lid (smooth muscle component) (1, 5).
Structures within the SOF can be further categorised as extra or intraconal depending on whether the muscle cone overlies their paths.
Extraconal SOF
The lacrimal nerve (a branch of the ophthalmic nerve), transverses the lateral portion of the SOF, running in parallel with the LR within the supero-lateral orbit (9, 10). It synapses with the lacrimal gland to provide it with both parasympathetic and sympathetic innervation (3, 5, 10, 11). It further travels within the orbit to terminate on the lateral edge of the upper eyelid by perforating the orbital septum, supplying the conjunctiva and skin of the lateral edge of the eyelid with sensory fibres (3, 10). Medial to the lacrimal nerve is the frontal nerve, another branch of the ophthalmic nerve (3, 10). This runs between the LPS and SR and divides into the supraorbital and supratrochlear nerves (3, 9, 10). The former exits the orbit by the supraorbital foramen to provide sensory innervation to several structures including the upper eyelid, forehead and scalp as far back as the vertex of the skull (3, 10). The latter travels above the trochlear of the SO to provide sensation to the conjunctiva, medial upper eyelid and forehead (3, 10). The trochlear nerve is located laterally, adjacent to the annulus of Zinn and travels within the periorbital fat anteromedially, to provide motor innervation to the SO (2, 12). This allows for depression and intorsion of the eyeball (especially in abduction) (2, 12). The superior ophthalmic vein (SOV) is located inferiorly within the lateral aspect of the SOF between the trochlear nerve and the annulus (1, 2, 4). It is formed at the anastomosis of the supraorbital, angular and supratrochlear veins at the anterior orbital margin and allows drainage of the supero-medial orbit into the cavernous sinus (1).
Intraconal SOF
Both divisions of the oculomotor nerve (CN III) pass medially within the muscle cone (3, 4). The SR and LPS are innervated by the superior division allowing for elevation of the globe and eyelid respectively, whilst the MR, IR and IO receive innervation by the inferior division’s medial, central and lateral roots allowing for medial, superior and inferior movement of the globe respectively (1, 3). In addition, the lateral root also gives rise to parasympathetic pre-ganglionic fibres, which synapses within the ciliary ganglion and subsequently onto the ciliary muscle and sphincter pupillae (the constrictor of the iris) allowing for both the accommodative reflex and light reflex (3, 4). Furthermore, the nasociliary nerve (the third branch of the ophthalmic nerve) passes between the two divisions of CN III (3, 4). Early during its course it provides a sensory branch to ciliary ganglion and subsequently crosses the optic nerve, giving rise to the two long ciliary nerves that allows for both corneal and ciliary body sensation (5, 10). Additionally, the long ciliary nerve provides sympathetic innervation to the dilator pupillae and ciliary body allowing for pupillary dilatation and inhibition respectively (5, 11). Additionally, it gives rise to the posterior ethmoidal nerve (providing sensation to the sphenoidal and posterior ethmoidal sinuses) and infratrochlear nerve (providing sensation to the medial eyelid, conjunctiva, and mendal canthal structures) (5, 11). It terminates as the anterior ethmoidal nerve which provides sensation to the anterior ethmoidal air cells and dura mater of the anterior cranial fossa (5, 11). The abducens nerve is located infero-medial to the inferior division of CN III in the SOF and deviates laterally to innervate the medial surface of LR (3, 4). The inferior ophthalmic vein (IOV) joins the SOV at the level of the SOF, however, the IOV also has a branch which tranverses through the SOF inferior to the annulus to drain the infero-lateral orbit into the pterygoid plexus (1).
| Foramen | Structures | Purpose |
| OC | Optic nerve | Vision |
| Ophthalmic artery | Arterial supply to eye | |
| Sympathetic fibres | Vasomotor to vessels | |
| SOF (extraconal) | Lacrimal nerve | Autonomic innervation to lacrimal gland, sensation to upper lid and conjunctiva |
| Frontal nerve | Sensation to the upper lid, forehead and scalp | |
| Trochlear nerve | Motor innervation to SO | |
| Superior ophthalmic vein | Drains supero-medial orbit | |
| Inferior ophthalmic vein | Drains infero-lateral orbit | |
| SOF (intraconal) | Superior division CN III | Motor to SR and LPS for elevation of eye and eyelid |
| Inferior division of CNIII | Motor to MR, IR and IO and parasympathetic supply to iris and ciliary muscle | |
| Nasociliary nerve | Sensation to the cornea and ciliary body.
