Risk Factors Associated with Oral Cancer in South East Asia
Info: 8176 words (33 pages) Dissertation
Published: 16th Dec 2019
CHAPTER ONE
INTRODUCTION
- Background
- Oral cancer contributes in over 300,000 deaths each year and the World Health Organisation (WHO, 2018) refers oral cancer as one of the major burdens in South Central Asia. Oral cancer in Southeast Asia has managed to overtake the number of the population diagnosed with lung cancer therefore consequently posing as a major threat to the Southeast Asian community (Moustafa,, 2017) .The increasing number of poorly developed countries in Southeast Asia results in an increased presence of the disease. Factors such as limited access of health care services and lack of health awareness contribute to the global burden of oral cancer. The limited knowledge of the cultural risks and knowledge relating to the overall health effects of oral cancer proves to be problematic for healthcare professionals to implement appropriate intervention strategies (Priebe et al., 2008). 70% of Oral cancer cases in Southeast Asia are diagnosed at a later stage thus minimising the survival rate to five years (Shukla & Shukla, 2012). The use of tobacco in Southeast Asia is identified as one of the major and avoidable threats to causing oral cancer with the majority of the poor unable to pay for treatment (SEARO, 2018). The practise of betel nut chewing, consuming smokeless tobacco products, smoking tobacco and alcohol consumption continues to increase the number of oral cancer cases in Southeast Asia (Kumar et al., 2016). This chapter will focus on the background of oral cancer, the history of the preventative measures adopted in South East Asia to lower the number of adults who suffer from oral cancer. The following chapter will address the aim, objective, rationale and research question which will be undertaken in this study.
- Global burden of Oral Cancer
Oral cancer is deemed to be amongst one of the eleventh most common cancers in the world. In 2012, cancers around the mouth were reported to contribute to 3.8% of oral cancer and 3.6% deaths, with 75% of cancers associated with alcohol and tobacco consumption (American Cancer Society, 2016). Over two thirds of the cancer is known to occur in countries with low income, with the vast majority of cases in South Asia (Sankaranarayanan, 2015).Excessive use is defined to individuals who exceed the limit of using a substance which will pose a threat and damage the body (National Institute of Health, 2018), the excessive consumption of alcohol or tobacco have been acknowledged as major risk factors contributing to oral cancer. A poor diet consisting of the lack of nutritional supplies such as fruits and vegetables has proved to cause oral cancer. Therefore, reducing or even preventing the intake of alcohol and tobacco use will significantly reduce the risk of the disease (Gelband, et al. 2015) and the absence of the drug will prevent harm to the body. However, substance misuse is a worldwide issue with over 2 billion consuming alcohol with 76.3 suffering the consequences of damaging health effects and the use of illegal drug use contributes results to a direct threat to the body. Furthermore, addictive behaviour patterns lead to poor oral hygiene, poor nutrition thus strengthening the risk of the disease (Saini, 2013). Evidence suggests that the primary reason of oral cancer in South Asian regions is the habit of betel chewing, smoking and alcohol consumption (Guha et al., 2014). Whilst treatments and clinical diagnoses of cancers have vastly improved over the years, the survival rate of cancers has not been able to cure half of the Southern Asian population over the years (Kumar, et al. 2016). The users of tobacco are three times more likely to develop oral cancer in comparison to non-smokers with passive smoking increasing further risk of the disease. Oral cancer can be presented in the tongue, the floor of the mouth and the upper lip (Rivera, 2015). Most patients with oral cancer detect the cancer at a later stage when the lymph node has occurred (Soully & Porter, 2001), this could be due to factors such as treating the symptoms of the disease with drugs (The Oral Cancer Foundation, 2018) which in retrospect could further harm to the individual and not detecting the symptoms of the disease as harmful. However, preventing treatment of oral cancer has been associated with financial difficulties for individuals to support themselves to cure for the symptoms before the condition becomes worse, the lack of access to health care does not enable to access the treatment and the limited knowledge about oral health care prevents individuals to detect the disease (Jafari et al., 2013) therefore interventions on the proposed risks would prove beneficial in the early detection of the disease (Soully & Porter, 2001).
The rates of deaths caused by oral cancer has reduced in Europe where there is a strong relationship between the cancer and the reduction of alcohol consumption, with an increasing 50% survival rate in five years (Gelband et al., 2015). Whilst in America the rate of survival rate improved by 11% between 1992 and 2006, the survival rates of the cancer in South Asian countries such as India fall below 35% (Gelband, et al. 2015).
Figure 1: Estimated mortality rate of oral cancer worldwide.
