Literature Review on Chronic Back Pain and Depression
Info: 15372 words (61 pages) Example Literature Review
Published: 19th Apr 2021
Tagged: PhysiologyMental HealthMedicine
Table of Contents
Prevalence of LBP among young females
Females are at a greater risk of depression
What is the association between CLBP/chronic pain and depression in the youth?
Adolescents with pain are more likely to have depression
Activity levels and fear avoidance model
Predisposing and protective factors for comorbid depression in young with pain
Chronic pain and depression have common risk factors
Sleep disturbance, chronic pain and depression
Pattern of pain prescriptions among youth with chronic pain
Table of Figures
Figure 1 Review Process of the Literature
Figure 2 Source: AIHW analysis of ABS Microdata: National Health Survey, 2014–15
Figure 3 Prevalence of mental disorders across age groups
Figure 4 Original version of fear avoidance model
Figure 5 Modified Fear avoidance model predicting depression in paediatric population
Figure 6 Fear avoidance model predicting disability in paediatric population
Figure 7 Psychological factors impacting the Fear Avoidance Model
Tables
Table 1 Search Statement
Table 2 Studies demonstrating an association between pain and depression
Table 3 Studies examination activity levels and biomechanical factors
Table 4 Studies exploring the psychosocial variables associated with pain
Table 5 Studies examining the association of sleep disturbance with pain and depression
Introduction
Young Australian females have the greatest prevalence of psychological distress when compared across all age groups (1). Between 2011-12 and 2014-15, young females in the 18-24 age group were the only age group in Australia to have reported an increase in the prevalence of psychological distress (increasing from 13% to 20%) (1). What is concerning is whether this reduced mental wellbeing in young females will lead to a reciprocal rise in the incidence of low back pain (LBP[1]), as such pain often co-exists with depression leading to greater disability[2], reduced quality of life and increased healthcare visits among adolescents with chronic pain (2, 3). Furthermore, studies have demonstrated females are more likely to suffer from LBP than males (4, 5), and report greater stress levels from school that is associated with more health complaints, such as “musculoskeletal pain, fatigue, sleep disturbances, sadness and anxiety” (6). Adolescence and young adulthood is an opportunity for intervention to modify ?outcome as the onset of LBP frequently occurs in the 16-34 age group (7) as depicted in Figure 2 (prevalence 13.4% males, 14% females) (7). Since LBP that develops during adolescence is likely to persist into adulthood (8), along with the immense cost chronic LBP (CLBP) places on the Australian healthcare system ($1.2 billion per annum) (9), it is important to prevent or improve the management of LBP in this age group.
The majority of the research investigating the association between CLBP and depression is conducted in the older population (>40yrs). In contrast , research in the younger population explores chronic pain,[3] rather than CLBP specifically. Most of this research is conducted in countries outside of Australia as depicted in Table 2 – Table 5 (United States (10-13), Norway (14, 15), Sweden (16), Netherlands (17-19)), with only two studies conducted in young Australian adolescents and adults (3, 20). The existing chronic pain research involves children (8-12yrs) and younger adolescents (8-15yrs), and few young adults (18-25yrs). Therefore, to address this gap in the literature, this review aims to address the following primary research question: what is the association between CLBP and depression in young females aged 16-25yrs old? The aims to address this question by exploring the topics outlined in the table of contents above.
Methods
Literature search
Three databases (PubMed, PsycINFO, Cinahl) were searched in February 2017 using the following Medical Subject Headings (MeSH) terms, titles and Boolean term as shown in Table 1.
Table 1 Search Statement
| MeSH* | Titles | |
| OR | Low back pain
Chronic pain |
Low back pain
Chronic pain |
| AND | ||
| OR | Depression
Anxiety Mental health |
Depression
Anxiety Mental health |
*Medical Subject Headings
Database filters were applied for all three searches as shown below:
- Age was restricted to adolescents (13-18yrs old) and young adults (19-24yrs old)
- Females
- Humans
- Last 10 years
- English language
Review procedure
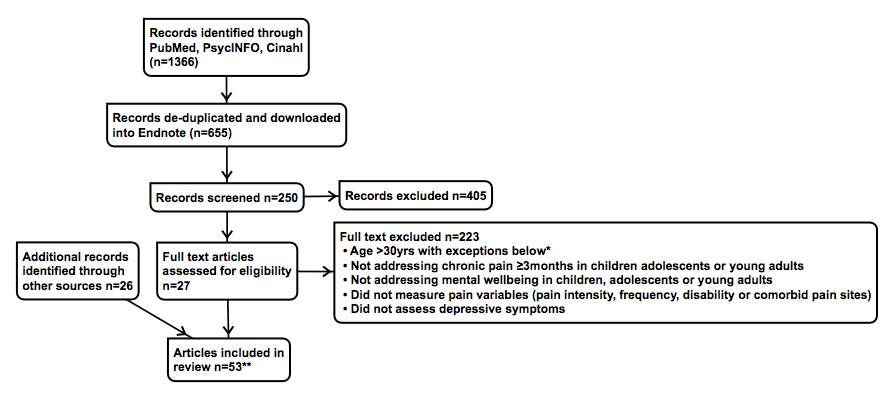
Figure 1 Review Process of the Literature
*Most studies relating to childhood adversities and alexithymia comprised mainly older adults (40-50yrs old).
**Not all articles were included in the table
Discussion
Prevalence of LBP among young females
Four studies (3, 4, 11, 20) from Australia, United States and Greece have reported the prevalence of LBP in community-dwelling adolescents and young adults to range between 15.2%-41%. Only two Australian studies compared the prevalence of LBP between females and males. While Beales et al stated significantly more females reported a “lifetime experience of LBP” compared to males (55.8% vs 41.8%) (3), Rees et al stated significantly more females reported comorbid back and neck pain compared to males (17.6% vs 9.1%, p
Females are more affected by LBP. The study by Beales et al demonstrated females reported lower quality of life in both physical and mental components compared to males (p
Females are at a greater risk of depression
According to Australia Bureau of Statistics, mental health disorders is most prevalent in the 16-24yr old age group and it decreases with age as depicted in Figure 3, with 76% of mental disorders developing before the age of 25 (21). In 2007, more females than males (30% vs 23%) in the 16-24 age group were symptomatic for a mental disorder, with anxiety (20% vs 12%) being the most common followed by mood disorders (8% vs 4%) (21), which often coexist together. Poorer mental wellbeing in females is also replicated in two other cross sectional studies in Greece and Sweden with a significantly greater proportion of females reporting persistent stress (22% vs 7%, p=0.0001), depressed mood (6% vs 2%, p=0.0055), persistent nervousness (15% vs 7%, p=0.036), persistent fatigue (19% vs 7%, p=0.0001) (4), sadness (p=0.000), and school-related stress (p=0.000) (6).