Sympathetic supply to the dilator pupillae |
|
| Abducens nerve | Motor supply to LR |
Table 1. Summarising the foramen of the orbital apex, associated structures and functions.
Inferior orbital fissure
The IOF is located inferior to the annulus of Zinn and posteriorly separates the lateral zygomatic bone from the inferior maxillary bone. It allows communication of the orbit with the pterygopalatine and temporal fossae and transmits the zygomatic nerves, infraorbital vessels and a branch of the inferior ophthalmic vein (1, 3, 4). The canal lies external to the orbital apex (2, 13).
Orbital lesion – Symptoms and signs
There are lesions of various aetiologies that can manifest within the orbit, the most common being benign, vascular or cystic neoplasms in all age groups (14). Malignant neoplasms usually occur in older age-groups, commonly secondarily to perineural metastasis (13).
A lesion within the lateral orbital apex would be located extra-conally. Initially the lesion may produce a localised forward displacement of the fat pads, leading to proptosis, in turn causing an increased inter-palpabral fissure distance.
As this lesion increases in size, the lacrimal, frontal and trochlear nerves would be impinged, leading to a compromised aqueous tear film, anaesthesia of the ipsilateral upper eyelid skin and forehead, and palsy of the SO respectively. Moreover, SO palsy will lead to diplopia, specifically on downward gaze resulting in the individual adopting an ipsilateral head tilt to compensate (15). Ocular and periorbital pain may also be evident due to involvement of the ophthalmic divisions (15). Venous congestion (once the SOV is involved) would follow, and further contribute to proptosis, chemosis and lid oedema (13, 14).
With further progression displacement of the SR and LR would occur. The superior division of CN III would become involved causing palsy of the SR and LPS leading to depression and extortion in primary gaze and associated ptosis. Encroachment of the optic nerve would cause reduced visual acuity, narrowing of the visual field and a relative afferent pupillary defect (RAPD). Involvement of the nasociliary nerve would lead to an absence of the corneal reflex, with associated Horner’s syndrome secondary to compromise of the third-order sympathetic neurons, leading to ipsilateral dysfunction of dilator pupillae and miosis (16). However, anhydrosis may not occur as the trajectory of the sympathetic fibres to the eye is different to that of the sweat glands (16).
