Calcium as a Means of Reducing Risk of Low Bone Mass
Info: 11872 words (47 pages) Dissertation
Published: 9th Dec 2019
Introduction;
Calcium is a mineral. The body has more calcium than any other mineral. About 99 percent of calcium in the body is stored in the teeth and bones, this nutrient is also present in the blood, the fluid in the body cells and muscles (Pu et al., 2016) . In addition, it has been established that calcium is a known mineral, however calcium is also an essential nutrients that is important for several functions in the body and it helps make strong bones and teeth (Beto, 2015). “Calcium is one of the most important nutrient in the body because without this nutrient death is paramount and this is why calcium is an essential nutrient. Calcium can be found in some certain foods and it is abundantly available in dietary supplements and these supplements include such as calcium magnesium supplements (Zhao et al., 2017).
FIG 1.2 Diagram of the biological composition of Calcium ion from (Rajagopal and Ponnusamy, 2017).
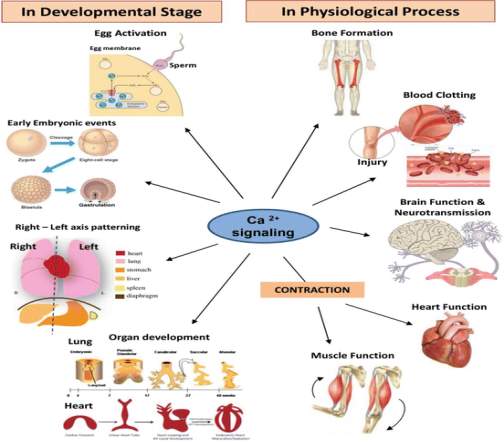
ROLES OF CALCIUM IN THE BODY.
Calcium plays a role in;
- Blood clotting
- Bone and teeth strengthening
- Regulating Heart Functioning
- Muscle functioning regulation, e.g. contraction and relaxation of muscles.
- Enzymatic functioning
- Transference of messages to nervous system. (Ismail, A., Ismail, N. A., 2016)
CALCIUM REGULATING HORMONES.
Parathyroid hormone: The parathyroid gland releases the parathyroid hormone which is divided into four and can be seen at the back of the thyroid gland in the neck (Akgül et al., 2017). PHT works on the bone and causes resorption of bone. This process triggers the release of bone calcium which then increases the plasma calcium concentrations (Lourida et al., 2015).
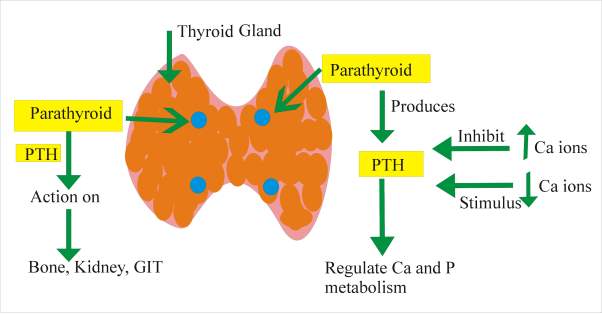
FIG 1.3 shows the regulation of plasma calcium concentrations with the action of both PTH and Calcitriol.
Calcitriol Hormone:
This is a hormone derived from vitamin D (Cholecalciferol). However, it is produced by the skin through ultraviolet light on 7-dehydrocholesterol. It stimulates increased calcium absorption from the GIT. This hormone triggers the release of calcium from by acting on osteoclasts found in the bone (Newman et al., 2016).
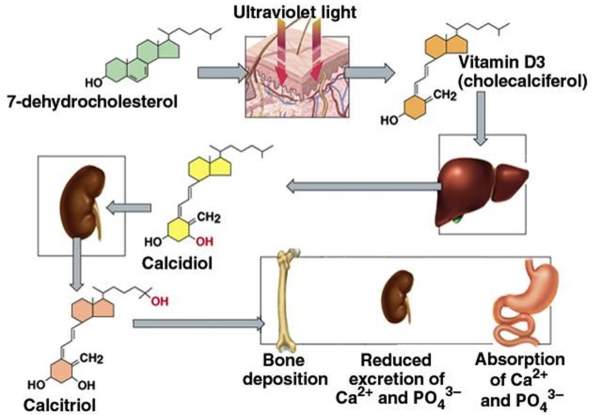
FIG 1.4 shows the production of Calcitriol.
THE IMPACT OF CALCIUM ON PATHOLOGICAL PROCESSES.
Calcium is an important component of the skeleton, and this skeleton produces a large volume of calcium for other important calcium-dependent functions in the body. There are three main functions the skeleton is responsible for. Firstly, calcium one of the mineral hydroxyapatite that is placed into the skeletons organic matrix and it is also important for the structure which is important for rigidity, elasticity, and strength of the tissue. However, all these help the normal body movement and exercise.
Calcium’s role in blood clotting: Calcium is essential in blood clotting and this nutrient is present in the clotting cascade through which insoluble prothrombin is converted into thrombin in blood clot by the action of fibrin and other clotting factors (Lean and Combet, 2016).
Calcium in bone and teeth strengthening: Strong teeth and bones are essential for all round health. Although, an important factor in maintaining healthy bones and teeth depend solely on calcium. However, Calcium can be described as a mineral that is one of the most abundant in the human body (Zhang, J. et al., 2001). This nutrient calcium can also be found in a number of foods and it can also be artificially added to some others. Amongst other factors, Calcium is known to be added to vitamins and some dietary supplements because it is an important mineral that is needed by the body (Zhao et al., 2017). Moreover, a number of the calcium found in the human body is stored in the teeth and bones. In addition, for the strengthening of the teeth and bones, calcium is also essential for the body’s blood vessels, fluids and muscles.
Muscle functioning regulation, e.g. contraction and relaxation of muscles; Calcium causes contraction by reacting with regulatory proteins in the absence of calcium which prevents actin and myosin interactions (Hessel et al., 2017). There are two different regulatory systems found in different muscles (Gong et al., 2005) For example, in actin-linked regulation troponin and tropomyosin they regulate actin by blocking sites on actin which is required for complex formation with myosin; in are blocked in the absence of calcium myosin-linked regulation sites on myosin are blocked. (Kuo and Ehrlich, 2015; Szent-Györgyi, 1975)
Enzymatic functioning; central to many of the most important cellular processes is Calcium signaling, from intracellular transport to memory (Ahvazi et al., 2003; Robinson, 2010). More often, calcium starts by joining up with an intermediary protein, calmodulin. With calcium involved, calmodulin (now called Ca2+/CaM) then it binds to a large number of cellular targets, disrupting their structure and their function ((Ahvazi et al., 2003; Robinson, 2010)
Transference of messages to nervous system;
The calcium communication signals between cells operates between neurons where these signals intimately integrate with chemical and electronic signal communication at the synapses (Suadicani et al., 2010). Most recently, glial cells have been seen to also exchange calcium signals between each other in brain slices and cultures. According to (Braet et al., 2004) states that, cells that are not considered as brain cells in general become incorporated progressively, as astrocytic calcium signals are said to be communicated to endothelial cells of the vessel wall which can affect smooth muscle cell tone to influence the vessel diameter and thereby resulting in blood flow. (Braet et al., 2004; Ruat and Traiffort, 2013)
The most important physiological function of calcium aside from the role it plays in maintaining the strength of the skeleton, the intracellular messenger in cells and tissues throughout the body is dependent on effectiveness of calcium (Pohlkamp et al., 2017).