What is the association between CLBP/chronic pain and depression in the youth?
Adolescents with pain are more likely to have depression
Depression and poor emotional wellbeing are more prevalent in children and adolescents with chronic pain (12, 20). A study involving college students (18-30yrs) demonstrated that LBP is significantly associated with greater depression scores (13). However, limitations of this study include no specification of pain duration and the possibility of selection bias, as all participants were recruited from the New York Institute of Technology where sedentary lifestyle may act as a confounding factor. Nevertheless, the results reported are consistent with two other cross sectional studies involving community-dwelling adolescents. Beales et al revealed adolescent females with LBP are more likely to suffer from depression/anxiety compared to males (84.1% vs 15.9%, p[4]=1.86, p
Pain and depression is a comorbidity with worse outcomes. The first study to explore the impact of comorbidities on LBP in 17yr old adolescents revealed anxiety/depression are significant comorbidities associated with LBP leading to reduced quality of life (3). Results from another study that investigated the impact of psychological and lifestyle factors on chronic pain revealed depressive/anxiety symptoms have the strongest association with chronic pain, more so than lifestyle factors (15). Akin to adult studies, a few studies in the youth with pain demonstrated higher depression scores are associated with (13, 15) or a significant predictor (ß=0.36, p=0.04) (17) of self-reported disability[5] (11, 17). Therefore, depression and chronic pain commonly co-exist leading to greater disability, which is no surprise since they share common neurobiological pathways (22). Hence, it is important to address these two most commonly occurring conditions early in life to prevent long term disability.
Activity levels and fear avoidance model
There is an inter-related relationship between activity levels, pain severity[6] and depression partly driven by pain catastrophizing[7]. Fear avoidance model (FAM) in Figure 4 (23) demonstrated pain catastrophizing drives pain related fear resulting in avoidance of activities, which reduces the pain threshold (24). This in turn leads to increased pain severity and further avoidance of activities, which results in a viscous cycle of deconditioning. A study by Long et al supported the FAM as it demonstrated a reciprocal relationship between activity levels and pain frequency (-0.66
Evidence to support the association between activity levels and depression in the younger population is equivocal. The FAM produced by Vlaeyen & Linton 2000 in adults with CLBP also predicted depression as an outcome Figure 4 (25), which is supported by Long et al where higher activity levels were inversely correlated with less depressive symptoms (-0.39
Predisposing and protective factors for comorbid depression in young with pain
Studies in adolescents have suggested that pain beliefs may be more important than pain severity in determining the risk for depression. A study conducted in adolescents and young adults demonstrated depression accounted for the frustration of not being able to achieve desired goals in personal values (p = 0.02), social acceptance (p
The association between pain severity and depression is equivocal depending on the study design used. Two cross sectional studies have exhibited severity[8] did not differ according to depression, disability and LBP status (11, 13). Instead, one of the studies demonstrated a significant association between the grade of depression and “pain interference” (F=3.50, p[9] would be high among adolescents. The different results reported between cross sectional and longitudinal studies above emphasise the need for more longitudinal studies as pain and depression exist in a dynamic biopsychosocial model that changes with time. Pain intensity in cross sectional studies were merely a snapshot of the participant’s momentary subjective pain experience. Whereas in longitudinal studies, changes in pain intensity can be monitored over time, which is probably more reflective of the factors that influence pain intensity or perception over time, namely, pain catastrophizing and pain related fear (23, 31, 32). These cognitive factors have been shown to influence pain perception and depression in the FAM and PCS[10]. But these are yet to be explored in young females with LBP.
Thus far one study has speculated pain related beliefs may contribute to comorbid depression/anxiety in adolescents with LBP. This study identified four distinct LBP subgroups. Although group 2 had a higher likelihood for LBP diagnosis compared to group 3, group 3 but not group 2 exhibited an increased likelihood for comorbid anxiety/depression, sleep disturbance and eating disorders (3), as well as a significantly lower quality of life. The protective and risk factors for comorbid depression/anxiety in group 2 and 3 were not assessed in this study. Nevertheless the author suggested physical factors, (spinal curvature and back endurance (13)), lifestyle factors (sedentary activity (15), obesity (15), school bags (33), smoking (15)) and alterations in nociceptive processing may play an important role in group 2. Whereas “pain related beliefs, self-efficacy and locus of control” may play a more important in group 3. The validation of the FAM in the paediatric population above has demonstrated negative pain beliefs, such as catastrophizing, pain related fear play an important role towards the development of depression (23).
On the other hand, family cohesion and control beliefs act as protective factors against depression (11, 34). Good family cohesion protected emotional wellbeing from the negative impacts of disability associated with chronic pain (34). Similarly, another study revealed peer support is fundamental to “independence, emotional adjustment and identity formation” (35), which all contribute to a well-balanced mental health. Therefore, pain related cognitions should be routinely screened and targeted in treatment to reduce the risk of depression and disability.
Currently two studies have incorporated cognitive factors into screening tools to risk stratify adolescents with chronic pain into subgroups. The most promising tool was the BAPQ that correctly risk stratified 95% of participants (34), while the PPST correctly allocated 71-79% of participants on a 4month follow up (36). However, both of these tools have been validated in samples recruited from secondary or tertiary pain clinics and are yet to be validated in the general community where they will be most useful, as primary care is often the first point of contact where early intervention can be implemented. Nevertheless, these two studies have demonstrated depressive symptoms, catastrophizing, disability, pain related fear, anxiety and sleep disturbance have some prognostic value for disability in children and adolescents with chronic pain.