If left untreated, the inferior division of CN III and abducens nerve would be affected leading to complete paralysis of all ipsilateral EOMs, pupillary unresponsiveness and blindness. These symptoms are characteristic of orbital apex and SOF syndrome.
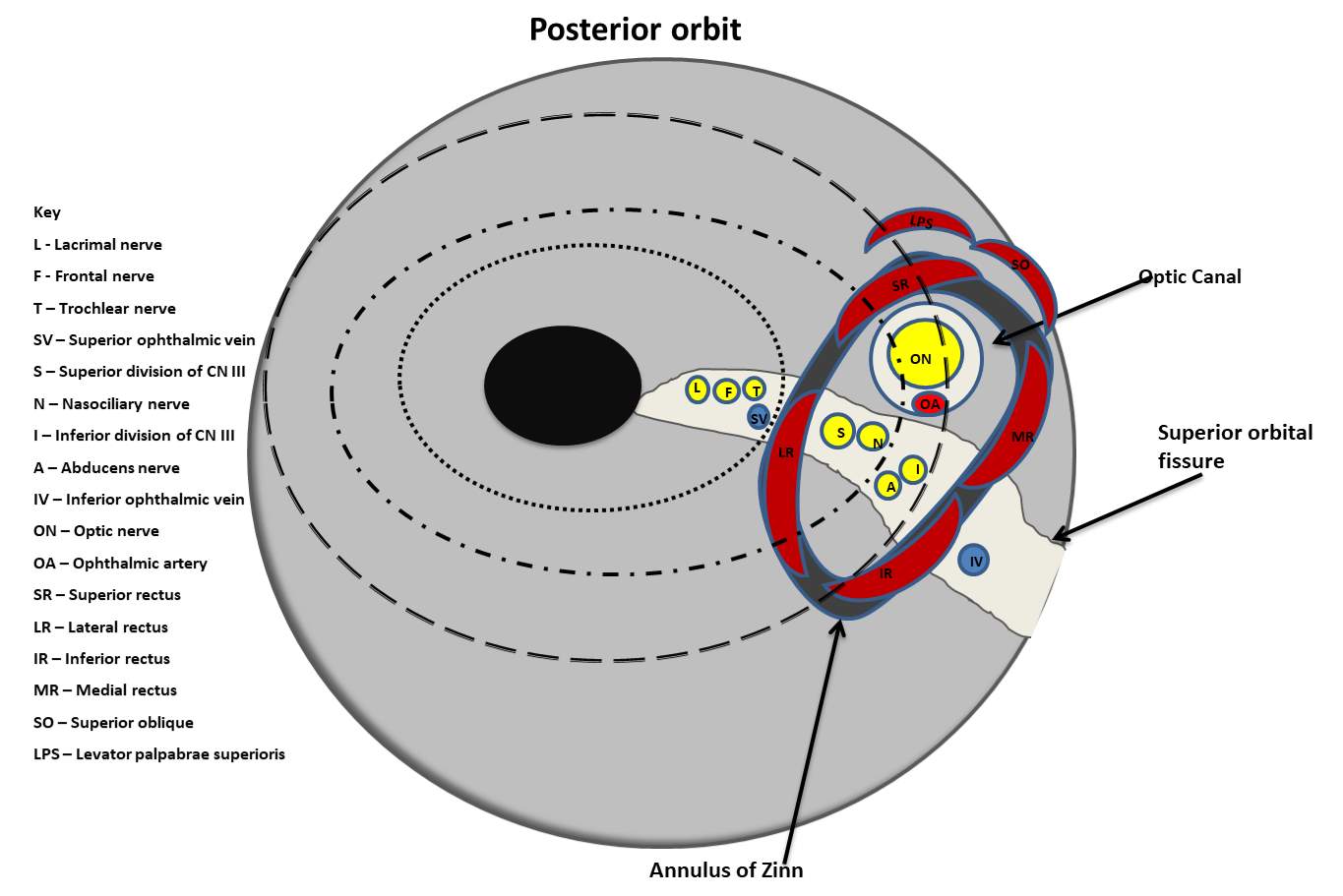
Figure 3. Schematic of the posterior orbit with the postero-lateral orbital lesion at stage 1 (depicted in solid black), and progressive enlargement to stage 2 (dotted outline), stage 3 (dotted and dashed lines) and stage 4 (dashed lines) and subsequent neurovascular involvement involvement.
Management
Lateral orbitotomy can be utilised to excise posterior orbital lesions (17). This involves exposing and removing parts of the lateral orbital wall (formed in part by the frontal, zygomatic and sphenoid bones), thereby allowing access to the lateral orbital apex (4). This technique traditionally involved removal of the entire lateral orbital border and was first described by Kronlein in 1889, however, this has undergone modifications overtime (17, 18). Thus, a modified method to access the lateral posterior wall involves incision of the lateral canthus, separation of the temporalis muscle to adequately expose an area of the frontal process of the zygomatic bone, followed by its removal (19). With this approach however, the sensory zygomatico-facial and temporal nerves (which supplies the cheek and the temple) are compromised (19). Nevertheless, subsequent related co-morbidies have not been reported (19). A recent study describes a modified approach to the orbital apex by lateral canthotomy orbitotomy (20). This allows access to the lateral orbit by creating a rhomboid space by excision of the lateral canthal tendon without bone removal (20). This method may be advantageous over the traditional approach as it is associated with decreased post-operative co-morbidity, better cosmetic outcomes and a lessened risk of dissemination following removal of malignant lesions (20).
Conclusion
In conclusion, the orbit is a pyramidal structure with its apex comprising of the optic canal and superior orbital fissure. These tunnels allow communication of the orbit with the middle cranial fossa, thereby transmitting neurovascular structures through a dense network of connective tissue and fat to innervate the globe. Lesions within the posterior orbit can be of various aetiologies and lead to compromise of the tightly contained structure and integrity of the orbital contents, causing symptoms such as ophthalmoplegia and visual disturbances. Lateral orbitotomy is a treatment option for such posterior orbital lesions.