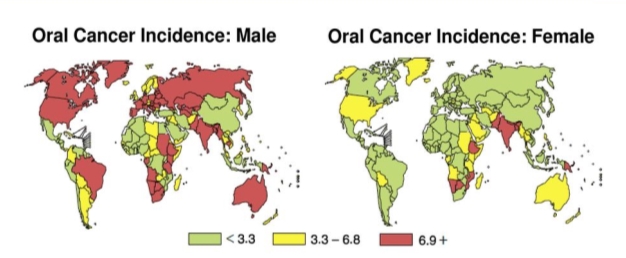
The incidence rate of oral cancer shows a significant gender gap of the incidences between men and women. The rate of incidences and mortality in men are much higher than in women, this is established worldwide as the overall incidence rate of oral cancer of women is 2.7% whereas the women’s incidence is lower at 1.5%. Similarly, this can be acknowledged in Southeast Asia as tobacco consumption is more frequent amongst men, in Mynamar over 50% of the male population smoke tobacco products whereas in the South and Southeast Asia 10% of women in the world’s population consume betel quid (Cheng et al., 2017). However, the South Eastern region is where the mortality and incidence rate of women and men with oral cancer are amongst the highest, Men’s incidence rate is one of the highest at 8.7% and the women’s incidence rate is greatest at 3.6%. Figure 1 displays an indication that men are exposed to an increased number of risk factors which ultimately results in oral cancer, whilst oral cancer is a worldwide problem the table in figure 1 enforces that an increased number of risk factors mainly smoking, smokeless tobacco and consuming betel quid are presented in the South East Region.
- Description of the diseases
WHO (2018) defines oral cancer to primarily occur in the mouth including the lip, oral cavity, nasopharynx and pharynx. When carcinoma arises in the mouth, the early detection could prevent the condition to become worse. Oral cancers could be presented as an ulcer, white lesions, a lump in the tongue and on the lip. Deaths in oral cancer occur when The solution of removing the nodes from the mouth can take place through surgical intervention, which in certain cases lead to death. When the primary malignancy is uncontrolled the individual is likely to die. Many treatments such as reconstructing the tissues and radiotherapy will support patients who suffer from oral cancer (Scully & Porter, 2001). However, the outcome of the survival rate in certain cases will only improve if the individual themselves can reduce the risk factors which cause the cancer. Individuals should take the initiative from health care professionals to understand the risks caused by tobacco, alcohol and diet (The Oral Cancer Foundation, 2018). The cancer is known to develop on the lip or the cavity, which is malignant in nature and it is commonly known as a squamous cell carcinoma due to the origin of 90% of cancers occurring in the squamous cells (Rivera, 2015). The cancer cells are separated from the main site, the cells spread in the tissue and move to the extracellular matrix, disrupting the blood vessels and microvasculature and forcing the fluid through the vessel and multiplying in the recipient’s tissue (Irani, 2016).
Symptoms of oral cancer can be identified from a sore spot around the mouth area, sore spot, a lump in the gums, a white patch on either the gums, tongue or lining, bleeding, changes in the individual’s voice or even signs in teeth loosening (Adult Treatment Editorial Board, 2018). Whilst there are a number of signs and symptoms which will give an indication of the cancer, the main symptom of oral cancer is
identified when mouth ulcers and when a lump in the lymph are not healed (National Health Service, 2016). Primarily the disease is mostly identified at a later stage of the disease, a visual examination provides an accurate description of the definition of the disease towards the individual, a full inspection from the head to neck is required in order to fully understand the extent of the cancer, the tumor, bone invasion or the breakdown of skin. The tumor, nodes and metastases (TNM) is where the patients first examination should be recorded, this is when the biopsy will be conducted a damaged tissue will be taken for examination with the assistance of punch or core needles. Another examination which is crucial for cancer patients is radiographic imaging which will evaluate the lymph node, a computerised tomography (CT) is essential in order to assess the back and neck nodes and to be able to examine the soft tissue a Magnetic resonance imaging (MRI) scan is required (Montero and Patel, 2016). Before acknowledging which treatment should be provided the treatment should be the best fit for the individuals needs, these decisions are made from the department of radiotherapy, oncology, pathology, and radiology. The patients conditions should be treated only when the individuals condition is taken into consideration. Oral cancer patients are provided with four treatment options a surgical treatment, conservative treatment, palliative treatment or dental rehabilitation (Wolff et al., 2012).
1.4 History of oral cancer
The forefront of the second highest deaths in the world is cancer, with numbers up to millions managing to survive with the support of an early diagnosis. Cancer is an ancient disease and the word cancer has been taken from ‘karkinos’, this word defined carcinoma tumors which was discovered in 460-370 B.C. (Sudhakar, 2009) Oral cancer was previously understood to often occur in elderly males (over 60 years), although at present the rate of oral cancer has an increase in females and an increase in the number of young patients (kritika & Omura, 2015).