Negative pain related cognitions may persist into adulthood leading to reduced resilience. A study by Ruehlman et al demonstrated depressed young adults with chronic pain shared similar pain beliefs (PCP:EA[11]) with “non-resilient” adults (11). Clinically depressed adolescents and “non-resilient” adults had similar pain related fear (M=8.46 vs 9.49) and control belief (M=17.14 vs 17.28) scores. Meanwhile, catastrophizing (M=7.69 vs 8.83) and perceived disability (M=4.65 vs 11.59) was higher in “non-resilient” adults (11), which suggest catastrophizing is a dynamic factor that should be targeted early in the phase of chronic pain to prevent long term disability associated with reduced self-efficacy and depression. However, compliance rates are lower for psychological treatments (73%) compared to medication (94%) and physical treatments (92%) (36). In addition, adolescents who were classified as high risk based on PPST were more likely to be non-compliant with psychological treatments at 4month follow up (36). Therefore, factors that influence engagement with healthcare services and treatment programs need to be explored to improve outcomes for young females with LBP and depression.
Longitudinal studies offer greater insight into the bidirectional relationship between pain and depression. Aforementioned results reported by Holley et al demonstrated pain may have a stronger impact on depression than vice versa. This is supported by another 12month longitudinal study that reported depressive symptoms predicted both the number of pain sites and multiple frequent pain sites at 1-year follow up (14). Although this finding is statistically significant, depressive symptoms only explained 11% of variance in pain outcomes (14), which suggest pain may have a stronger influence over depression. However, a multinational study conducted in adults reported contradicting results whereby early onset of mental disorder (
Chronic pain and depression have common risk factors
Childhood adversities (CAs) are a risk factor for chronic pain in a “dose-dependent” manner (38-40) and depression (41). A multinational (37) and smaller cross sectional study in Japan (40) revealed physical and sexual abuse are significant risk factors for chronic back pain in adults. While a longitudinal study conducted in adolescents also revealed parental divorce during the 1-year of follow up is associated with frequent back pain co-existing with other pain sites (14). In the multinational study conducted in adults, the risk of chronic back/neck pain increased with the number of CAs: one CA (HR=1.13, p
CAs also predisposes to alexithymia[12] (42, 43) which is often associated with chronic pain (39, 44). A Finland study exhibited a correlation between the prevalence of alexithymia and pain status: no pain 4%, acute pain 6.6%, chronic pain 10.9% (39). Moreover, “difficulty identifying feelings” measured on the TAS-20[13] scale is significantly correlated with chronic pain in the general Japanese community (39). A study conducted in a health centre of United States also revealed alexithymic scores was significantly higher in adult females with intractable CLBP compared to controls (45). All these findings suggest difficulties with recognition of aversive emotions within oneself may lead to expression of these unrecognised emotions as somatic complaints such as pain (46). Therefore alexithymia may be a perpetuating factor for chronic pain.
The association between alexithymia and pain/depression may lead to greater disability among adults with chronic pain. A Finland study conducted in adults demonstrated the negative impact of alexithymia on pain intensity and disability was mediated by depression (44). This study also stated there was a moderate association between depression and specific components of alexithymia related to emotional regulation (difficulty identifying feelings: r=0.450, p≤0.01, difficulty describing feelings: r=0.464, p≤0.01). Most importantly, alexithymic score was also associated to with reduced life satisfaction[14] in Japanese adults with chronic pain (39). Given that alexithymia may reduce the quality of life in patients with chronic pain via its association with depression, poorer social support (47) and pain intensity, alexithymia is a promising target for intervention. A 6-month longitudinal study in adults demonstrated a decrease in the TAS-20 score is accompanied by a decrease in depression scores at follow up (48). The importance of emotional competence should not be under-estimated, as it is required for the identification and manipulation of unpleasant emotions to handle psychosocial challenges upon entering young adulthood (43). It is known that disruptions to emotional development and poor mental health (37) greatly contribute to pain conditions since pain perception consist of sensory, emotional and cognitive components (31). Therefore, alexithymia appears to be an intervention worth exploring in young females who are faced with many emotional challenges as they transition from adolescence to adulthood.
Sleep disturbance, chronic pain and depression
It is known that sleep disturbance[15] is more prevalent among adolescents and young adults with chronic pain (49, 50), and a significant mediator between pain intensity and disability (p≤0.01) (16). More specifically, a longitudinal study demonstrated adolescents with chronic pain reported poorer sleep quality[16] and a higher prevalence of insomnia symptoms compared to healthy adolescents, whereas total sleep time was comparable across both groups (49). Studies have shown sleep disturbance is a significant contributor to reduced quality of life (p
Sleep disturbance negatively impacts on pain in young adults with chronic pain. A cross sectional study in young adults revealed a significant and robust correlation between the severity of pain and sleep quality after controlling for demographic and psychological factors (ß=0.26, p[17] (OR=1.3) compared to those with no sleep disturbances at baseline (19). Notably, this prognostic effect of sleep disturbance was stronger in females than males. However, this same study revealed chronic pain and musculoskeletal pain severity had no significant effect on sleep disturbance. Meanwhile, another longitudinal study in adolescents demonstrated chronic pain was the strongest predictor for sleep disturbance (coefficient=1.52, 95% CI [0.90, 0.21], p[18] (2). This suggest there may be a bidirectional relationship between sleep and pain depending on the population studied, as Bonvanie et al was conducted in young adults from the community whereas Palermo et al was conducted in adolescents recruited from tertiary pain clinics.
Depression is known to be associated with sleep disturbance in adolescents and young adults with chronic pain. A cross sectional study by Graham et al reported an reciprocal association between depressive symptoms and sleep quality in young adults with chronic pain (r=0.39, p
Depression also impacts on sleep. A longitudinal study in adolescents demonstrated depressive symptoms are a significant risk factor for the persistence of insomnia over a 12month period (coefficient=0.05, p=0.031) (2). This is further supported by a study that reported depressive symptoms (ß=-0.32, p=0.07) and pre-sleep worry (ß=-0.43, p=0.02) were significant predictors for self-reported sleep quality (2). Although a longitudinal study conducted in adolescents revealed fatigue and not depressive symptoms mediated the predictive effect of sleep disturbance on chronic pain and musculoskeletal pain severity (19), another study revealed sleep disturbance mediated the effect of depression on fatigue (51). Therefore, sleep disturbance is not merely a symptom of depression, but also an important contributor to the association between pain and depression via fatigue.