References
1. Cornelius CP, Mayer P, Ehrenfeld M, Metzger MC. The orbits–anatomical features in view of innovative surgical methods. Facial plastic surgery : FPS. 2014;30(5):487-508.
2. Snell R, Lemp M, Grunther I. Clinical anatomy of the eye. Oxford: Blackwell Science Ltd; 1998.
3. Bron A, Tripathi R, Tripathi B. Wolff’s anatomy of the eye and orbit. Eighth ed. 2-6 Boundary Row, London: Chapman & Hall; 1997.
4. Rene C. Update on orbital anatomy. Eye. 2006;20(10):1119-29.
5. Remington L. Clinical anatomy and physiology of the visual system. Third ed. St. Louis Elsevier/Butterworth-Heinemann; 2012.
6. Hart CK, Theodosopoulos PV, Zimmer LA. Anatomy of the optic canal: a computed tomography study of endoscopic nerve decompression. The Annals of otology, rhinology, and laryngology. 2009;118(12):839-44.
7. Daniels DL, Mark LP, Mafee MF, Massaro B, Hendrix LE, Shaffer KA, et al. Osseous anatomy of the orbital apex. AJNR American journal of neuroradiology. 1995;16(9):1929-35.
8. Reymond J, Kwiatkowski J, Wysocki J. Clinical anatomy of the superior orbital fissure and the orbital apex. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2008;36(6):346-53.
9. Shi X, Han H, Zhao J, Zhou C. Microsurgical anatomy of the superior orbital fissure. Clinical anatomy. 2007;20(4):362-6.
10. Shankland WE. The trigeminal nerve. Part II: the ophthalmic division. Cranio : the journal of craniomandibular practice. 2001;19(1):8-12.
11. Thakker MM, Huang J, Possin DE, Ahmadi AJ, Mudumbai R, Orcutt JC, et al. Human orbital sympathetic nerve pathways. Ophthalmic plastic and reconstructive surgery. 2008;24(5):360-6.
12. Iaconetta G, de Notaris M, Benet A, Rincon J, Cavallo LM, Prats-Galino A, et al. The trochlear nerve: microanatomic and endoscopic study. Neurosurgical review. 2013;36(2):227-37; discussion 37-8.
13. Goyal P, Lee S, Gupta N, Kumar Y, Mangla M, Hooda K, et al. Orbital apex disorders: Imaging findings and management. The neuroradiology journal. 2018;31(2):104-25.
14. Costa RM, Dumitrascu OM, Gordon LK. Orbital myositis: diagnosis and management. Current allergy and asthma reports. 2009;9(4):316-23.
15. Yeh S, Foroozan R. Orbital apex syndrome. Current opinion in ophthalmology. 2004;15(6):490-8.
16. Kong YX, Wright G, Pesudovs K, O’Day J, Wainer Z, Weisinger HS. Horner syndrome. Clinical & experimental optometry. 2007;90(5):336-44.
17. Mariniello G, Maiuri F, de Divitiis E, Bonavolonta G, Tranfa F, Iuliano A, et al. Lateral orbitotomy for removal of sphenoid wing meningiomas invading the orbit. Neurosurgery. 2010;66(6 Suppl Operative):287-92; discussion 92.
18. Lyson T, Sieskiewicz A, Rogowski M, Mariak Z. Endoscopic lateral orbitotomy. Acta neurochirurgica. 2014;156(10):1897-900.
19. Ulutas M, Boyaci S, Akakin A, Kilic T, Aksoy K. Surgical anatomy of the cavernous sinus, superior orbital fissure, and orbital apex via a lateral orbitotomy approach: a cadaveric anatomical study. Acta neurochirurgica. 2016;158(11):2135-48.
20. Hamed-Azzam S, Verity DH, Rose GE. Lateral canthotomy orbitotomy: a rapid approach to the orbit. Eye. 2018;32(2):333-7.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Neurology"
Neurology is the specialist branch of medicine that deals with the treatment of disorders of the nervous system. This means that neurologists concern themselves with issues affecting the brain, the nerves, and the spinal cord.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