OSTEOPOROSIS
Low bone mass which results in increased fracture risk and structural deterioration is caused by a condition known as Osteoporosis. It further leads to porous bone, which is related with higher fracture risk (Lorentzon and Cummings, 2015). However, declining of estrogen levels caused by Bone loss is related with increased fracture risk in postmenopausal women, who produce the majority of osteoporosis cases. Moreover, diagnosis and screening utilize bone mineral density (BMD) measurement which analysis bone strength (Kling et al., 2014)
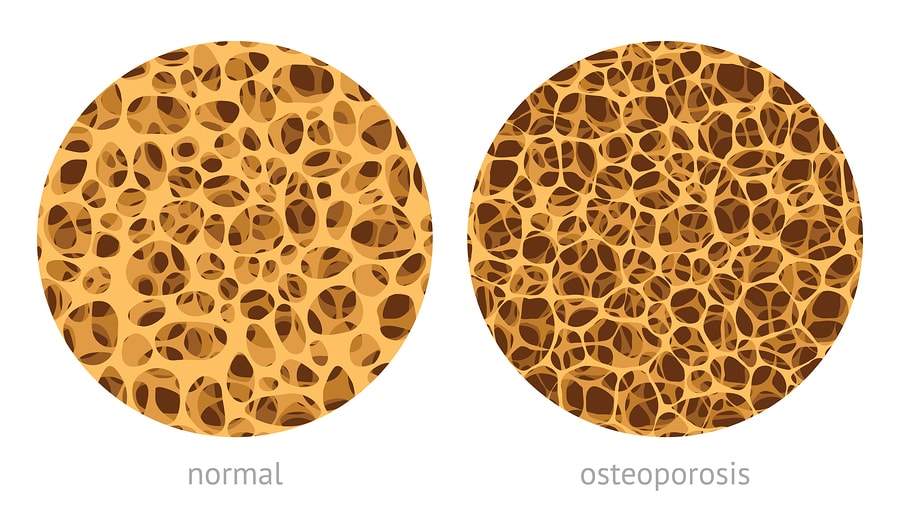
Fig 1.5: The diagram above shows a normal bone and a diseased bone. (Zoch et al., 2016)
Osteoporosis is a disease caused by fragile and thin bones which can easily break. People with the condition osteoporosis, it is normally associated with low bone mass that can lead to fractures of the bone. Although, having sufficient levels of calcium intake in the diet can help prevent osteoporosis and loss of bone mass (Higgs et al., 2017). Osteoporosis is a disorder that is very common, and it often results in an increase in fracture risk. Statistics show that the annual cost delegated to vertebral, hip and wrist fractures in England and Wales is approximately £1.7 billion (Hernlund et al., 2013). However, as a result of this fractures caused by osteoporosis, mortality and morbidity rate have significantly increased over time (Teng et al., 2008). Over 55% of women and 22% of men over the age of 50 years will be affected by fractures caused by osteoporosis in their life (Nazrun et al., 2014) The common A method called dual energy x-ray absorptiometry is a frequently used method for diagnosing osteoporosis (Blake & Fogelman, 2007; Sheu and Diamond, 2016). Nevertheless, the aim of preventing and treating osteoporosis is to stop the future fractures from occurring again. Also, changes in lifestyle should be advised for patients that are of high risk of developing this disease (Vestergaard, 2006). In addition, Pharmacological treatments which entails the bisphosphonates, hormone replacement therapy, calcium and vitamin D supplements, oestrogen selective receptor modulators, calcitonin, the fragment 1-34 of calcitriol and parathyroid hormone.
How Osteoporosis develops.
Bones are derived from proteins which are collagen and non-collagen, and they are strengthened with calcium. Peradventure an individual does receive sufficient calcium from their diet, the body then removes calcium from the bones, which results in loss of bone mass and strength (Veldurthy et al., 2016). As a result of this, the person is likely to develop thin and fragile bones with osteoporosis. However, developing and maintaining calcium bone density differs throughout a person’s life. In some cases, calcium is more important in bone growth during teenage years and rapid bone loss is more significant after age 50 years (Levine, 2012). Therefore, to reduce the risk of osteoporosis, calcium intake should be the highest during adolescence and after 50 years of age.
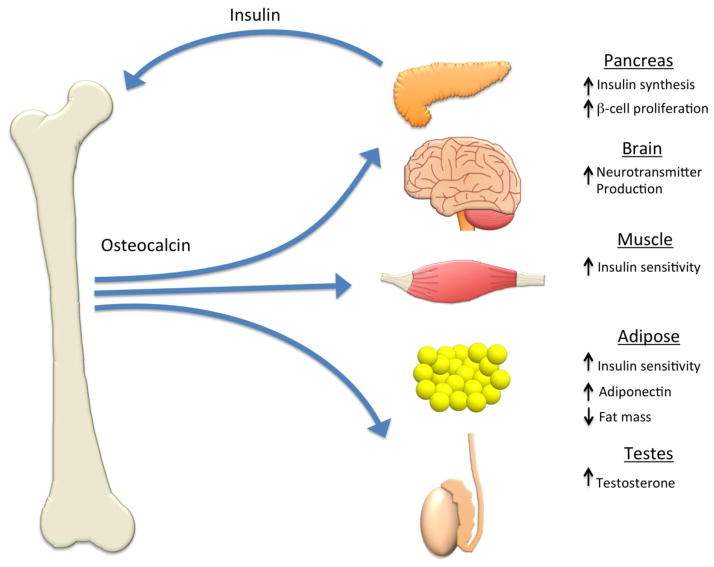
Fig 1.6: This diagram shows the bone protein osteocalcin.
A protein hormone called osteocalcin is produced by osteoblasts, the cells that create bone tissue.
It is part of the materials in your body’s bones. It tends to attach itself to calcium in the bones and it’s also involved in the regeneration and formation of the bones.
FOOD SOURCES THAT CONTAIN CALCIUM
- Cheese
- Salmon
- Beans
- Yogurt Etc.
The causes of osteoporosis.
Mineral bone density
It has been revealed that the lower the BMD the higher the fracture risk. A number of sites including the lumbar spine can be assessed for bone mass function e.g. the forearm, the hit, and other sites. Dual energy x-ray absorptiometry (DXA) at the hip and the spine is the most commonly used technique (Sheu and Diamond, 2016).
Body weight
Several studies have revealed that there is a negative relationship between low body mass index and peak bone mass. However, low body mass and weight loss have a relationship with increased fracture risk.
Nutrition
In several studies and a relationship between calcium intake and bone mass which appeared in premenopausal women. On the other hand, the association between calcium intake and fracture rate is not certain in these women (Burckhardt, 2015).
Sex hormone deficiency
Low bone density is related to Primary hypogonadism in both sexes. ‘’In women with secondary amenorrhoea the peak bone mass reduces and the chances of osteoporosis is increased’’. Late menarche reduces high bone mass. However, premature menopause in women before the age of 45, results in a likelihood of bone loss and increased risk of fracture among women. (Christodoulou & Cooper, 2003)
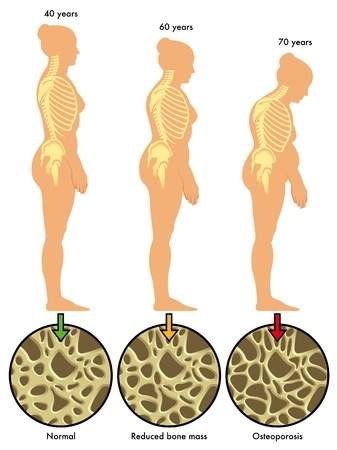
Fig 1.7: The diagram above shows the effect of low bone mass on women as they age.