Herein modifiable risk factors for insomnia could be potential targets for intervention. A study in young adults reported higher stress levels is significantly associated with reduced sleep quality (r=0.36, p
Sleep among young adults with chronic pain are more vulnerable to unhealthy lifestyle behaviours. A study in young college adults revealed health behaviours (alcohol, caffeine, exercise, typical diet, pain medication) are significant predictors of sleep quality among those with chronic pain only (∆R2=0.16, p
Pattern of pain prescriptions among youth with chronic pain
Based on three studies it seems adolescents and young adults with chronic pain are more likely to be prescribed pain medications. Among young adults from the community, having chronic pain increases the likelihood of having taken prescribed analgesia and over the counter (OTC) herbal preparations (50). Meanwhile a longitudinal study revealed 75% of adolescents with chronic pain were prescribed ≥1 of anti-depressants, anti convulsants or opioids for pain control, whereas none of healthy controls had been prescribed any of the mediations above (p
Conclusions
In summary, LBP/chronic pain and depression are common comorbidities in the younger population associated with reduced quality of life (3). Current literature has demonstrated young females are more vulnerable to this comorbidity and its associated consequences on a background of declining mental wellbeing over the past 6 years (1). Evidence strongly suggest mental health and pain co-exist in a bidirectional relationship within a biopsychosocial matrix (53). The fear avoidance model has demonstrated how activity levels and psychological factors (pain catastrophizing, pain related fear) contribute to depression and disability in children and adolescents with chronic pain (23). Meanwhile pain acceptance, sense of control, social support and good family cohesion are protective against depression. Childhood adversities, alexithymia and sleep disturbance appear to act as predisposing and perpetuating factors for this comorbidity but prospective studies are required to validate this.
Young Australian females are still an under-researched group and there is a great need to conduct more longitudinal studies in this population to determine the risk factors associated with this comorbidity. It will also be interesting to conduct a cross sectional survey to gain a deeper understanding of how lifestyle and healthcare factors may influence their engagement with health services.
Word count: 5229
Table 2 Studies demonstrating an association between pain and depression
| Association | Study design | Inclusion criteria | Sample | Measured variables | Adjustment | Aims |
| Holley et al (10)
United States |
Longitudinal with follow up at 6 and 12 months
No control group – chronic pain vs depression group |
Chronic pain
Depression |
|
Predictor
Outcome
|
|
Aim was to determine whether changes in pain intensity lead to changes in depressive symptoms and vice versa |
| Larsson et al (14)
Norway |
1-year longitudinal study with two time points (baseline and follow up after 1 year) |
|
Baseline
|
|
|
Examine the association between psychosocial factors and pain characteristics (number of pain, frequency, duration) other than pain type/location
Assess whether psychological factors are predictive of number of coexisting frequency pains at 1yr follow up |
| Beales et al (3)
Australia |
Cross sectional |
|
|
|
|
Explore the impact of common comorbidities on LBP in 17yr old adolescents
Results showed there was 4 distinct clusters with different SF-36 scores and LBP impacts |
| Korovessis et al (4)
Greece |
Cross sectional
No control group |
|
|
Pain variables
Biophysical
Psychological
Social
|
Gender | Revealed gender differences in the biophysical and psychosocial factors associated with LBP in a non-clinical sample
Self-constructed questionnaire yet to be validated |
| Rees et al (20)
Australia |
Cross sectional
Control group: no back or neck pain |
Not provided |
|
Independent variable (YSR of CBCL[27])
Dependent variable
|
Sex | Revealed significant associations between internalising and externalising behaviours with back pain
Significantly higher correlation between withdrawn scale and back pain was found in the females compared to males |
| Hoftun et al (15)
Norway |
Cross sectional |
|
|
Outcome measure: chronic pain ≥3months
Exposure measure: |
|
Aim was to explore the association between chronic pain, and lifestyle and psychological factors in a large cohort of adolescents from the community |
| Ruehlman et al (11)
United States |
Cross sectional |
|
Part 1
Part 2
|
|
Not mentioned | Part 1
To validate the utility of PCP:S/EA as a screening tool for pain in young adults from the general population. Part 2 To explore differences in pain attitudes and pain beliefs (using PCP:EA) in adolescents with chronic pain according to severity of depressive symptoms |