Oral cancer is a cause of concern worldwide, with the cancer being the sixth common cancer worldwide. In 2008 the incidence rate of new oral cancers was 263, 861 (Monterio., et al 2012)
1.5 Oral cancer in South East Asia
Oral cancer is recognised as one of the more popular non-communicable diseases across the globe, with over 90% of the burden being in South East Asia: India, Pakistan, Afghanistan, Bangladesh, Sri Lanka with other South Asian countries. South East Asia is a country highly affected from the disease reaching the position of being one the most frequent types of cancers being present within the country, this is due to its poor socio-economic conditions, social and cultural habits (Priebe et al., 2016). Whilst research has been conducted on head and neck cancers in Southern Asia, high quality of knowledge-based research has not been conducted because
a number of studies have presented different figures and gaps can be identified in the incidence rates and morality rates between specific time periods which has therefore not provided opportunities on how to control the disease (Khan and Tonniem et al., 2014).
40% of oral cancers in South East Asia is greatly associated with the numerous tobacco products available, with some of the popular tobacco’s being hand-made tobacco, betel nut and chewing tobacco (The Oral Cancer Foundation, 2017). Cultural beliefs may stem from a range of ethnic groups which, therefore could lead to poor oral health, cultural beliefs can lead to the prevention of healthy teeth or individuals placing restrictions on treatment methods (Butani et al., 2008). With a range of differences between individual’s attitudes and cultural beliefs in South Asian countries, the use of tobacco is very common and easy to access (Priebe et al., 2008). In 2012, 11% of the South East population were identified with oral cancer, according to the range of smokers in the South East Population. Smokeless tobacco is identified as a leading trend in South East Asia, therefore questioning the marketing of selling a range of tobacco products which can cause damage to the body and understandably question individuals knowledge about the harms associated with buying tobacco products (Cheong et al., 2017). Tobacco consumption varies in the socioeconomic status of the individual, lack of research and omitted information has proven to be difficult in understanding how to control the overall disease. Oral cancer is 3-7 times more present in poor countries in comparison to rich countries. The health care systems of poor countries like Vietnam is worse due to lack of education, poverty, lack of government funding and policies (Priebe et al, 2008). Due to an increased number of poor population in South East Asia, there is an increased lack of knowledge and education of the threats posed to oral cancer.
1.6 Rationale
Oral cancer is a leading risk factor towards public health worldwide and is amongst the top six cancers (Tanaka & Ishigamori, 2011). The cancer is greatly associated with the link between tobacco and the behavioural factors within the region because of the poor socioeconomic conditions of the Southeast Asian community. In recent years a 60% increase of under 40 years old have suffered from oral cancer with under 50% managing to survive, this figure is evident in Vietnam whereby 30% of 15-20 years old consumed tobacco, with the majority of young men consuming 20% of tobacco, therefore establishing gender differences between the causes of the risk factors (Priebe et al., 2008). However, the lack of progress made from the strategies to control oral cancer does not enable to fully understand the extent of how improvements have been made to control the disease over the years (Tanaka et al., 2011). The main burden of oral diseases compromises of dental caries, gum disease and oral cancer with South East Asia with dental caries being the most common in South East Asia. Even with a number of resources to facilitate the treatment of the disease, the lower class are unable to access the health care system due to poor financial conditions to cure the disease, Impacting on both children and adults (WHO, 2013). When treatment is inaccessible the cancer leads towards tooth decay in children and in adults the teeth are removed. Oral cancer is largely associated with the socioeconomic status of an individual: Late diagnosis of oral cancer, individuals presenting symptoms to the clinic at a later stage due to limited health awareness and lack of financial stability to afford health services is one of the main reasons the diseases has not been fully cured in developing countries (Who, 2013), whereas in rich and more developed countries there has been a decline in the number of oral cancer cases as more care facilities have been provided.
However, when there are opportunities provided for the poor to access treatments, the treatment is poor or illegal which causes further complications (WHO, 2013).
In order to prevent oral cancer, preventive strategies such as enforcing a law on an alcohol ban and restricting certain areas of smoking tobacco in Southeast Asian countries have been put into place. In 2007, The World Health Organisation (WHO, 2007) global health programme evaluated the risks towards oral cancer worldwide. After 25 years of no solution towards oral cancer, a target had been made to prevent the cancer by including oral cancer in the national cancer control programmes, including well educated health care professionals who are experts within the field of oral cancer and can detect and diagnose the cancer at an early stage (Petersen, 2009). However, whilst this strategy was placed there has been minimal improvement in curing the disease. Increasing the educational knowledge of the risk factors amongst the Southeast Asian population regarding the causes of oral cancer would prevent a reduction of the number of oral cancer cases. Almost 50% of oral cancer patients have been noted to reach the final stages of the disease in hospitals and health care centres (Shrivastava et al., 2013). In the worldwide strategies to decrease the incidence of oral cancer, challenges like unqualified health care professionals, poor diagnoses in advanced stages of the disease, lack of funding to use health care services, less effective use of mass-media and difficulty in screening methods have been methods which have been experiences. These are potential barriers which has minimised the scope of public health advantage in reducing the success of government strategic programmes to prevent or reduce the incidence rate of oral cancer (Shrivastava et al., 2013). However, the presence of current strategies of preventing oral cancer such as, early detection, diagnostic process and biological markers of oral cancer, there has been less effective government policies in minimising the disease (Pereira, 2010).