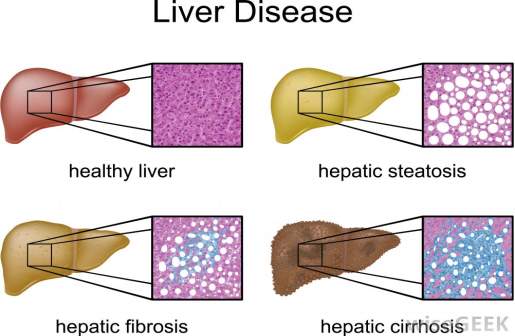
VITAMIN D AND LIVER DISEASE.
25-hydroxy (25-OH) vitamin D is produced by the liver, which is also known as calcidiol, the second precursor to the metabolically active 1, 25 dihydroxyvitamin D 1-25 vitamin D. The most abundant circulating form of vitamin D is 25-OH vitamin D, and this is a technique to measure vitamin D deficiency (Bikle, 2009). However, with liver failure patients, the levels of 25-OH vitamin D is relatively low due to impaired synthesis. However, in order for this impairment to occur liver function needs to be severely compromised (Konstantakis et al., 2016). The impaired absorption of vitamin D can also be caused by liver disease, which is related with impaired bile acid production and gut edema portal hypertension (Iruzubieta et al., 2014; Yang, C. H. et al., 2017).
Moreover, bone disease with low vitamin D levels are known to be associated with complications of “cholestatic” liver disease, which reduces the flow or production of bile. Recent studies have also revealed low vitamin D levels in non- cholestatic liver disease (Nair, S., 2010; Reshetnyak, 2015).
Fig 1.8: This diagram shows the effect of low bone mass on the liver.

Fig 1.9: This diagram below illustrates how low bone mass can damage the liver.
How Much Calcium Is Needed?
Although the calcium in the body changes with age, the amount of calcium taken calcium should monitored and regulated. Based on age, the intake of calcium is normally between 1,000 and 1,300 milligrams (mg) per day. The person’s gender and age is a factor that determines the dose of calcium required (Sunyecz, 2008).
Table 1.1 Calcium Reference Range.
| Age (years) | Calcium (mg/day) | Vitamin D (IU/day) |
| 4–8 | 800 | 200 |
| 9–13 | 1300 | 200 |
| 14–18 | 1300 | 200 |
| 19–30 | 1000 | 200 |
| 31–50 | 1000 | 200 |
| 51–70 | 1200 | 400 |
| ≥70 | 1200 | 600 |
In the body, only about 500-600 mg of calcium the intestine can absorb at a time, which means the total calcium intake would be divided over the course of a day (Bronner, 2003). Absorbing too much calcium can lead to the formation of kidney stones (Sorensen, 2014). However, high intake of calcium may be associated with some health risks, for example, strokes and heart attacks. Nonetheless, scientific studies have not be conclusive (Body et al., 2012). Although, having enough calcium in the body is important, too much could result in major health issues (Chin et al., 2017).
Foods containing high calcium can help meet the daily dietary requirement. Dairy products are the best sources of calcium due to their high elemental calcium content, high absorptive rate, and relative low cost. Most dietary foods containing calcium includes cheese, milk, yogurt) also green vegetables such as spinach etc. Each day approximately 300 milligrams of dairy serving is consumed (Bauer, D. C., 2013) . One cup (8 ounces) of yogurt, one cup of milk or one to 1.5 ounces of cheese equals a dairy serving size. Therefore, an approximate total elemental calcium consumption can be provided by multiplying each daily serving by 300mg (Sunyecz, 2008).
Therefore, for adequate calcium intake to be assured, some of calcium supplements are readily available. There are two widely used and common calcium supplements which are calcium citrate and calcium carbonate. However, when these two supplements are taken with food they equally become well absorbed (Lamy & Burckhardt, 2014). In the time past, gastric acid secretion and gastric acidity have been said to play a vital role in the intestinal calcium absorption (Kopic and Geibel, 2013). Based on randomized crossover trial it has been revealed that the proton pump inhibitor, omeprazole, distinctively reduced fractional calcium absorption from calcium carbonate when elderly women ingest it after fasting overnight without eating (Yu, E. W. et al., 2011). However, it was revealed by a case control study that long-term proton pump inhibitor therapy in particular when at high doses, was linked with an increased risk of hip fracture (Wang, L. et al., 2017; Yang, Y.-X. et al., 2006). According to research which also supports that calcium absorption can be certain by taking it with food (Pereira et al., 2009). Moreover, normal calcium carbonate supplements absorption have been reported to improve when ingested with a meal, even with patients who are achlorhydric (Cavalcoli et al., 2017). According to a study which assessed the role of gastric acid on calcium absorption revealed that a large dose of cimetidine, that reduced gastric acid secretion, had no significant effect on calcium absorption from citrate or carbonate sources (Kopic and Geibel, 2013). In addition, calcium carbonate absorption did not change even though gastric contents were maintained at a pH of 7.4 or 3.0 (Sunyecz, 2008; Yang, Y.-X., 2012).
Treatment
- Only about 14% of patients who consume continuous oral glucocorticoids receive treatment to prevent bone loss.
- Only adults who will receive glucocorticoids at doses of 7.5 mg/day or more for six months or more should be considered for treatment.
- The most commonly used therapies in the UK are the bisphosphonates and HRT. (Christodoulou & Cooper, 2003)
DURATION OF HEALING AFTER NUTRIENT HAS BEEN ADMINISTERED.
- Osteoporosis does not inhibit the healing processes. Although, when a fracture occurs, it usually heals between six to twelve weeks. However, in any broken bone, it sometimes takes longer. (Fischer et al., 2017; Pesce et al., 2009)
THE ROLE OF VITAMIN D.
Vitamin D is a steroid hormone that is vital for the absorption of calcium and bone mineralization which is related with bone mineral density [BMD] (Veldurthy et al., 2016). It has been established that severe and prolonged vitamin D deficiency leads to osteomalacia in adults and ricket in children. Suboptimal vitamin D status has been revealed in many populations but has become a major concern in elderly people; thus there is a clear need for effective ways to optimise bone health (Uday and Högler, 2017). Moreover, recent studies have suggested that the vitamin D role in preventing fractures may be through its mediating effects on muscle function e.g. a defect in muscle function is one of the signs of inflammation and ricket (Laird et al., 2010; Nair, R. and Maseeh, 2012). Studies have also shown that vitamin D supplementation can positively change muscle strength. Osteoporosis is often considered to be an inflammatory condition and pro-inflammatory which is one of the largest contributors to fracture incidences (Ferrucci et al., 2014).