| Wiklund et al (6) | Cross sectional |
|
|
|
Girls reported significantly higher amounts of somatic symptoms and poor mental health, which may be related to perceived stress from school |
Table 3 Studies examination activity levels and biomechanical factors
| Physical activity | Study design | Inclusion criteria | Sample | Measured variables | Adjustment | Aims |
| Handrakis et al (13)
United States |
Cross sectional
Control group: no or minimal LBP |
|
|
Control variables
Subjective outcome measures
Objective outcome measures
|
No significance difference between groups for age, BMI, blood pressure and heart rate hence no adjustments were made | To explore the difference between groups with LBP and no/minimal LBP in terms factors commonly associated with LBP and disability |
| Long et al (12)
United States |
Cross sectional
Control group: healthy adolescents (n=20) Chronic pain group (n=20) |
|
|
Self-reported measures
Physical activity (actigraphy over 7 days)
|
No significance difference in age, gender, ethnicity between the two groups hence no adjustments were made | Compare physical activity levels between adolescents with chronic pain and healthy adolescents
Investigate the relationship between actigraphy and subjective measures of activity limitation |
| Stommen et al (17)
Netherlands |
Cross sectional case control
Control: healthy adolescents (n=42) Non-specific MSK[35] pain (n=42) |
|
|
|
Not mentioned | To compared physical activity levels between young adults with chronic pain and healthy participants |
Table 4 Studies exploring the psychosocial variables associated with pain
| Psychosocial | Study design | Inclusion criteria | Sample | Measured variables | Adjustment
|
Aims |
| Simons et al (23)
United States |
Cross sectional
No control group |
|
|
|
Duration of pain | Aim was to validate the fear avoidance model (FAM) in the paediatric population |
| Hulsebusch et al (26)
Germany |
Cross sectional |
|
|
|
Not mentioned | Test the cognitive mediation hypothesis in a sample of participants with acute/subacute pain |
| Wallace et al (58)
United States |
Cross sectional |
|
|
CPAQ-A
Pain characteristics
Disability
Depression
Anxiety
Pain self-efficacy
|
Not mentioned | Validate the CPAQ-A in adolescents with chronic pain |
| Weiss et al (30)
United States |
Cross sectional
No control group |
|
|
|
|
Examine the impact of changes in pain acceptance on pain catastrophizing, depression and disability |
| Forgeron et al (59)
Canada |
Cross sectional
Control group: healthy adolescents (n=62) Chronic pain group (n=45) |
|
|
|
|
Compare social information processing between adolescents with and without chronic pain |
| Eccleston et al (35)
United Kingdom |
Cross sectional
No control group |
|
|
|
|
Aim is to compared subjective views of social development among adolescents with and without chronic pain |
| Saariaho et al (44)
Finland |
Cross sectional
Control: non alexithymic |
|
|
|
Not mentioned | Aim was to examine differences in pain disability and depression in chronic pain patients with and without alexithymia |
| Shibata et al (39)
Japan |
Cross sectional
Control group: no pain Acute pain group Chronic pain group |
|
|
|
Demographic variables
|
Aim was to evaluate the association of alexithymia with pain intensity, disability, distress and life satisfaction in a non-clinical sample |
| Stickley et al (40)
Japan |
Cross sectional |
|
|
|
|
Investigate the association between childhood adversities (CAs) and chronic pain |
| Scott et al (37)
United States |
Multinational cross sectional survey involving 10 countries |
|
|
Face to face interviews
|
|
Examine the association between chronic physical conditions, and childhood adversities and early onset mental health disorders |
Table 5 Studies examining the association of sleep disturbance with pain and depression
| Sleep | Study design | Inclusion criteria | Sample | Measured variables | Adjustment | Aims |
| Kanstrup et al (16)
Sweden |
Cross sectional
No control group |
|
|
|
|
Investigate the association between sleep, pain and depression |
| Graham et al
United States |
Cross sectional
Control group Chronic pain group ≥3-6 months |
|
|
Biological factors
Psychosocial factors
Behavioural factors
|
|
Explore the bio-behavioural factors influencing sleep in young adults with chronic pain |
| Palermo et al (2007) (49)
United States |
Cross sectional
Control group (n=20) Controls were sex and age matched within 6months Chronic pain (n=20) |
|
|
|
Not mentioned | Compare sleep among adolescents with and without chronic pain using objective and subjective measures |
| Palermo et al (2012) (2)
United States |
1-year Longitudinal study
Control group (n=61): no serious chronic illness Chronic pain group (n=60) |
|
|
|
|
Assess differences in insomnia symptoms and risk factors for insomnia among adolescents with and without chronic pain |
| Bonvanie et al (19)
Netherlands |
3-year Longitudinal study
Cross sectional (baseline) Categories