The following chapter will summarise the key risk factors associated with oral cancer in South East Asia. The results will prove beneficial to countries worldwide, in particularly in countries where there is the lack of awareness of the risk factors contributing to oral cancer. A consideration must be made to the socio economic status, cultural beliefs, gender and education towards the rate of oral cancer cases. Once the risk factors of oral cancer are acknowledged, it will help in creating awareness among people in the community and will have an impact in minimizing the epidemic of oral cancer.
1.7 AIM, OBJECTIVES AND RESEARCH QUESTION
1.7.1 AIM AND OBJECTIVES
The aim of the study is to identify and synthesise the factors which are associated with oral cancer in South East Asia. The objective of the study is to critically analyse the appropriate studies providing the contributory factors towards the disease, to summarise the key information from these studies and highlight the risk factors contributing to oral cancer in South East Asia between the period of 2008-2018. The current study is conducted to carry out the objectives which are as follows:
- To evaluate appropriate literatures to recognise if tobacco consumption is associated with an increasing risk of oral cancer cases in Southeast Asian countries.
- To evaluate appropriate literatures to identify if socioeconomic condition and alcohol is strongly linked with the risk of oral cancer in Southeast Asia.
- To review appropriate literatures to identify if gender habits are associated with risk to oral cancer in Southeast Asia.
- To evaluate appropriate literatures to discuss if betel quid chewing is related with an increasing risk of oral cancer in Southeast Asian countries.
1.7.2 RESEARCH QUESTION
The overarching research question of the study was: What are the risk factors contributing to oral cancer in South East Asia?
Conclusion
After providing a brief background and information of the study, a literature review will be discussed in next chapter of the study. The next chapter will propose a detailed outline of the risk factors involved in that have been discussed in the introduction, this chapter will critically reflect on the evidence of the risks and identify the any gaps in the evidence.
CHAPTER TWO- LITERATURE REVIEW
2.1 INTRODUCTION
An in-depth detail of literature review is not only vital in determining the selected topics for research, however it allows the correct application of the research project. Moreover, a reliable and validate literature search is a key principle to evidence-based practice. Absence of good literature review results in a time-consuming process. Research of literature review has been divided into several important steps such as proper selection of research question, choosing suitable sources, searching accurate terms, utilising screening criteria, analysing and evaluating the results. The literature review is completed by researching the information and guidelines from validated data sources like PUBMED, NCBI and google scholar (Poojary & Bagadia, 2014). A prominent change in the in the lifestyle, cultural beliefs, age, gender and dietary system all have a negative outcome in the incidence of the cancer cases (Sankaranarayanan et al., 2014), therefore the study will elaborate on the key risk factors in the below sections: Impact of socio economic status, the use of tobacco, betel quid chewing and oral hygiene.
IMPACT OF SOCIO-ECONOMIC STATUS
A number of environmental and psychosocial factors determine different smoking patterns. Individuals with poor education, unemployment and poverty are identified to be smokers (Castro et al., 2015). The population of Southeast Asia is 1853195 per thousand, oral cancer is amongst one of leading causes for deaths in Southeast Asia with a 6% incidence rate, 5.6% mortality rate and a survival rate of 5.5%. In comparison to more developed countries which contribute to 1.2% of mortality rates less developed countries have a mortality rate of 2.1% (IARC, 2018), therefore providing the conclusion that unstable socioeconomic conditions lead to increasing oral cancer cases. Well marked and defined cultural practices of Asia like betel nut chewing, use of smokeless tobacco, consumption of alcohol are prominent risk factors that make people susceptible to oral cavity cancer: In addition to this, low socio-economic status and poor diet imposes the risk of oral cancer. Alike many other chronic and communicable diseases, oral cancer also manifests a social gradient. Socioeconomic status (SES) can influence the overall health outcomes of an individual and relies upon many factors such as the earned income, the area of housing, level of education, work and status of living. There are numerous factors associated with socioeconomic status, nevertheless in the majority of studies only income is considered in evaluating socioeconomic status (Auluck et al., 2016). Relevant studies such as, Rao et al., 2013; Sankaranarayanan et al., 2014; Cheong et al., 2017; Siakholak et al., 2016 consider the impact of the development of cancer due to the poor socioeconomic condition in Southeast Asia. Rao et al., (2013) states that In Southeast Asia, physical employment like farming, labour and people working in industries are at a higher risk of oral cancer. Tea workers in Sri Lanka and farmers in India are high risk groups in developing oral cancer. The development of oral cancer in from physical employment reiterates that individuals with a lower income are at a disadvantage to developing the disease, this is supported by Priebe et al., (2008) who establishes that education for the poor is limited therefore individuals are unaware about the health risks caused by consuming tobacco products, additionally cultural habits of smoking tobacco products is deeply embedded into the workplace therefore causing further deterioration to their health. Nevertheless, whilst the upper class would be able to afford treatment for the diagnoses, it cannot be assumed that the upper class have the wealth of knowledge regarding the consequences of consumption of drug substances, Warnakulasuriya (2009) identifies how the trends of oral cancer has not changed despite the increase in public education. Studies from Turkey, India and Pakistan reveal the ongoing relationship between oral cancer and education (Siakholak et al., 2016; Rao et al., 2014; Khan et al., 2017), with the poor unable to access educational facilities, people with poor educational backgrounds and unschooled individuals are more exposed towards oral cancer (Rao et al., 2013).