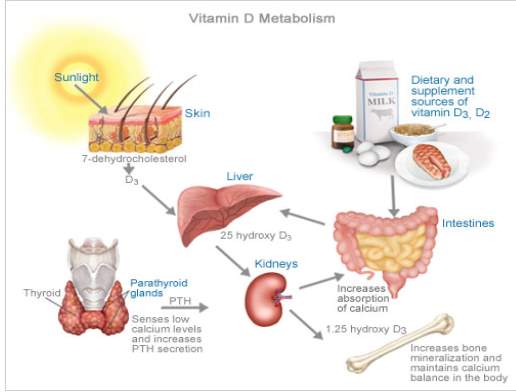
FIG 2.0 SYNTHESIS OF CALCITRIOL FOLLOWING ACTION OF SUNLIGHT ON 7-DEHYDROCHOLESTEROL IN THE SKIN.
Cytokines have been seen to be closely related with high bone metabolism. The immune-regulatory mechanisms of vitamin D may increase the effect of these cytokines on bone health and increase fracture risk. Vitamin D can influence fracture risk through different mechanisms (Gröber and Kisters, 2012).
- Drug interactions
Calcium supplements have the tendencies to interact with many prescription and over the counter medications. Calcium supplements may reduce levels of the drug digoxin. The drug interaction between vitamin D supplements with calcium and digoxin may also increase the risk of hypercalcemia. Calcium supplements also interact with different antibiotics such as; levothyroxine, fluoroquinolones antibiotics which are in the tetracycline family. Overall, when two of these drugs mentioned above are taken together and at the same time, the intake of any calcium supplement reduces the absorption of these antibiotic drugs (Jellin et al 2000; Shannon et al 2000).
- Food Interaction.
Foods containing high amounts of oxalate and phytate reduces the absorption of calcium contained in these foods. For example, Spinach, rhubarb and beet greens are foods high in oxalate. Although, these foods may be good for a healthy diet, they are not effective sources of calcium nutrients (Han, H. et al., 2015).
CALCIUM HOMEOSTASIS.
1. CALCIUM DEFICIENCY CAN LEAD TO.
- calcium deficiency disease (hypocalcaemia)
- Poor calcium intake over a long period of time particularly during childhood
- medications that may reduce calcium absorption due to drug interactions
- Dietary intolerance due to high calcium foods.
- Hormonal changes particularly in women can lead to calcium deficiency.
2. Hypoparathyroidism is a hormonal disorder that may lead to calcium deficiency disease. Individuals with this condition do not produce sufficient parathyroid hormone that is known to controls calcium levels in the blood.
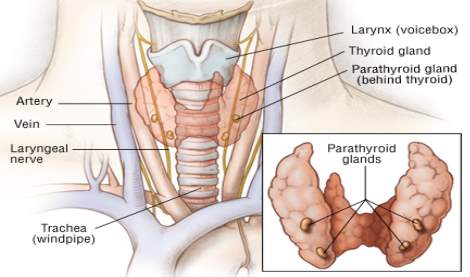
Fig 2.1: Shows the diagram for hypo-parathyroid hormonal disorder.
3. Paget’s disease: Paget’s disease of bone affects the body’s recycling processes, This occurs when new bone tissue replaces old bone tissue gradually (Alonso et al., 2017). If disease is prolonged, it will start affecting the bones and lead to bones becoming fragile and misshapen. Paget’s disease of bone occurs commonly in the pelvis, skull, spine and legs (Paul Tuck et al., 2017).
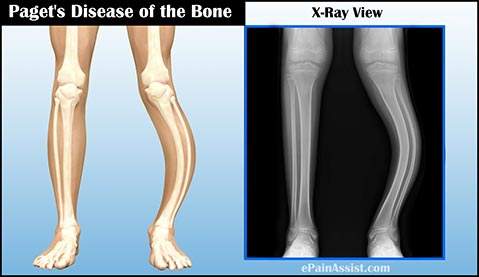
Fig 2.2: The diagram above shows the effects of Paget’s disease on the bone.
4. Hungry bone syndrome: This is a faster and more prolonged hypocalcaemia which is related with hypophosphatemia and hypomagnesaemia. This is aggravated by parathyroid hormone (PTH) levels that is suppressed, it also follows with para-thyroidectomy in patients with severe preoperative high bone turnover and primary hyperparathyroidism (PHPT) (Witteveen et al., 2013)
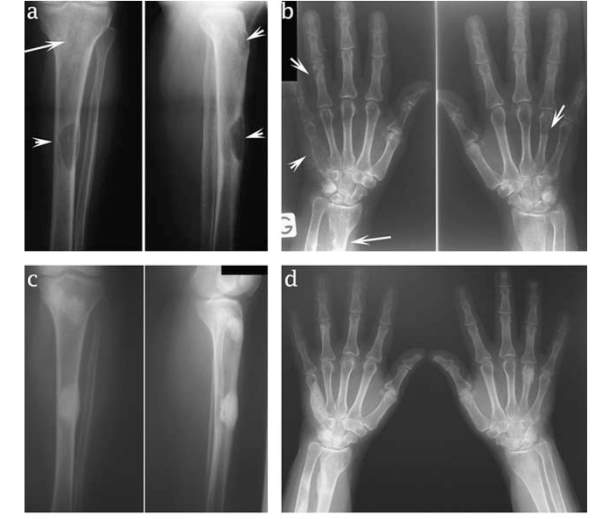
Fig 2.3: This diagram shows the hungry bone syndrome caused by low bone mass.
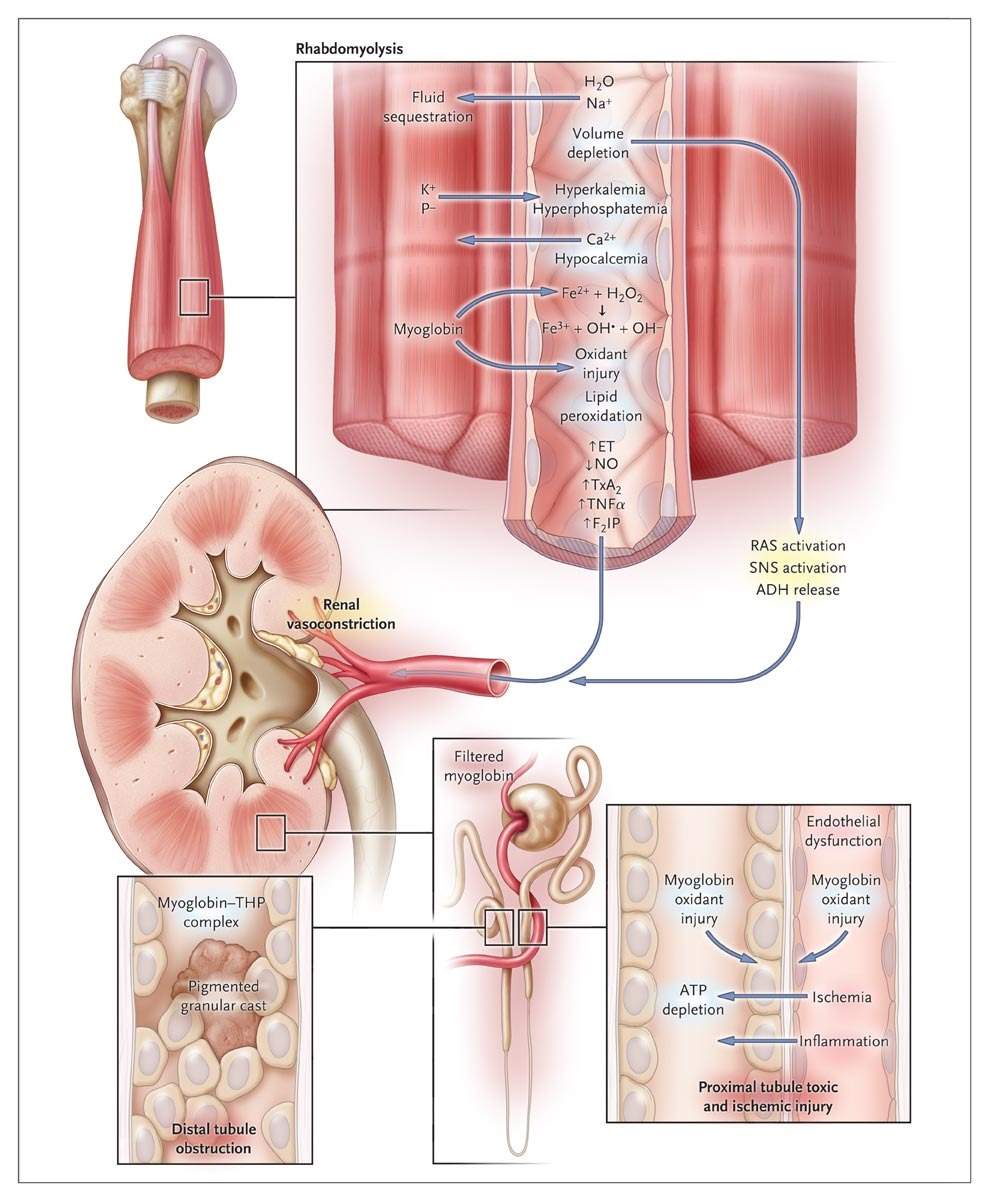
5. Rhabdomyolysis: a severe syndrome caused by a direct or indirect muscle injury. The death of muscle fibres and release of their contents into the bloodstream is the major cause leading to this disease (Bosch et al., 2009). Renal (kidney) failure is one of the complications of this disease. This is when the kidneys is not able to remove waste and concentrated urine (Torres et al., 2015)
Fig 2.4: This diagram an illustration of the Rhabdomyolysis disease mentioned above.
In conclusion, Calcium deficiency is often easy to treat and can be improved by adding more calcium to diet.
Age at Onset of Puberty Predicts Bone Mass in Young Adulthood
Conclusions of study
In adolescent females and males who were healthy, the bone mass and density of bone at skeletal maturity are related to puberty timing. (Gilsanz et al., 2011)
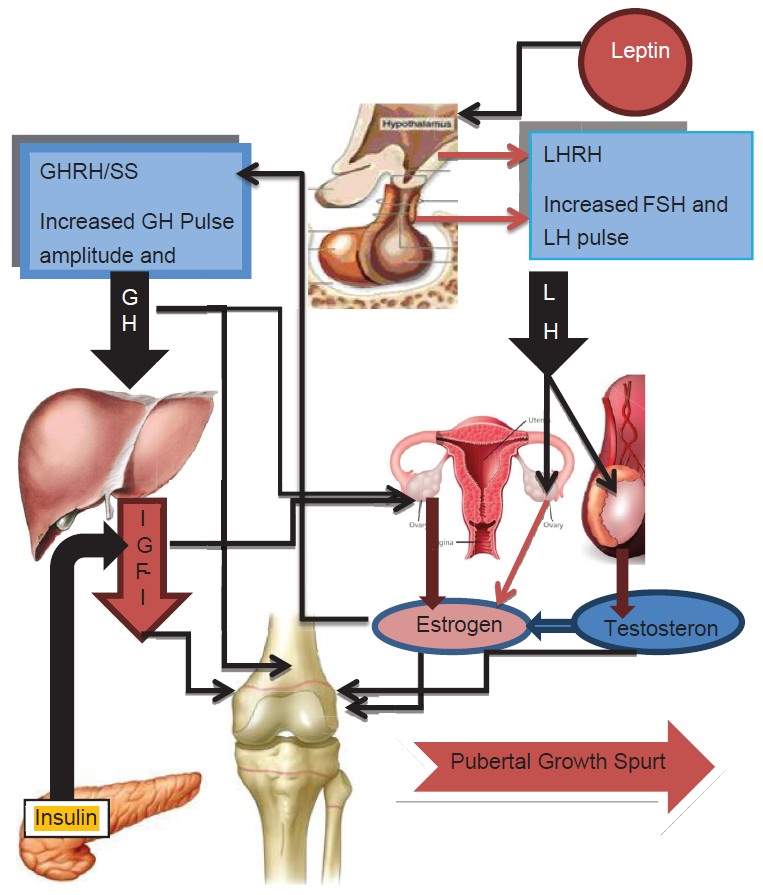
Fig 2.5: The diagram below shows the pubertal growth spurt and sexual development.
CONCLUSIONS AND RECOMMENDATIONS.
The results of increase in fracture risk, bone loss and osteoporosis should be major concerns for patients and health care providers. The increase in age in population, the more prolonged the effects of osteoporosis including pain, loss of independence and institutionalized care will become more common (Sözen et al., 2017). However, educating population about healthy lifestyle is a major way to prevent bone loss and osteoporosis, including optimal calcium and vitamin D and exercise in adolescence. Throughout life this education should be conducted, majorly during times of increased bone loss for example, menopause transition.
This write up is about bone health; calcium and vitamin D. Although dietary sources of both nutrients are available, a number of people do not receive sufficient amounts for a healthy bone formation. In addition, the damaging effects of sunlight has reduced vitamin D synthesis from the skin. Notwithstanding, supplements that can supply the body with sufficient amounts of nutrient necessary for bone health are now available. As seen in the introduction, there are a few evidences which support the fact that calcium and vitamin D alone can reduce fractures and also prevent bone loss.
Recommendation.
Office officials should remind patients about bone health per time, for example when scheduling bone density testing. The health care staffs should review proper nutrition and supplementation at appropriate times when needed. For example, examinations performed annually are perfect periods to review calcium and vitamin D intake with supplementation reviewed recommendations. However, a vital role of the pharmacists is making patients aware of the importance of calcium and vitamin D with osteoporosis therapy prescriptions, which includes administration to confirm absorption of bisphosphonate medications.
Epidemiology Evidence.
- Vertebral, hip and wrist fractures are commonly related with osteoporosis.
- In England and Wales about £1.7 billion is attributed to fractures.
(Christodoulou & Cooper, 2003)
Bibliography
Ahvazi, B., Boeshans, K. M., Idler, W., Baxa, U. & Steinert, P. M. (2003) Roles of Calcium Ions in the Activation and Activity of the Transglutaminase 3 Enzyme. The Journal of biological chemistry [Online], 278 (26) June, pp. 23834–23841. Available from: <http://dx.doi.org/10.1074/jbc.M301162200>.
Akgül, F., Serçelik, A., Çetin, H. & Erten, T. (2017) Association of Parathyroid Hormone and Vitamin D with Untreated Hypertension: Is It Different in White-Coat or Sustained Hypertension? PloS one [Online], 12 (11) November, p. e0188669. Available from: <http://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0188669&type=printable> [Accessed 4 May 2018].
Alonso, N., Calero-Paniagua, I. & Del Pino-Montes, J. (2017) Clinical and Genetic Advances in Paget’s Disease of Bone: A Review. Clinical reviews in bone and mineral metabolism [Online], 15 (1), pp. 37–48. Available from: <http://dx.doi.org/10.1007/s12018-016-9226-0>.
Bauer, D. C. (2013) Clinical Practice. Calcium Supplements and Fracture Prevention. The New England journal of medicine [Online], 369 (16) October, pp. 1537–1543. Available from: <http://dx.doi.org/10.1056/NEJMcp1210380>.
Beto, J. A. (2015) The Role of Calcium in Human Aging. Clinical nutrition research [Online], 4 (1) January, pp. 1–8. Available from: <http://dx.doi.org/10.7762/cnr.2015.4.1.1>.
Bikle, D. (2009) Nonclassic Actions of Vitamin D. The Journal of clinical endocrinology and metabolism [Online], 94 (1) January, pp. 26–34. Available from: <http://dx.doi.org/10.1210/jc.2008-1454>.
Blake, G. M. & Fogelman, I. (2007) The Role of DXA Bone Density Scans in the Diagnosis and Treatment of Osteoporosis. Postgraduate medical journal [Online], 83 (982) August, pp. 509–517. Available from: <http://dx.doi.org/10.1136/pgmj.2007.057505>.
Body, J.-J., Bergmann, P., Boonen, S., Devogelaer, J.-P., Gielen, E., Goemaere, S., Kaufman, J.-M., Rozenberg, S. & Reginster, J.-Y. (2012) Extraskeletal Benefits and Risks of Calcium, Vitamin D and Anti-Osteoporosis Medications. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA [Online], 23 Suppl 1 February, pp. S1–S23. Available from: <http://dx.doi.org/10.1007/s00198-011-1891-8>.
Bosch, X., Poch, E. & Grau, J. M. (2009) Rhabdomyolysis and Acute Kidney Injury. The New England journal of medicine [Online], 361 (1) July, pp. 62–72. Available from: <https://doi.org/10.1056/NEJMra0801327>.
Braet, K., Cabooter, L., Paemeleire, K. & Leybaert, L. (2004) Calcium Signal Communication in the Central Nervous System. Biology of the cell / under the auspices of the European Cell Biology Organization [Online], 96 (1) February, pp. 79–91. Available from: <http://dx.doi.org/10.1016/j.biolcel.2003.10.007>.
Bronner, F. (2003) Mechanisms of Intestinal Calcium Absorption. Journal of cellular biochemistry [Online], 88 (2) February, pp. 387–393. Available from: <http://dx.doi.org/10.1002/jcb.10330>.
Burckhardt, P. (2015) Calcium Revisited, Part III: Effect of Dietary Calcium on BMD and Fracture Risk. BoneKEy reports [Online], 4 August, p. 708. Available from: <http://dx.doi.org/10.1038/bonekey.2015.77>.
Calvez, J., Poupin, N., Chesneau, C., Lassale, C. & Tomé, D. (2011) Protein Intake, Calcium Balance and Health Consequences. European journal of clinical nutrition [Online], 66 November, p. 281. Available from: <http://dx.doi.org/10.1038/ejcn.2011.196>.
Cavalcoli, F., Zilli, A., Conte, D. & Massironi, S. (2017) Micronutrient Deficiencies in Patients with Chronic Atrophic Autoimmune Gastritis: A Review. World journal of gastroenterology: WJG [Online], 23 (4) January, pp. 563–572. Available from: <http://dx.doi.org/10.3748/wjg.v23.i4.563>.
Chin, K., Appel, L. J. & Michos, E. D. (2017) Vitamin D, Calcium, and Cardiovascular Disease: A‘D’vantageous or ‘D’etrimental? An Era of Uncertainty. Current atherosclerosis reports [Online], 19 (1) January, p. 5. Available from: <http://dx.doi.org/10.1007/s11883-017-0637-2>.
Christodoulou, C. & Cooper, C. (2003) What Is Osteoporosis? Postgraduate medical journal [Online], 79 (929) March, pp. 133–138. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/12697910>.
Ferrucci, L., Baroni, M., Ranchelli, A., Lauretani, F., Maggio, M., Mecocci, P. & Ruggiero, C. (2014) Interaction between Bone and Muscle in Older Persons with Mobility Limitations. Current pharmaceutical design [Online], 20 (19), pp. 3178–3197. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/24050165>.
Fischer, V., Haffner-Luntzer, M., Prystaz, K., Scheidt, A. V., Busse, B., Schinke, T., Amling, M. & Ignatius, A. (2017) Calcium and Vitamin-D Deficiency Marginally Impairs Fracture Healing but Aggravates Posttraumatic Bone Loss in Osteoporotic Mice. Scientific reports [Online], 7 (1) August, p. 7223. Available from: <https://doi.org/10.1038/s41598-017-07511-2>.
Gilsanz, V., Chalfant, J., Kalkwarf, H., Zemel, B., Lappe, J., Oberfield, S., Shepherd, J., Wren, T. & Winer, K. (2011) Age at Onset of Puberty Predicts Bone Mass in Young Adulthood. The Journal of pediatrics [Online], 158 (1) January, pp. 100–105, 105.e1–e2. Available from: <http://dx.doi.org/10.1016/j.jpeds.2010.06.054>.
Gong, H., Hatch, V., Ali, L., Lehman, W., Craig, R. & Tobacman, L. S. (2005) Mini-Thin Filaments Regulated by Troponin–tropomyosin. Proceedings of the National Academy of Sciences of the United States of America [Online], 102 (3) January, pp. 656–661. Available from: <http://www.pnas.org/content/102/3/656> [Accessed 26 April 2018].
Gröber, U. & Kisters, K. (2012) Influence of Drugs on Vitamin D and Calcium Metabolism. Dermato-endocrinology [Online], 4 (2) April, pp. 158–166. Available from: <http://dx.doi.org/10.4161/derm.20731>.
Han, H., Segal, A. M., Seifter, J. L. & Dwyer, J. T. (2015) Nutritional Management of Kidney Stones (Nephrolithiasis). Clinical nutrition research [Online], 4 (3) July, pp. 137–152. Available from: <http://dx.doi.org/10.7762/cnr.2015.4.3.137>.
Hernlund, E., Svedbom, A., Ivergård, M., Compston, J., Cooper, C., Stenmark, J., McCloskey, E. V., Jönsson, B. & Kanis, J. A. (2013) Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. Archives of osteoporosis [Online], 8 (1) October, p. 136. Available from: <https://doi.org/10.1007/s11657-013-0136-1>.
Hessel, A. L., Lindstedt, S. L. & Nishikawa, K. C. (2017) Physiological Mechanisms of Eccentric Contraction and Its Applications: A Role for the Giant Titin Protein. Frontiers in physiology [Online], 8 February, p. 70. Available from: <http://dx.doi.org/10.3389/fphys.2017.00070>.
Higgs, J., Derbyshire, E. & Styles, K. (2017) Nutrition and Osteoporosis Prevention for the Orthopaedic Surgeon: A Wholefoods Approach. EFORT open reviews [Online], 2 (6) June, pp. 300–308. Available from: <http://dx.doi.org/10.1302/2058-5241.2.160079>.