|
|
Baseline
Follow up
Non clinical sample |
|
|
Explore the factors that mediate the relationship between pain and sleep disturbance |
| Tham et al (51)
United States |
1-year Longitudinal study
Control group (n=60) Chronic pain group (n=61) Depressive group (n=51) |
General
Chronic pain
Depressive group
Healthy group
|
|
|
Not mentioned | Investigate what contributes to fatigue in chronic pain adolescents |
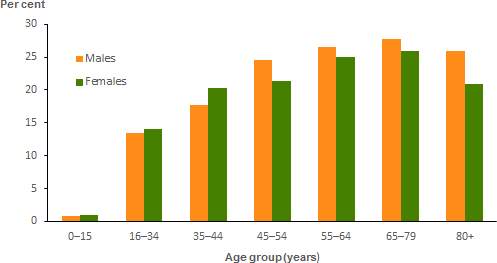
Figure 2 Source: AIHW analysis of ABS Microdata: National Health Survey, 2014–15
(http://www.aihw.gov.au/back-problems/prevalence/)
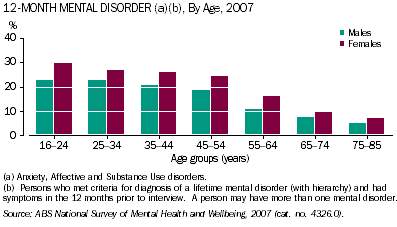
Figure 3 Prevalence of mental disorders across age groups
Taken from Australian Bureau of Statistics webpage
(http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4125.0main+features3150Jan%202013
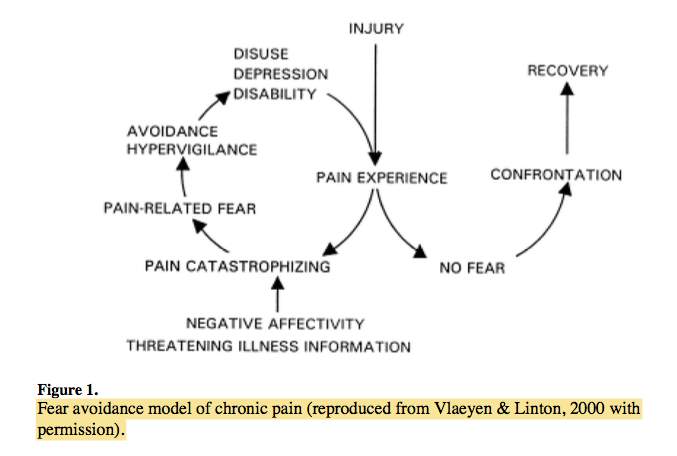
Figure 4 Original version of fear avoidance model
Ownership Vlaeyen & Linton 2000 (25)
Taken from Simons et al 2012 (23)
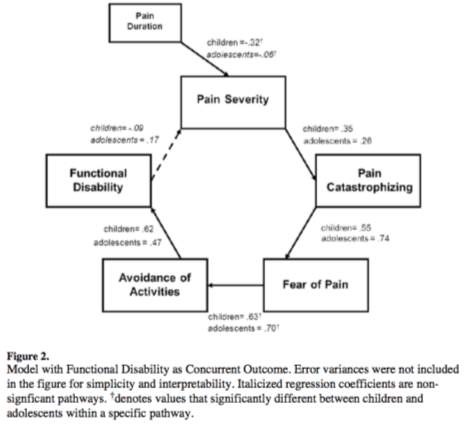
Figure 5 Modified Fear avoidance model predicting depression in paediatric population Taken from Simons et al 2012 (23) |
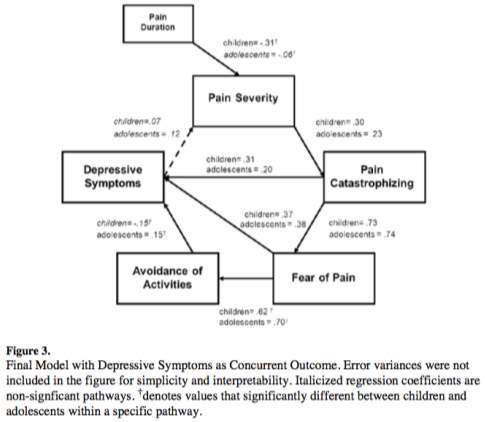
Figure 6 Fear avoidance model predicting disability in paediatric population Taken from Simons et al 2012 (23) |
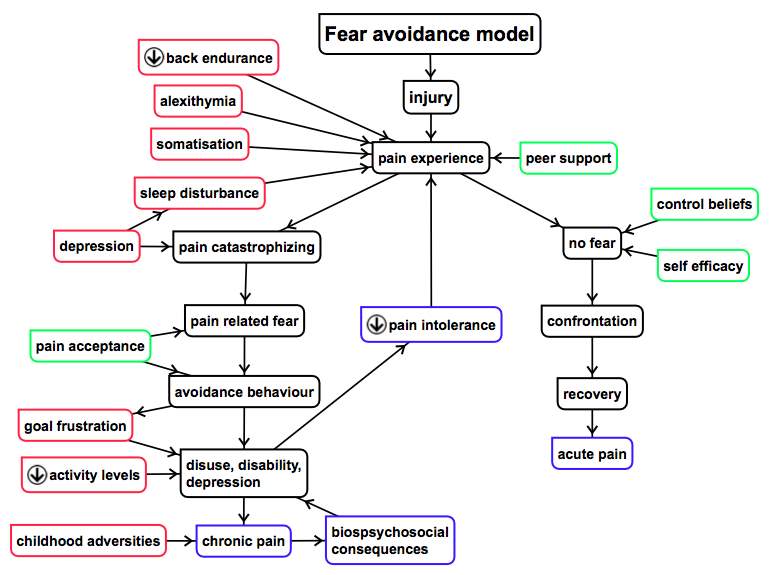
Figure 7 Psychological factors impacting the Fear Avoidance Model (reproduced from Vlaeyen & Linton, 2000)(25)
Coloured boxes are author’s addition whereby red represents a risk factor, green is a protective factor, blue are consequences
Bibliography
1. National Health Survey: First Results, 2014-15 Canberra Australian Bureau of Statistics; 2015 [updated 22/03/2016. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by Subject/4364.0.55.001~2014-15~Main Features~Psychological distress~16.
2. Palermo TM, Law E, Churchill SS, Walker A. Longitudinal course and impact of insomnia symptoms in adolescents with and without chronic pain. The journal of pain : official journal of the American Pain Society. 2012;13(11):1099-106.
3. Beales DJ, Smith AJ, O’Sullivan PB, Straker LM. Low back pain and comorbidity clusters at 17 years of age: a cross-sectional examination of health-related quality of life and specific low back pain impacts. The Journal Of Adolescent Health: Official Publication Of The Society For Adolescent Medicine. 2012;50(5):509-16.
4. Korovessis P, Repantis T, Baikousis A. Factors affecting low back pain in adolescents. Journal of spinal disorders & techniques. 2010;23(8):513-20.
5. Taloyan M, Lofvander M. Depression and gender differences among younger immigrant patients on sick leave due to chronic back pain: a primary care study. Primary health care research & development. 2014;15(1):5-14.
6. Wiklund M, Malmgren-Olsson E-B, Öhman A, Bergström E, Fjellman-Wiklund A. Subjective health complaints in older adolescents are related to perceived stress, anxiety and gender–a cross-sectional school study in Northern Sweden. BMC public health. 2012;12(1):993.
7. Who gets back problems? : Australian Institute of Health and Welfare; 2016 [Available from: http://www.aihw.gov.au/back-problems/prevalence/.
8. Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. European journal of pain (London, England). 2004;8(3):187-99.
9. Back pain and problems: Australian Institute of Health and Welfare 2016 [Available from: http://www.aihw.gov.au/back-problems/.
10. Holley A, Law E, Zhou C, Murphy L, Clarke G, Palermo T. Reciprocal longitudinal associations between pain and depressive symptoms in adolescents. European Journal of Pain. 2013;17(7):1058-67.
11. Ruehlman LS, Karoly P, Pugliese J. Psychosocial correlates of chronic pain and depression in young adults: further evidence of the utility of the Profile of Chronic Pain: Screen (PCP: S) and the Profile of Chronic Pain: Extended Assessment (PCP: EA) battery. Pain medicine (Malden, Mass). 2010;11(10):1546-53.
12. Long AC, Palermo TM, Manees AM. Brief report: using actigraphy to compare physical activity levels in adolescents with chronic pain and healthy adolescents. Journal of pediatric psychology. 2008;33(6):660-5.
13. Handrakis JP, Friel K, Hoeffner F, Akinkunle O, Genova V, Isakov E, et al. Key Characteristics of Low Back Pain and Disability in College-Aged Adults: A Pilot Study. Archives of Physical Medicine & Rehabilitation. 2012;93(7):1217-24.
14. Larsson B, Sund AM. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: Influences of pain characteristics. European Journal of Pain. 2007;11:57-65.
15. Hoftun GB, Romundstad PR, Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the Young-HUNT Study 2008. The journal of pain : official journal of the American Pain Society. 2012;13(9):874-83.
16. Kanstrup M, Holmstrom L, Ringstrom R, Wicksell RK. Insomnia in paediatric chronic pain and its impact on depression and functional disability. European journal of pain (London, England). 2014;18(8):1094-102.