19.80% of the Vietnamese population in Southeast Asia are diagnosed with oral cancer. Vietnam is considered as a financially poor country facing many obstacles. The health care system in Vietnam is challenged due to poverty, limited access to education and insufficient government funding and policies, therefore this does not allow a satisfactory number oral health care professionals to treat the disease Due to the increased number of population in Southeast Asia suffering from poverty, the regular visits to the dentists for general oral examination is uncommon for people in Vietnam( Priebe et al., 2008). Due to inadequate knowledge of the risks caused by tobacco, the use of tobacco to Southeast Asians may not be seen as harmful. In low income countries, oral health awareness is usually unreal regarding the causing factors such as use of tobacco, areca nut chewing, use of alcohol and lack of awareness about health (Goyal & Bhagwati, 2016). There is a strong negative connection of socio economic condition with oral health of an individual. In published report by Columbia university’s earth institute in Vietnam Sunday morning says, that tobacco use and lifestyle of people in developing countries are the main possible risk factors for deaths of thousands of individuals. The burden of oral cancer is associated with use of smokeless tobacco, alcohol, diet and lifestyle. Health care professionals and oncologists in southern Vietnam are worried about awareness of oral health of patients as well as health care workers (Priebe et al., 2012). Health care costs in South East Asia due to oral cancer has been an incredible burden, both towards the cost of medicine to treat patients with oral cancer and costs associated with the use of tobacco. The costs associated with treating tobacco in India 2004, ultimately resulted to an incredibly large sum of 285 million US dollars (WHO, 2018). Oral cancer cases are higher in poor people who are more exposed to smokeless tobacco and alcohol. Studies from south Asian countries like Thailand, India, Indonesia and Bangladesh suggested that consumption of tobacco are higher in less educated and poor people. However, poor socioeconomic conditions does not necessarily mean that individuals will be identified with oral cancer, Khan et al., (2017) states that the product consumption of tobacco, is inexpensive and affordable to the poor and alternative methods of buying and consuming tobacco products are easily accessible. Therefore, one could argue that the risks are not only associated with poor conditions, the risks is highly associated with selling tobacco products which are affordable to the majority.
2. THE ENVIRONMENTAL FACTORS OF CONSUMING TOBACCO:
Worldwide, oral cancer is mainly associated with the usual risk factor of tobacco smoking, in both forms of smoked and smokeless tobacco (Critchley & Unal, 2003). Whilst betel nut chewing can be combined with both smokeless and smoked tobacco it known to be more noticeably used in smokeless tobacco. Smokeless tobacco in South and South East Asia is consumed as one of the major component of betel quid, a combination of elements having arecanut, slakedlime and other components. Betel nut chewing is a major risk factor since it is consumed by more than 600 million population across the globe with the majority of people in Southeast Asia. There is a strong link between consumption of betel quid containing tobacco and oral cancer among the population in this area. In one of the study cases in Cambodia, it is revealed that major possible risk factors of oral cancer is smokeless tobacco where almost 20% of women frequently chewed betel nut, resulting in a possible 6.7% risk of the disease (Cheong et al., 2017).
Smokeless tobacco is one of the important risk factors in developing oral cancer in South East Asia. South east Asia consists of Almost more than 90% of world population in consumption of different forms of tobacco. In India and Pakistan, approximately 100 million people consume smokeless tobacco (Khan et al., 2014). The cases of oral cancer cases are increasingly more in certain parts of India and Southern Asia, in particularly in China and Thailand where the main causal factors of smoking tobacco are with or without areca nut. In the United Kingdom, the burden of oral cancer cases is more in people who are native from South Asian countries, in comparison to the host population. It is estimated that incidence of oral cancer will reach at extreme levels in Europe where larger Asian populations are residing.