Iruzubieta, P., Terán, Á., Crespo, J. & Fábrega, E. (2014) Vitamin D Deficiency in Chronic Liver Disease. World journal of hepatology [Online], 6 (12) December, pp. 901–915. Available from: <http://dx.doi.org/10.4254/wjh.v6.i12.901>.
Ismail, A. & Ismail, N. A. (2016) Magnesium: A Mineral Essential for Health yet Generally Underestimated or Even Ignored. Journal of nutrition & food sciences [Online], 6 (523), p. 2. Available from: <http://dx.doi.org/10.4172/2155-9600.1000523Ismail>.
Kling, J. M., Clarke, B. L. & Sandhu, N. P. (2014) Osteoporosis Prevention, Screening, and Treatment: A Review. Journal of women’s health [Online], 23 (7) July, pp. 563–572. Available from: <http://dx.doi.org/10.1089/jwh.2013.4611>.
Konstantakis, C., Tselekouni, P., Kalafateli, M. & Triantos, C. (2016) Vitamin D Deficiency in Patients with Liver Cirrhosis. Annales de gastroenterologie et d’hepatologie [Online], 29 (3) July, pp. 297–306. Available from: <http://dx.doi.org/10.20524/aog.2016.0037>.
Kopic, S. & Geibel, J. P. (2013) Gastric Acid, Calcium Absorption, and Their Impact on Bone Health. Physiological reviews [Online], 93 (1) January, pp. 189–268. Available from: <http://dx.doi.org/10.1152/physrev.00015.2012>.
Kuo, I. Y. & Ehrlich, B. E. (2015) Signaling in Muscle Contraction. Cold Spring Harbor perspectives in biology [Online], 7 (2) February, p. a006023. Available from: <http://dx.doi.org/10.1101/cshperspect.a006023>.
Laird, E., Ward, M., McSorley, E., Strain, J. J. & Wallace, J. (2010) Vitamin D and Bone Health: Potential Mechanisms. Nutrients [Online], 2 (7) July, pp. 693–724. Available from: <http://dx.doi.org/10.3390/nu2070693>.
Lamy, O. & Burckhardt, P. (2014) Calcium Revisited: Part II Calcium Supplements and Their Effects. BoneKEy reports [Online], 3 October, p. 579. Available from: <http://dx.doi.org/10.1038/bonekey.2014.74>.
Lean, M. E. J. & Combet, E. (2016) Barasi’s Human Nutrition: A Health Perspective, Third Edition [Online]. CRC Press. Available from: <https://www.amazon.co.uk/Barasis-Human-Nutrition-Health-Perspective/dp/1444137204/ref=sr_1_2?s=books&ie=UTF8&qid=1524673550&sr=1-2>.
Levine, M. A. (2012) Assessing Bone Health in Children and Adolescents. Indian journal of endocrinology and metabolism [Online], 16 (Suppl 2) December, pp. S205–S212. Available from: <http://dx.doi.org/10.4103/2230-8210.104040>.
Lorentzon, M. & Cummings, S. R. (2015) Osteoporosis: The Evolution of a Diagnosis. Journal of internal medicine [Online], 277 (6) June, pp. 650–661. Available from: <http://doi.wiley.com/10.1111/joim.12369>.
Lourida, I., Thompson-Coon, J., Dickens, C. M., Soni, M., Kuźma, E., Kos, K. & Llewellyn, D. J. (2015) Parathyroid Hormone, Cognitive Function and Dementia: A Systematic Review. PloS one [Online], 10 (5) May, p. e0127574. Available from: <http://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0127574&type=printable> [Accessed 4 May 2018].
Marks, A. R. (2003) Calcium and the Heart: A Question of Life and Death. The Journal of clinical investigation [Online], 111 (5) March, pp. 597–600. Available from: <http://dx.doi.org/10.1172/JCI18067>.
Nair, R. & Maseeh, A. (2012) Vitamin D: The ‘Sunshine’ Vitamin. Journal of pharmacology & pharmacotherapeutics [Online], 3 (2) April, pp. 118–126. Available from: <http://dx.doi.org/10.4103/0976-500X.95506>.
Nair, S. (2010) Vitamin D Deficiency and Liver Disease. Gastroenterology & hepatology [Online], 6 (8) August, pp. 491–493. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/20978551>.
Nazrun, A. S., Tzar, M. N., Mokhtar, S. A. & Mohamed, I. N. (2014) A Systematic Review of the Outcomes of Osteoporotic Fracture Patients after Hospital Discharge: Morbidity, Subsequent Fractures, and Mortality. Therapeutics and clinical risk management [Online], 10 November, pp. 937–948. Available from: <http://dx.doi.org/10.2147/TCRM.S72456>.
Newman, C. L., Tian, N., Hammond, M. A., Wallace, J. M., Brown, D. M., Chen, N. X., Moe, S. M. & Allen, M. R. (2016) Calcitriol Suppression of Parathyroid Hormone Fails to Improve Skeletal Properties in an Animal Model of Chronic Kidney Disease. American journal of nephrology [Online], 43 (1) February, pp. 20–31. Available from: <http://dx.doi.org/10.1159/000444423>.
Paul Tuck, S., Layfield, R., Walker, J., Mekkayil, B. & Francis, R. (2017) Adult Paget’s Disease of Bone: A Review. Rheumatology [Online], 56 (12) December, pp. 2050–2059. Available from: <http://dx.doi.org/10.1093/rheumatology/kew430>.
Pereira, G. A. P., Genaro, P. S., Pinheiro, M. M., Szejnfeld, V. L. & Martini, L. A. (2009) Dietary Calcium: Strategies to Optimize Intake. Revista brasileira de reumatologia [Online], 49 (2), pp. 164–171. Available from: <http://www.scielo.br/scielo.php?pid=S0482-50042009000200008&script=sci_arttext&tlng=en> [Accessed 28 April 2018].
Pesce, V., Speciale, D., Sammarco, G., Patella, S., Spinarelli, A. & Patella, V. (2009) Surgical Approach to Bone Healing in Osteoporosis. Clinical cases in mineral and bone metabolism: the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases [Online], 6 (2) May, pp. 131–135. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/22461162>.
Pohlkamp, T., Wasser, C. R. & Herz, J. (2017) Functional Roles of the Interaction of APP and Lipoprotein Receptors. Frontiers in molecular neuroscience [Online], 10, p. 54. Available from: <https://www.frontiersin.org/article/10.3389/fnmol.2017.00054>.
Pu, F., Chen, N. & Xue, S. (2016) Calcium Intake, Calcium Homeostasis and Health. Food Science and Human Wellness [Online], 5 (1) March, pp. 8–16. Available from: <http://www.sciencedirect.com/science/article/pii/S2213453016000021>.
Rajagopal, S. & Ponnusamy, M. (2017) Calcium Ion in Biological Systems [Online]. In: Rajagopal, S. & Ponnusamy, M. ed., Calcium Signaling: From Physiology to Diseases. Singapore: Springer Singapore, pp. 1–14. Available from: <https://doi.org/10.1007/978-981-10-5160-9_1>.
Reshetnyak, V. I. (2015) Primary Biliary Cirrhosis: Clinical and Laboratory Criteria for Its Diagnosis. World journal of gastroenterology: WJG [Online], 21 (25) July, pp. 7683–7708. Available from: <http://dx.doi.org/10.3748/wjg.v21.i25.7683>.
Robinson, R. (2010) Structure of Signaling Enzyme Reveals How Calcium Turns It On. PLoS biology [Online], 8 (7) July, p. e1000427. Available from: <http://journals.plos.org/plosbiology/article/file?id=10.1371/journal.pbio.1000427&type=printable> [Accessed 26 April 2018].
Ruat, M. & Traiffort, E. (2013) Roles of the Calcium Sensing Receptor in the Central Nervous System. Best practice & research. Clinical endocrinology & metabolism [Online], 27 (3) June, pp. 429–442. Available from: <http://dx.doi.org/10.1016/j.beem.2013.03.001>.
Sheu, A. & Diamond, T. (2016) Bone Mineral Density: Testing for Osteoporosis. Australian prescriber [Online], 39 (2) April, pp. 35–39. Available from: <http://dx.doi.org/10.18773/austprescr.2016.020>.
Soliman, A., De Sanctis, V., Elalaily, R. & Bedair, S. (2014) Advances in Pubertal Growth and Factors Influencing It: Can We Increase Pubertal Growth? Indian journal of endocrinology and metabolism [Online], 18 (Suppl 1) November, pp. S53–S62. Available from: <http://dx.doi.org/10.4103/2230-8210.145075>.
Sorensen, M. D. (2014) Calcium Intake and Urinary Stone Disease. Translational andrology and urology [Online], 3 (3) September, pp. 235–240. Available from: <http://dx.doi.org/10.3978/j.issn.2223-4683.2014.06.05>.
Sözen, T., Özışık, L. & Başaran, N. Ç. (2017) An Overview and Management of Osteoporosis. European journal of rheumatology and inflammation [Online], 4 (1) March, pp. 46–56. Available from: <http://dx.doi.org/10.5152/eurjrheum.2016.048>.
Suadicani, S. O., Cherkas, P. S., Zuckerman, J., Smith, D. N., Spray, D. C. & Hanani, M. (2010) Bidirectional Calcium Signaling between Satellite Glial Cells and Neurons in Cultured Mouse Trigeminal Ganglia. Neuron glia biology [Online], 6 (1) February, pp. 43–51. Available from: <http://dx.doi.org/10.1017/S1740925X09990408>.
Sunyecz, J. A. (2008) The Use of Calcium and Vitamin D in the Management of Osteoporosis. Therapeutics and clinical risk management [Online], 4 (4) August, pp. 827–836. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/19209265>.
Szent-Györgyi, A. G. (1975) Calcium Regulation of Muscle Contraction. Biophysical journal [Online], 15 (7) July, pp. 707–723. Available from: <http://dx.doi.org/10.1016/S0006-3495(75)85849-8>.
Teng, G. G., Curtis, J. R. & Saag, K. G. (2008) Mortality and Osteoporotic Fractures: Is the Link Causal, and Is It Modifiable? Clinical and experimental rheumatology [Online], 26 (5 Suppl 51) September, pp. S125–S137. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/19026155>.
Torres, P. A., Helmstetter, J. A., Kaye, A. M. & Kaye, A. D. (2015) Rhabdomyolysis: Pathogenesis, Diagnosis, and Treatment. The Ochsner journal [Online], 15 (1) Spring, pp. 58–69. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/25829882>.
Uday, S. & Högler, W. (2017) Nutritional Rickets and Osteomalacia in the Twenty-First Century: Revised Concepts, Public Health, and Prevention Strategies. Current osteoporosis reports [Online], 15 (4) August, pp. 293–302. Available from: <http://dx.doi.org/10.1007/s11914-017-0383-y>.
Veldurthy, V., Wei, R., Oz, L., Dhawan, P., Jeon, Y. H. & Christakos, S. (2016) Vitamin D, Calcium Homeostasis and Aging. Bone Research [Online], 4 October, p. 16041. Available from: <http://dx.doi.org/10.1038/boneres.2016.41>.
Vestergaard, P. (2006) Current Pharmacological Options for the Management of Primary Hyperparathyroidism. Drugs [Online], 66 (17), pp. 2189–2211. Available from: <https://www.ncbi.nlm.nih.gov/pubmed/17137403>.
Wang, L., Li, M., Cao, Y., Han, Z., Wang, X., Atkinson, E. J., Liu, H. & Amin, S. (2017) Proton Pump Inhibitors and the Risk for Fracture at Specific Sites: Data Mining of the FDA Adverse Event Reporting System. Scientific reports [Online], 7 (1) July, p. 5527. Available from: <https://doi.org/10.1038/s41598-017-05552-1>.
Witteveen, J. E., Thiel, S. van, Romijn, J. A. & Hamdy, N. A. T. (2013) Hungry Bone Syndrome: Still a Challenge in the Post-Operative Management of Primary Hyperparathyroidism: A Systematic Review of the Literature. European journal of endocrinology / European Federation of Endocrine Societies [Online], 168 (3) March, pp. R45–R53. Available from: <http://dx.doi.org/10.1530/EJE-12-0528>.
Yang, C. H., Perumpail, B. J., Yoo, E. R., Ahmed, A. & Kerner, J. A., Jr (2017) Nutritional Needs and Support for Children with Chronic Liver Disease. Nutrients [Online], 9 (10) October. Available from: <http://dx.doi.org/10.3390/nu9101127>.
Yang, Y.-X. (2012) Chronic Proton Pump Inhibitor Therapy and Calcium Metabolism. Current gastroenterology reports [Online], 14 (6) December, pp. 473–479. Available from: <http://dx.doi.org/10.1007/s11894-012-0290-4>.
Yang, Y.-X., Lewis, J. D., Epstein, S. & Metz, D. C. (2006) Long-Term Proton Pump Inhibitor Therapy and Risk of Hip Fracture. JAMA: the journal of the American Medical Association [Online], 296 (24) December, pp. 2947–2953. Available from: <http://dx.doi.org/10.1001/jama.296.24.2947>.
Yu, E. W., Bauer, S. R., Bain, P. A. & Bauer, D. C. (2011) Proton Pump Inhibitors and Risk of Fractures: A Meta-Analysis of 11 International Studies. The American journal of medicine [Online], 124 (6) June, pp. 519–526. Available from: <http://dx.doi.org/10.1016/j.amjmed.2011.01.007>.
Zhang, J., Zhang, Z. & Yu, A. (2001) Discussion on the Mechanism of the Calcium Absorption in the Human Body. Chinese science bulletin = Kexue tongbao [Online], 46 (16) August, pp. 1403–1408. Available from: <https://doi.org/10.1007/BF03183399>.
Zhao, J.-G., Zeng, X.-T., Wang, J. & Liu, L. (2017) Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. JAMA: the journal of the American Medical Association [Online], 318 (24) December, pp. 2466–2482. Available from: <https://jamanetwork.com/journals/jama/article-abstract/2667071> [Accessed 25 April 2018].
Zoch, M. L., Clemens, T. L. & Riddle, R. C. (2016) New Insights into the Biology of Osteocalcin. Bone [Online], 82 January, pp. 42–49. Available from: <http://dx.doi.org/10.1016/j.bone.2015.05.046>.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medicine"
The area of Medicine focuses on the healing of patients, including diagnosing and treating them, as well as the prevention of disease. Medicine is an essential science, looking to combat health issues and improve overall well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