17. Stommen NC, Verbunt JA, Gorter SL, Goossens ME. Physical activity and disability among adolescents and young adults with non-specific musculoskeletal pain. Disability and rehabilitation. 2012;34(17):1438-43.
18. Stommen NC, Verbunt JA, Goossens ME. Future goals of adolescents and young adults with chronic musculoskeletal pain. European journal of pain (London, England). 2016;20(4):564-72.
19. Bonvanie IJ, Oldehinkel AJ, Rosmalen JG, Janssens KA. Sleep problems and pain: a longitudinal cohort study in emerging adults. Pain. 2016;157(4):957-63.
20. Rees CS, Smith AJ, O’Sullivan PB, Kendall GE, Straker LM. Back and neck pain are related to mental health problems in adolescence. BMC public health. 2011;11:382.
21. Statistics ABo. Mental Health Canberra2013 [Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4125.0main+features3150Jan 2013.
22. Simons LE, Elman I, Borsook D. Psychological processing in chronic pain: a neural systems approach. Neuroscience & Biobehavioral Reviews. 2014;39:61-78.
23. Simons LE, Kaczynski KJ. The Fear Avoidance model of chronic pain: examination for pediatric application. The journal of pain : official journal of the American Pain Society. 2012;13(9):827-35.
24. Dr Michael Nicholas DAM, Lois Tonkin, Lee Beeston. Manage your pain. 3rd ed. Australia Harper Collins Publishers; 2011. 256 p.
25. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-32.
26. Hulsebusch J, Hasenbring MI, Rusu AC. Understanding pain and depression in back pain: The role of catastrophizing, help-/hopelessness, and thought suppression as potential mediators. International journal of behavioral medicine. 2016;23(3):251-9.
27. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour research and therapy. 2006(1):1.
28. McCracken LM, Gauntlett‐Gilbert J, Eccleston C. Acceptance of pain in adolescents with chronic pain: Validation of an adapted assessment instrument and preliminary correlation analyses. European Journal of Pain. 2010;14(3):316-20.
29. Wicksell RK, Olsson GL, Hayes SC. Mediators of change in Acceptance and Commitment Therapy for pediatric chronic pain. Pain. 2011;152:2792-801.
30. Weiss KE, Hahn A, Wallace DP, Biggs B, Bruce BK, Harrison TE. Acceptance of pain: associations with depression, catastrophizing, and functional disability among children and adolescents in an interdisciplinary chronic pain rehabilitation program. Journal of pediatric psychology. 2013;38(7):756-65.
31. Serge M, Djéa S, Isabelle G. Mental health and Pain: Somatic and Psychiatric Components of Pain in Mental Health Paris Springer; 2014. 307 p.
32. Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 1995;7(4):524-32.
33. Macedo RB, Coelho-e-Silva MJ, Sousa NF, Valente-dos-Santos J, Machado-Rodrigues AM, Cumming SP, et al. Quality of life, school backpack weight, and nonspecific low back pain in children and adolescents. Jornal de pediatria. 2015;91(3):263-9.
34. Vowles KE, Jordan A, Eccleston C. Toward a taxonomy of adolescents with chronic pain: exploratory cluster and discriminant analyses of the bath adolescent pain questionnaire. European journal of pain (London, England). 2010;14(2):214-21.
35. Eccleston C, Wastell S, Crombez G, Jordan A. Adolescent social development and chronic pain. European journal of pain (London, England). 2008;12(6):765-74.
36. Simons LE, Smith A, Ibagon C, Coakley R, Logan DE, Schechter N, et al. Pediatric Pain Screening Tool: rapid identification of risk in youth with pain complaints. Pain. 2015;156(8):1511-8.
37. Scott KM, Korff MV, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Archives of General Psychiatry. 2011(7):838.
38. Goldberg RT, Pachas WN, Keith D. Relationship between traumatic events in childhood and chronic pain. Disability and rehabilitation. 1999;21(1):23-30.
39. Shibata M, Ninomiya T, Jensen MP, Anno K, Yonemoto K, Makino S, et al. Alexithymia is associated with greater risk of chronic pain and negative affect and with lower life satisfaction in a general population: the Hisayama Study. PloS one. 2014;9(3):e90984.
40. Stickley A, Koyanagi A, Kawakami N. Childhood adversities and adult-onset chronic pain: Results from the World Mental Health Survey, Japan. European journal of pain (London, England). 2015;19(10):1418-27.
41. Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal Of Psychiatry: The Journal Of Mental Science. 2010;197(5):378-85.
42. Kooiman CG, van Rees Vellinga S, Spinhoven P, Draijer N, Trijsburg RW, Rooijmans HGM. Childhood adversities as risk factors for alexithymia and other aspects of affect dysregulation in adulthood. Psychotherapy and psychosomatics. 2004;73(2):107-16.
43. Goleman D. Emotional Intelligence. London: Bloomsbury; 1996. 352 p.
44. Saariaho AS, Saariaho TH, Mattila AK, Karukivi MR, Joukamaa MI. Alexithymia and depression in a chronic pain patient sample. General hospital psychiatry. 2013;35(3):239-45.
45. Pecukonis EV. Physical self-efficacy and alexithymia in women with chronic intractable back pain. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2009;10(3):116-23.
46. Association AP. Diagnostic and statistical manual of mental disorders: DSM-5 / American Psychiatric Association, task force chair David J. Kupfer. 5th ed2013. 947 p.
47. Zeng F, Sun X, Yang B, Fu X. Life events, anxiety, social support, personality, and alexithymia in female patients with chronic pain: A path analysis. Asia-Pacific psychiatry : official journal of the Pacific Rim College of Psychiatrists. 2016;8(1):44-50.
48. Honkalampi K, Hintikka J, Saarinen P, Lehtonen J, Viinamäki H. Is alexithymia a permanent feature in depressed patients? Results from a 6-month follow-up study. Psychotherapy and psychosomatics. 2000;69(6):303-8.
49. Palermo TM, Toliver-Sokol M, Fonareva I, Koh JL. Objective and subjective assessment of sleep in adolescents with chronic pain compared to healthy adolescents. The Clinical journal of pain. 2007;23(9):812-20.