Bidis, smokeless tobacco, betel quid and cigarette smoke are a few of the products which are consumed globally (WHO, 2013). Within the Southeast Asian region there are 600 million tobacco users with the majority of smokers, smoking at an early stage, the increase of tobacco smoking is influenced from family, environmental and Individual factors (Sadat et al., 2010).
In a study conducted in Malaysia, tobacco became socially acceptable within young community, the acceptance of tobacco products was observed from the youth observing adults who smoke and consequently deemed smoking to be healthy (Zin et al., 2016). The Global Youth Tobacco Survey reported that 30% of children between 13 to 15 years of age were cigarette smokers and 35.9% of male secondary school pupils were smokers (Swe et al., 2016). Therefore, when an attitude of acceptance is present, there is an unlikelihood of the young realising the damaging consequences of their actions. Factors such as glamorizing tobacco products provides a positive influence of consuming tobacco products (Morrow & Barraclough, 2003). However, the onset of consuming tobacco products at a young age proves to be difficult to discontinue the use of tobacco products (Pradhan & Marahatta, 2016).
Gender patterns are identified to males and females smoking tobacco, with more independence provided to women there has been a rise in the number of women smoking tobacco (Morrow & Barraclough, 2003). Therefore, an increase of tobacco cannot always be determined by poor socioeconomic conditions. Nevertheless, there is a larger proportion of under educated men who consume tobacco (Morrow & Barraclough, 2003). Smoking tobacco and intake of smoking products in Southeast Asia were higher in men in comparison to women, due to the factors such as high age, limited education and poverty (Sreeramareddy et al., 2014). However, there has been a sense to control the disease by advertising the consequences of smoking to both males and females (Morrow & Barraclough, 2003). However, within Southeast Asia smoking and smokeless tobacco was present in women in poor resourced areas However, regardless of the gender roles smoking is commonly associated to both genders, in particularly with those who are undereducated. In sub-region countries such as India, Nepal, Philippines and Cambodia there is a link between men and women smoking and tobacco (Sreeramareddy et al., 2014), therefore cultural influences regarding tobacco use cannot be ignored.
Cultural beliefs imply that smokeless tobacco is less harmful than smoking tobacco (Kyaing et al., 2011). Tobacco in Southeast Asia is used to define the culture between the ‘mainstream’ and ‘minority’, the use of tobacco products is used to celebrate the ethnicity, the cultural practise for the majority would be to use tobacco for social gatherings and consume the product during specific celebrations (Mukherjea et al., 2011). Therefore, cultural practise lead towards leads towards the unacceptance or ignorance towards the harms caused by the product.
Substances such as bidi, hookah and cigarette products are widely available to buy in India (Varshitha, 2015). Therefore, it can be questioned that when tobacco products are easily available and accessible in India, the real risk factors of tobacco is associated with the rules and regulation of drug use and availability of the country. Undoubtedly, in countries such as India, Sri Lanka and Bangladesh laws have been implemented to control the use of tobacco, laws such as restricting the use of smoking in public places, schools and surgeries are already in place, with certain countries such as Bhutan making it a legal requirement to prevent selling and consuming tobacco (The World Bank, 2016). However, irrespective of the implemented laws, the laws are disregarded in certain areas of Southeast Asia where the use of tobacco is continued through cultural influences and poor education.
Limited Access Health care service
The access to health care in Southeast Asia prevents the treatment of oral cancer. Financial issues are in particularly from low-income families which restricts the use of the health care system (The Economist Intelligent Unit, 2017). 72% of the Indian population live in villages and suffer from poverty, around 30 to 40% of the cancers in the rural areas are diagnosed with oral cavity. Due to insufficient knowledge, lack of health care and screening facilities there is an unfortunate outcome of oral cancer cases. Within Southeast Asia India is recognised to have one of the largest oral cancer cases in the world, there is a link between the access to health care services are the geographical region where individuals live. Where 80% of the elderly live in rural areas, the use of smokeless is greater which links to limited knowledge about the health care consequences of using tobacco and the opportunity of finding health care services is a challenge (Dangi et al., 2012).
BETEL QUID
In Southeast Asia, the chewing of betel quid is traditionally practised. Chewing of betel quid is considered to have medical advantages and it is seen as a symbol of social life. In India and Pakistan, one type of quid is named, PAAN. Paan contains areca nut, betel leaf and calcium hydroxide. Betel nut chewing is identified as an important causal factor of oral cancer, with a strong association between oral cancer and betel quid. The ingredient Areca nut being used with Paan is known to be a risk factor of oral cancer due to the presence of substances, which are carcinogenic in nature. In Taiwan, betel quid without tobacco is used while in other South Asian countries like Pakistan, Bangladesh and India betel quid contains tobacco as the main ingredient. However, the burden of oral cancer in Taiwan is higher among men who have built a routine of chewing quid without tobacco and the incidence rate increase amongst individuals who combine tobacco with betel quid. Studies from India and Pakistan also reveals the same. Hence, the combination of tobacco with betel quid increases the risk of oral cancer. Nevertheless, similarly to tobacco the less educated will be unaware of the harmful effects and the individual’s right of autonomy cannot be ignored.
Oral Hygiene
Apart from tobacco and alcohol, poor oral hygiene is one of the factors in developing oral cancer. Insufficient cleaning of teeth may lead to poor oral health. In poor resourced countries, people with low economic status have a worse overall oral health due to lack of awareness and limited education of healthcare (Oji & Chukwuneke, 2012). Countries like India, lack of proper oral hygiene is revealed in around 32% of men and 64% of women. There is a strong association between dental care and oral cancer in India. Dental patients having dentures for more than 15 years and using same denture for many years is one of the major cause of poor oral hygiene. In relation to oral health status survey, it is stratified that 23% of adolescents in India and 12% in china has poor oral health. In Sri lanka, one in five children have poor oral health. Oral health status is an important outcome variable in measuring oral and dental care in southeast Asian countries. Poor oral health may lead to different oral diseases like periodontal disease, gum disease and in later stage it may have risk of oral cancer. With respect to promote oral health and proper oral hygiene, it is mandatory to understand oral health practices in south Asian countries (Peltzer et al., 2016).
ALCOHOL CONSUMPTION
Similarly, to tobacco alcohol is known to be one major risk factors of oral cancer and has been a noticeable problem for over 50 years. The increase of excessive alcohol consumption has raised concerns over the number of oral cancer rates (Ogden, 2005). Substances found in alcohol create damaging effects, when addictive behaviours patterns are identified as the second leading cause of oral cancer and there are difficulties in identifying those diagnosed with only alcohol as most will consume tobacco products (The Oral Cancer Foundation, 2018). However, in a case control study by Goldstein et al., (2010) found that alcohol is significantly associated to oral cancer case even in the presence of tobacco. In Southeast Asia alcohol was accountable for 4.6 deaths (WHO, 2017), the consumption of alcohol is associated to gender and poor socioeconomic conditions. The World Health Organisation (2017) establishes that alcohol is posed to a threat mostly to men, due to factors such low socioeconomic status and poor educational results. This is evident in Thailand, whereby 15 to 32% of alcohol related problems were identified (Nanakorn et al., 2001). Therefore, it can be acknowledged that both tobacco and alcohol are at a greater extent consumed by the poor, with significance in the socioeconomic conditions. In Southeast Asian countries alcohol consumption is greater amongst the poor, who are affected the most. With the poor spending a majority of their income on alcohol, for example in Sri Lanka 30-50% of low income families would spend their income on either tobacco or alcohol. In southeast Asian countries alcohol is a primary problem for women who are left with ill partners who are unable to afford treatment (Assunta, 2001). Therefore, it can be acknowledged that alcohol, socioeconomic status, tobacco and gender factors all contribute to the risk of developing oral cancer.
Conclusion
Oral cancer contributes to the ill health of individuals across the globe. The impact of the socioeconomic status, the environmental factors of tobacco, oral hygiene and alcohol are all risk factors contributing to oral cancer. Poorly developed countries in the Southeast Asian region are challenged with a majority consuming alcohol and tobacco products. However, the mass production of alcohol, betel quid, tobacco and smokeless tobacco at affordable rates continues to be evident. Therefore, a number of potential strategies are available which the government can develop to prevent the disease. The study will now systematically review the risk factors of oral cancer in Southeast Asia and the methodology will be discussed in the next chapter.
CHAPTER THREE- METHODOLOGY
3.1 INTRODUCTION
The research will be conducted using a systematic review. This chapter will provide justification of conducting the research using a systematic approach including the specific research question, ‘What are the risk factors of oral cancer in Southeast Asia?.’. The methodology will outline how ‘The Cochrane system’ involving statistics, figures and research linked to tobacco will be completed by using the PICO tool, where relevant opportunities for research can be accessed, how quality data can be accessed and evaluated. The methodology aims to address the ethical principles of conducting the research. This chapter will be divided into nine sections to discuss the systematic approach.
Research design
A purposeful research design allows access to reliable and relevant data. From the research question, aims and data sources the most suited data research can be accessed and evaluated (Pereyra, 2012). Systematic reviews is identified as one of the most purposeful research systems. Whilst there are many research design options available, systematic reviews eliminate selection bias. A systematic review will consist of a thorough and informative plan and actions to search strategies which is in effect how this study will be completed. A systematic review will focus on the link between two compatible variables. The scale of the study is dependent on the sample size, the intervention and the outcome of the study. A population, intervention, comparison and outcome (PICO) tool proves beneficial and can be useful to ensure that the key aspects are covered before the review is conducted (Lindsay & Usman, 2011).
A systematic review is established on fair grounds proving to provide the more thorough evidence. In comparison, another design ‘narrative review’ is biased and there is a likelihood that the authors will preselect the research. Narrative reviews are less thorough in terms pf approaching the review process. A systematic review will report on the methodology, the terms to search and the inclusion and exclusion criteria (Jahan et al., 2016). Systematics reviews use specific methods of extraction and synthesises the studies with the quality of the study being assessed. Systematic reviews are reliable, unbiased and an alternative solution can be found to resolve conflicting findings (Cochrane Public Health, 2015) .
Accurate and reliable research can be sought systematically, with a clear emphasis on the quality of the literature search. A literature search is valuable in answering the research question and a systematic approach will only focus on specific information. A systematic approach is manageable when the process is accurately followed (Grewal et al., 2016). A systematic review will narrow studies down, proving useful to reduce the number of studies selected (Smith et al., 2011), therefore enabling to provide a quality assessment of the results. Systematic reviews is not opposed to including meta analysis, however where systematic reviews are conducted, meta-analysis is used to draw out statistical data from a number of specific studies, which creates additional robust evidence than choosing data from one study (Northcentral University, 2018). Therefore, systematic reviews provide a well-structured process so that the evidence found in the studies can provide a conclusion of the cause of the disease (MacGill, 2016).
Rationale for systematic review
The present research was conducted to search for accurate and valid information including the key factors contributing to oral cancer, with countries within Southeast Asia. Thus, the approach of using a systematic approach for the study design can be identified as one of the most preferred methods to conduct the study. Systematic Reviews support clinical decisions, once the problem or personal situation has been identified there is more scope for alternative decisions. A number of studies are considered to search for a specific research question. Systematic reviews provide the indication if scientific findings can be Systematic reviews provide the indication if there is reliability of the research by accounting for factors such as the population, type of settings and if there are similarities within subgroups (Garg et al., 2008). A systematic approach is seemingly the best-fit approach to investigate and determine the global outlook of the risk factors contributing to oral cancer (Haidich, 2010). Furthermore, systematic review was chosen on the grounds that data is easily accessible, in comparison to other research designs using a systematic approach is inexpensive, uses time effectively and there are more opportunities to access data for both the population involved and the subgroups within the population.
Searching strategy
Numerous data sources to search the risk factors for oral cancer has been collected from relevant data sources such as PubMed, NCBI, World Bank, Google Scholar and The World Health Organisation. These databases will provide validated information for the study. Additionally, for further material e-journals have been accessed from the University of Bedfordshire. The key terms searched to access the literature review Include ‘oral cancer’, ‘tobacco’, ‘risk factor’, ‘Southeast Asia’, ‘beetle nut chewing’, ‘India’, ‘Vietnam’, ‘Pakistan’, ‘alcohol’ ‘socio-economic status’, ‘compare’ and ‘smoking’. The reference list from the searched materials were accessed and utilised to strengthen the reliability of the results. Furthermore, the Boolean operators ‘And’, ‘Or’ and ‘NOT’ were used to access relevant data and the search engine has been used to find additional data.
Inclusion and exclusion criteria
To concise the findings for the results the inclusion and exclusion criteria is developed. Before commencing onto the findings for the literature the points sated in the criteria list reduces bias. To avoid confusion and access to poor quality data, the criteria was set before the study commenced (McDonagh et al., 2010) The Cochrane system including statistics, figures and research linked to tobacco will be completed by using the PICO tool, this will provide an outline of the population, intervention and outcomes of tobacco and drug use in Southeast Asia. The PICO tool is useful in this study to focus on the systematic evidence to eliminate unnecessary research materials and focus on specific interventions (Methley et al., 2014).
Below is the outline for PICOS tool for this study:
P- Population- population who suffer from oral cancer and rate of oral cancer cases. I-Intervention- acknowledging the programmes and media contribution to prevent the use of drug related products in order to reduce the rate of oral cancer.
C- Comparator- risk factors amongst males and females of oral cancer in Southeast Asia and the
O-Outcome- main risk factor of oral cancer.
Study design-a systematic review outlining an exclusion and inclusion criteria.
The following table explores the study design and outlines the restrictions which have set in the study.
Table 1: Table outlining the inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Cancer"
Cancer is a disease in which cells grow or reproduce abnormally or uncontrollably. Cancerous cells have the potential to spread to other areas of the body in a process called metastasis.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