50. Graham JE, Streitel KL. Sleep quality and acute pain severity among young adults with and without chronic pain: the role of biobehavioral factors. Journal of behavioral medicine. 2010;33(5):335-45.
51. Tham SW, Holley AL, Zhou C, Clarke GN, Palermo TM. Longitudinal course and risk factors for fatigue in adolescents: the mediating role of sleep disturbances. Journal of pediatric psychology. 2013;38(10):1070-80.
52. Lautenbacher S, Kundermann B, Krieg J-C. Sleep deprivation and pain perception. Sleep Medicine Reviews. 2006;10(5):357-69.
53. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The Biopsychosocial Approach to Chronic Pain: Scientific Advances and Future Directions. Psychological Bulletin. 2007;133(4):581-624.
54. Richardson LP, Russo JE, Katon W, McCarty CA, DeVries A, Edlund MJ, et al. Mental health disorders and long-term opioid use among adolescents and young adults with chronic pain. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2012;50(6):553-8.
55. Moore JT, Kelz MB. Opiates, Sleep, and PainThe Adenosinergic Link. The Journal of the American Society of Anesthesiologists. 2009;111(6):1175-6.
56. Morasco BJ, O’Hearn D, Turk DC, Dobscha SK. Associations Between Prescription Opioid Use and Sleep Impairment among Veterans with Chronic Pain. Pain Medicine. 2014;15(11):1902-10.
57. Robertson J, Purple R, Cole P, Zaiwalla Z, Wulff K, Pattinson K. Sleep disturbance in patients taking opioid medication for chronic back pain. Anaesthesia. 2016;71(11):1296-307.
58. Wallace DP, Harbeck-Weber C, Whiteside SP, Harrison TE. Adolescent acceptance of pain: confirmatory factor analysis and further validation of the chronic pain acceptance questionnaire, adolescent version. The journal of pain : official journal of the American Pain Society. 2011;12(5):591-9.
59. Forgeron PA, McGrath P, Stevens B, Evans J, Dick B, Finley GA, et al. Social information processing in adolescents with chronic pain: my friends don’t really understand me. Pain. 2011;152(12):2773-80.
Endnotes
[1] LBP is defined as pain in the lower back region, pain into the buttock region and/or pain radiating down the back of the leg
[2] Disability is used in the review encompasses both activity limitations and participation restriction with regards to school, home, social life, leisure activities (WHO)
[3] Chronic pain is defined as any pain regardless of site that is persisting beyond 3-6months. Some studies have used 3 months as the cut off for chronic pain, while others have used 6 months
[4] MOR Multimodal Odds Ratio
[5] Disability is used in the review encompasses both activity limitations and participation restriction due to pain in physical (daily activities, exercise) and social (school, work, leisure) domains of life
[6] Pain severity includes pain intensity and pain frequency
[7] Catastrophizing is currently defined as: “an exaggerated negative mental set brought to bear during actual or anticipated painful experience” (Sullivan et al., 2001)
[8] pain severity in this review will refer to pain intensity and frequency
[9] “Social desirability” may lead to under reporting of psychological distress among the children and adolescents, because children and adolescents tend to down-play their psychological symptoms as it is seen as a more favourable response by others (Logan et al 2008)
[10] The Pain Catastrophizing Scale assesses three components of catastrophizing, namely, rumination (“I can’t stop thinking about how much it hurts”), magnification (“I worry that something serious may happen”), and helplessness (“It’s awful and I feel that it overwhelms me”) – Sullivan et al 1995
[11] PCP:EA Profile of Chronic Pain: Extended Assessment contains 13 multi-item subscales addressing aspects of coping, positive and negative social responses, catastrophizing, and pain attitudes and beliefs (Ruehlman et al)
[12] Alexithymia is characterised by “difficulties in identifying and describing feelings, externally oriented thinking, and lack of imagination and fantasies” (Saariaho et al)
[13] TAS-20 Toronto Alexithymia Scale contains 3 subscales “difficulty identifying feelings”, “difficulty describing feelings” and “externally orientated thinking” (Shibata et al)
[14] Life satisfaction was assessed with a 100mm VAS rather than a valid questionnaire
[15] Sleep disturbance is the presence of insomnia symptoms and/or reduced sleep quality
[16] Sleep quality: includes “subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction”
[17] Musculoskeletal pain includes back, neck, shoulder, arms, legs
[18] pubertal development, depressive symptoms, sleep hygiene, cognitive and somatic pre sleep arousal, and pain intensity
[19] MDD Major depressive disorder
[20] NOS Not otherwise specified
[21] CES-D Centre for Epidemiologic Studies Depression Scale
[22] NRS Numerical Rating Scale
[23] Non-participants at T2 were characterised by having higher levels of depressive symptom level and more often had a non-Norwegian background
[24] MFQ Moods and Feelings Questionnaire
[25] SES socioeconomic status
[26] VAS visual analogue scale
[27] CBCL Child Behaviour Checklist
[28] HUNT The Nord-Trondelag Health Study
[29] WHO World Health Organisation
[30] SCL-5 5-item version of Symptom Checklist
[31] DASS-21 Depression, Anxiety and Stress Scale
[32] MDT Multidisciplinary Team
[33] CALI Child Activity Limitations Interview
[34] RCADS Revised Child Anxiety and Depression Scale
[35] MSK Musculoskeletal
[36] SQUASH Short Questionnaire to Assess Health-enhancing physical activity
[37] SCAS Spence Children’s Anxiety scale
[38] CSES Children’s self-efficacy scale
[39] PedMIDAS Paediatric Migraine Disability Assessment Scale
[40] CASAFS Child and Adolescent Social and Adaptive Functioning Scale
[41] CAM Complimentary Alternative Medicine
[42] ASR Adult Self Report (Anxious/Depressed scale)
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medicine"
The area of Medicine focuses on the healing of patients, including diagnosing and treating them, as well as the prevention of disease. Medicine is an essential science, looking to combat health issues and improve overall well-being.
Related Articles
DMCA / Removal Request
If you are the original writer of this literature review and no longer wish to have your work published on the UKDiss.com website then please:




