Spina Bifida and the Development Stage
Info: 9528 words (38 pages) Dissertation
Published: 13th Dec 2019
Contents
Occurrences of Neural Tube Defects:
The occurrences of Neural Tube Defects to uncomplicated gestations:
Graph two: Neural tube defects by live births, stillbirths, neonatal deaths, and terminations
Symptoms that occur with Neural Tube Defects:
Raw and Analysed Data four: (5)
Different Causes and Preventative Methods of Spina Bifida
Neural Tube Defects
Birth defects affect 1 in 50 infants (1) and are the main cause of babies under the age of one dying. The most common Neural Tube Defects (NTD) in humans are myelomeningocele – most serious form of Spina Bifida and anencephaly – the absence of a major part of the brain, skull, and scalp. Neural Tube Defects have no defined cause however there are several factors which increases the risk both environmental and genetic – this will be considered further within my investigation.
Neurulation
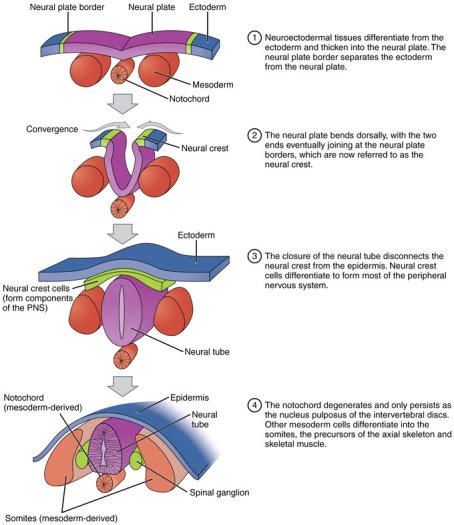 The formation of the neural tube (Neurulation) is a vital morphogenetic occurrence in embryo development. The central nervous system (CNS) is formed when the neural tube produces the brain and the spinal cord. (2) Neurulation in embryos has two phases; the primary and secondary neurulation. Both phases occur in specific areas of the rostro-caudal (head to tail) axis of the embryo. The secondary phase is limited to a specific area – the tail bud (does not develop in humans), which is located beyond the posterior (caudal) end of the embryos developing end of the neural tube. Secondary neurulation occurs by the excess of stem cells. Rod-like condensations forms from this and results in rapidly forming and vapor pockets collapsing (cavitates). The rod transforms into a tube because of the cavitation, the lumen of this tube connects with the lumen of the developing tube of primary neurulation. Secondary neurulation appears to not be responsible for open NTD, however primary neurulation is. The primary neurulation forms the brain and spinal cord. After the development of the notochord it stimulates neurulation in the ectoderm. The neural groove is formed when the neural plate folds’ outwards. The beginnings within the future neck area, the neural folds of this groove closing create the neural tube. The basal plate is the anterior part of the neural tube and the alar plate is the posterior part. The neural canal is the hollow interior and after week four of gestation, the open ends of the neurospores – neural tube closes off. See figure 1. (3).
The formation of the neural tube (Neurulation) is a vital morphogenetic occurrence in embryo development. The central nervous system (CNS) is formed when the neural tube produces the brain and the spinal cord. (2) Neurulation in embryos has two phases; the primary and secondary neurulation. Both phases occur in specific areas of the rostro-caudal (head to tail) axis of the embryo. The secondary phase is limited to a specific area – the tail bud (does not develop in humans), which is located beyond the posterior (caudal) end of the embryos developing end of the neural tube. Secondary neurulation occurs by the excess of stem cells. Rod-like condensations forms from this and results in rapidly forming and vapor pockets collapsing (cavitates). The rod transforms into a tube because of the cavitation, the lumen of this tube connects with the lumen of the developing tube of primary neurulation. Secondary neurulation appears to not be responsible for open NTD, however primary neurulation is. The primary neurulation forms the brain and spinal cord. After the development of the notochord it stimulates neurulation in the ectoderm. The neural groove is formed when the neural plate folds’ outwards. The beginnings within the future neck area, the neural folds of this groove closing create the neural tube. The basal plate is the anterior part of the neural tube and the alar plate is the posterior part. The neural canal is the hollow interior and after week four of gestation, the open ends of the neurospores – neural tube closes off. See figure 1. (3).
Figure 1: Neurulation (3)
Spina Bifida
Spina Bifida is a neural tube defect. In the first trimester of a pregnancy the embryo develops an incomplete closure of one or more vertebral arches of the spine. This overall results in the malformations of the spinal cord. This results in the spinal cord being vulnerable to infection or injury. In the UK, Spina Bifida occurs 1 in every 200 births (0.5%). (4) When an infant is born with Spina Bifida, a lifetime of problems may occur. One being paralysis, depending on where the malformation of the spinal column has occurred and which nerves had been affected. Also, many infants suffer from bowel and urinary dysfunction. The causes and preventative methods will be discussed further in this investigation.
Occurrences of Neural Tube Defects:
Neural tube defects are a main group of severe congenital anomalies that are related to long-term disability, mortality, and morbidity. Every year, there is around 5000 embryos affected by NTD in Europe (5). NTD are mostly diagnosed prenatally and the most common outcome for the foetus is termination – at 80%.
The occurrences of Neural Tube Defects to uncomplicated gestations:
Raw Data one:
Table one: “Total and live birth prevalence of neutral tube defects in study population, European Surveillance of Congenital Anomalies (EUROCAT), 1991-2011” (5)
This table shows the prevalence of neural tube defects of all the European countries. For this investigation, the table was simplified to the UK and analysed the results.
| Place | Time period | Total births | Total live births | Neural tube defects | Anencephaly | Spina bifida | |||
| No | Prevalence per 10 000 births | No | Prevalence per 10 000 births | No | Prevalence per 10 000 births | ||||
| Ireland, Cork and Kerry | 1996-2010 | 131 168 | 130 443 | 159 | 12.13 | 65 | 4.96 | 83 | 6.33 |
| Ireland, Dublin | 1991-2011 | 470 231 | 467 901 | 411 | 8.74 | 149 | 3.17 | 201 | 4.28 |
| Ireland, south east | 1997-2011 | 101 348 | 101 269 | 97 | 9.58 | 30 | 2.96 | 63 | 6.22 |
| United Kingdom, East Midlands and South Yorkshire | 1998-2011 | 922 288 | 916 786 | 1012 | 10.97 | 426 | 4.62 | 480 | 5.21 |
| UK, northern England | 2000-2011 | 382 973 | 380 843 | 522 | 13.63 | 214 | 5.59 | 251 | 6.56 |
| UK, Thames Valley | 1991-2011 | 291 827 | 290 307 | 337 | 11.55 | 155 | 5.31 | 156 | 5.35 |
| UK, Wales | 1998-2011 | 466 358 | 463 941 | 703 | 15.08 | 278 | 5.96 | 330 | 7.08 |
| UK, Wessex | 1994-2011 | 492 629 | 490 436 | 598 | 12.14 | 288 | 5.85 | 249 | 5.06 |
Table two: Total and live birth prevalence of neural tube defects in study population, UK, 1991-2011. Simplified version of the above table. (5)
Analysed Data one:
| Place | Time Period | Total Births | Total live births | Still Births
|
Neural Tube Defects | |
| No | Prevalence per 10000 births | |||||
| Ireland, Dublin | 1991-2011 | 470231 | 467901 | 2330 | 411 | 8.74 |
| United Kingdom, East Midlands and south Yorkshire | 1998-2011 | 922 288 | 916 786 | 5502 | 1012 | 10.97 |
| United Kingdom, Northern England | 2000-2011 | 382 973 | 380 843 | 2130 | 522 | 13.63 |
| United Kingdom, Thames Valley | 1991-2011 | 291 827 | 290 307 | 1520 | 337 | 11.55 |
| United Kingdom, Wales | 1998-2011 | 466 358 | 463 941 | 2417 | 703 | 15.08 |
| TOTAL | 2533677 | 2519778 | 13899 | 2985 | 59.97 | |
Out of the total births of 2533677 the number of infants born with neural tube defects was 2985 (total number of neural tube defects in the UK over a 20 year period) with the prevalence of neural tube defects per 10000 births 59.97. In the United Kingdom, East Midlands and south Yorkshire had the highest number of infants born with neural tube defects of 1012 and the prevalence of 10.97, this could be explained by the higher number of total 922288 and live 916786 births. However out of all the places analysed Wales had the highest prevalence per 10000 births being 15.08. The occurrence of neural tube defects to an uncomplicated gestation is 11.78% (see figure 2 for calculation). The occurrence of neural tube defects of total live births of an uncomplicated gestation is 11.84%. Therefore, the occurrence of neural tube defects to an uncomplicated gestation is that it occurs 11.84%, suggesting the occurrence on neural tube defects is unlikely to occur to an uncomplicated gestation. The different time periods do not affect the prevalence in use.
Figure 2: Calculations
Total Births:
Percentage=Total number of Neural Tube DefectsTotal Number of Births
Percentage=29852533677×10000
=11.78% occurrence of neural tube defects of total births.
Total live Births:
Percentage= Total Number of Neural Tube DefectsTotal number of Live Births
Percentage= 29852513778×10000
=11.84% occurrence of neural tube defects of total live births.
Raw Data two: (6)
As stated previously, it was found that Wales had a higher rate of NTD occurring and a higher number of still births the common cause is the diet and lack of folic acid. The pictorial representation below shows the neural tube defects gross case rate by local authority in Wales between 1998-2013.
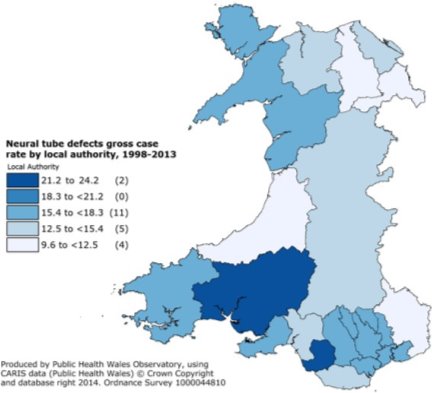
Figure 3: Neural Tube defects gross case rate by local authority – Wales, 1998-2013 (6)
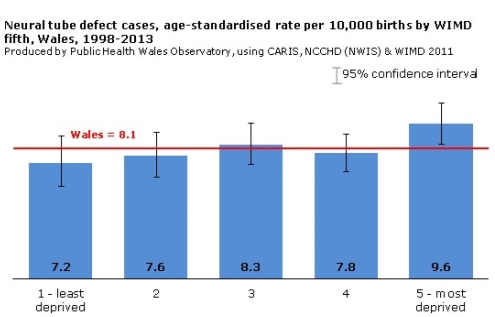
Graph one: Neural Tube Defect cases, age-standardised rate per 10,000 births by WIMD fifth, Wales, 1998-2013
| Place | Total Number of Abortions | Percentage of total number of Abortions |
| England | 177535 | 89.71% |
| Wales | 8289 | 4.19% |
| Scotland | 12082 | 6.10% |
| TOTAL | 197906 | 100% |
Table two: Abortion Statistics of 2015 in the UK (7)
Analysed Data two:
The data from Congenital Anomaly Register and Information Service (CARIS), National Community Child Health Database (NCCHD), from the National Wales Informatics Service (NWIS) indicates NTD are at a higher risk in the most deprived areas of Wales compared to that of the more affluent areas. However, the reasons for this are not clear. One factor could be a lack in variation of diet – ensuring the diet is filled with the correct vitamins and nutrition but also taking folic acid supplements before and during the first trimester of pregnancies is less in the deprived areas. It was also found according the government statistics Wales had the lowest rate of abortions of 2015 being 4.19% which could explain the reason of Wales having a higher prevalence of NTD than England as they had a higher termination rate of 89.71%.
Raw Data three:
To further the findings that the occurrence of neural tube defects to an uncomplicated gestation is very low was also the occurrence of neural tube defects in general is decreasing over a time in the UK due to better screenings, diet and general health.
Table two: “Neural tube defects by live births, stillbirths, neonatal deaths and terminations, England and Wales 1975–99”. (8) This table shows the numbers and rates of the total births, live births, still births, registered stillbirths, neonatal deaths and terminations of neural tube defects, Spina Bifida, Encephalocele and Anencephaly. I selected the data of NTD and analysed the information.
| Time period | Total | Live births | Stillbirths | Registered stillbirths | Neonatal deaths | Terminations | |
| NTD | 1975-79 | 8,106 | 4,829 | 3,249 | 3,943 | 2,388 | 751 |
| 1980-84 | 4,141 | 2,937 | 1,176 | 1,329 | 1,149 | 1,902 | |
| 1985-89 | 1,734 | 1,471 | 244 | 349 | 616 | 2,090 | |
| 1990-94 | 722 | 598 | 116 | 192 | 285 | 1,935 | |
| 1995-99 | 477 | 340 | 122 | 232 | 151 | 1,624 | |
| TOTAL | 15180 | 10175 | 4907 | 6045 | 4589 | 8302 |
Analysed Data three:
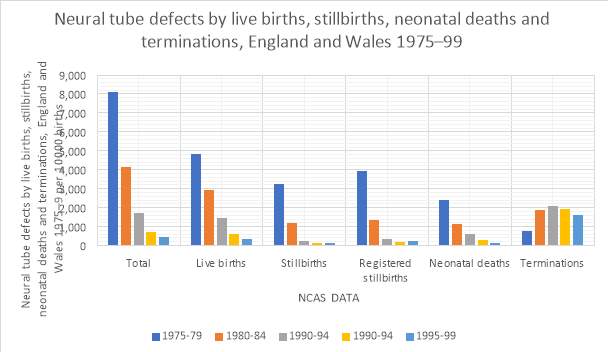 Graph two: Neural tube defects by live births, stillbirths, neonatal deaths, and terminations
Graph two: Neural tube defects by live births, stillbirths, neonatal deaths, and terminations
Between the period of 1975-1999 the total number of neural tube defects decreased by 50.26% (see figure 3 for calculation), as these numbers decreased the number of live births of foetus born with NTD had a 71.38% chance of survival, the number of still births had decreased 63.73% this could be due to more screening and critical observations of professionals. Neonatal deaths had decreased by 48.75% (see figure 4). However, the number of terminations associated with NTD had fluctuated, in 1985-89 the number of terminations was at its highest of 2,090 but then it began to decrease by 8.25% (see figure 4). Alongside this research, a survey was produced (see Appendix one) and the public expressed their opinion on the awareness of Spina Bifida and Neural tube defects. One question asked if the method of termination was offered to the mother if an abnormality was detected and 68.85% agreed with this method. (See Appendix one) So as there is a particularly high termination rate if an abnormality is detected on the 20-week antenatal scans a large percentage of mothers/families agree which may indicate the decrease in NTD infants born as they are terminated. Furthermore, a government bill regarding bread and flour fortification stated “1,000 pregnancies per year in the UK are affected by Neural Tube Defects, of which 80% are terminated.” (9) The number of stillbirths decrease over the time period however the number of terminations start to increase the two factors could be linked due to the increase in the prenatal screening. This could also suggest a reason for the decline in NTD as a large proportion of pregnancies are terminated if an abnormality is detected.
Figure 4: Calculations
Percentage decrease of total number of NTD cases:
Percentage decrease=Time period 1975-79-(1995-99)Total Number×100
Percentage decrease= 8,106-47715180×100
Percentage decrease=50.26%
Percentage of number of live births to a foetus born with NTD:
Percentage= Live births (1995-99)Total births (1995-99)
Percentage=340477 x100
Pecentage=71.38%
Percentage decrease of number of stillbirths:
Percentage decrease= Number of still births 1975-79-(1995-99)Total number of Stillbirths
Percentage decrease=3249-1224907×100
Percentage decrease=63.73%
Percentage decrease of neonatal deaths:
Percentage decrease= Number of neonatal deaths 1975-79-(1995-99)Total number of Neonatal deaths
Percentage decrease=2388-1514589×100
Percentage decrease=48.75%
Percentage decrease of terminations:
Percentage decrease= Number of terminations 1985-89-(1995-99)Total number of terminations from 1985-1999
Percentage decrease=2090-1,6245649*x100
Percentage decrease=8.25%
*5649 was the total from 1985-1999.
Symptoms that occur with Neural Tube Defects:
Prenatal Screening:
The NTD screening is performed between the 16 and 18-week gestation period, but if defects are found earlier screening can be performed as early as 15 weeks and vice versa if the defects are found later, screening can be performed as late as 23 weeks. Neural tube defect screening is not carried out within the first trimester as the maternal serum alpha-fetoprotein (AFP) levels are too low and it would be too difficult to separate between an abnormality or not. Maternal serum AFP concentration is determined and the calculations to determine the multiple of the median (MoM), this is done by dividing the patients AFP concentration with the median AFP concentration for an uncomplicated pregnancy at the specific day of gestation. Different medians are used for different ethnic groups. Depending on mother’s weight and if the mother is insulin dependent adjustments must be made; this is because blood volume changes with mother’s weight. Also, women with type 1 diabetes have a higher chance of NTD occurring than women who are not type 1 diabetes; the HbA1c levels (glycated haemoglobin) are recommended to be below 48 mmol/mol within the first trimester of the pregnancy this reduces the risk of birth defects occurring, miscarriage and stillbirth/neonatal deaths. Professionals strongly advise women who have a HbA1c level of 86 mmol/mol or above against pregnancy (10). Furthermore type 1 diabetic women have lower levels of AFP, so the lower levels of the HbA1c the greater chance of survival the foetus will have and the decreased risk of a NTD occurring. (11)
Neural Tube Defects are gradually on the decline this is because of the vigilant care of sonographers and the neural tube defects screening which help detect the neural tube defects early in the pregnancy which gives the family the option of continuing with the pregnancy or termination.
Raw and Analysed Data four: (5)
Graph three: The prevalence per 10000 live and stillbirths in the United Kingdom, Ireland, and the Rest of Europe
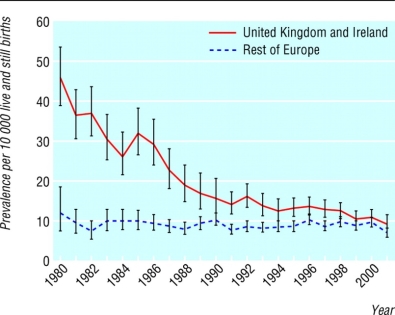
Over a 20-year period, “A total of 9 273 212 births were surveyed 16 countries 1980-2001,including 8913 babies with neural tube defects, 3298 live births, 844 stillbirths, and 4771 terminations of pregnancy after prenatal diagnosis.” (5) The United Kingdom has had an overall decrease in the number of neural tube defects prevalence per 10000 live and stillbirths. Several factors could have influenced this information. As the defect is detected early in the pregnancy terminations are offered but also the change in preventative methods offered which will be investigated further in the report. Before the 1980’s fortification was not introduced which could suggest a reason for why the United Kingdom had a higher prevalence of NTD occurring. But also the in recent years it is better reported to the NHS due to the extreme care and critical eye of professionals which could have impacted the decreased levels in the prevalence. Overall neural tube defects occurrence is decreasing which could be because of the vigilant screening and professionals.
Different Causes and Preventative Methods of Spina Bifida
A cause has not actually been stated which increases the risk of a foetus developing Spina Bifida however there are a few hypothetical causes which are said to increase the risk.
Folic Acid
The first cause and the most spoken about cause is the lack of folic acid within the first trimester of the pregnancy. Folic acid is a B vitamin which aids a female’s body to produce new healthy cells. Folic acid intake before and during the first trimester of pregnancy can reduce the risk of Spina Bifida occurring. Green vegetables, fruits and juices contain folic acid, folic is added into some cereal and bread (fortification). Most people do not digest enough food with high levels of folate so rely on a vitamin with folic acid. A female is recommended a daily dose of 400 micrograms (0.4 mg) (2) of synthetic folic acid.
Whilst collating data, a survey was produced (see Appendix one) and one question asked if anyone knew of the possible causes those who answered yes – 16.40%, 80.00% answered folic acid deficiency within the first trimester increased the risk of a foetus developing Spina Bifida. To further the findings a professional within the field of Spina Bifida was emailed (see Appendix two) stated that taking folic acid in the first few weeks of pregnancy as this is when the neural tube forms, this has greater impact. The telegraph stated “Most of these cases of NTD could be prevented through women taking folic acid supplements while trying to conceive and during early pregnancy.” (1)
Raw Data five:
To strengthen this point that taking folic acid could decrease the risk of an embryo forming Spina Bifida is a few countries have introduced cereal grains and bread have been fortified with folic acid.
Table 3: “Estimation of the number of pregnancies with a neural tube defect (NTD) that would have been prevented if folic acid fortification of flour had been implemented in 1998 in the UK” (12)
| Year of Notification | Number of pregnancies with an NTD | Proportion of women taking folic acid before pregnancy (%) | Estimated additional percentage reduction in women if folic acid fortification implemented from 1998 (%) | Number of pregnancies with an NTD that would have been prevented by folic acid fortification |
| A | B | C=(1-B/100) x23 | AxC | |
| 1998 | 936 | 39.6 | 0 | 0 |
| 1999 | 898 | 39.6 | 14 | 125 |
| 2000 | 898 | 39.6 | 14 | 125 |
| 2001 | 884 | 39.6 | 14 | 123 |
| 2002 | 915 | 35.6 | 15 | 136 |
| 2003 | 931 | 35.6 | 15 | 138 |
| 2004 | 910 | 35.6 | 15 | 135 |
| 2005 | 905 | 31.8 | 16 | 142 |
| 2006 | 931 | 31.8 | 16 | 146 |
| 2007 | 875 | 31.8 | 16 | 137 |
| 2008 | 863 | 29.9 | 16 | 139 |
| 2009 | 1019 | 29.9 | 16 | 164 |
| 2010 | 1022 | 29.9 | 16 | 165 |
| 2011 | 1034 | 27.8 | 17 | 172 |
| 2012 | 1012 | 27.8 | 17 | 168 |
| TOTAL | 14033 | 505.9 | 217 | 2014 |
Analysed Data five:
Graph four: Estimation of the number of pregnancies with a NTD that would have been prevented if folic acid fortification of flour had been implemented in 1998 in the UK.
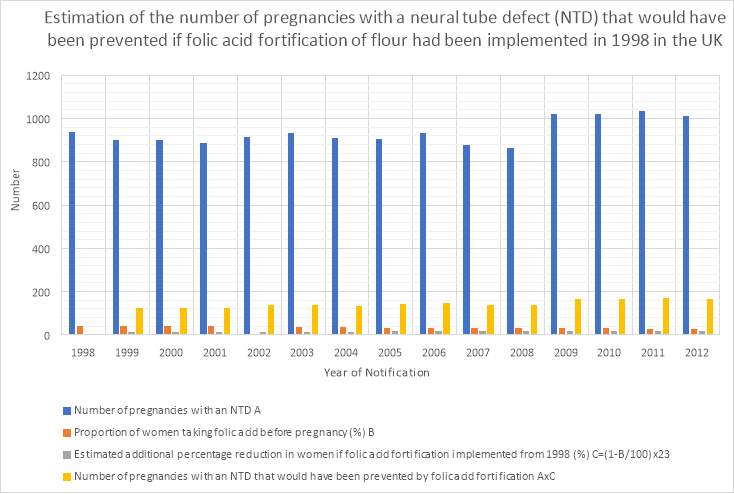 The numbers used for this graph were selected from the total number from the table above.
The numbers used for this graph were selected from the total number from the table above.
From the table a total of 2014 pregnancies could have been prevented by folic acid fortification. Out of the total number of pregnancies with a NTD only 3.61% of women were taking the recommended folic acid intake before pregnancy. Also, the number of pregnancies that would have been prevented by folic acid fortification was only 14.35%. So, whilst folic acid can decrease the risk of an embryo forming a NTD it doesn’t completely prevent the risk of it occurring.
Risk Factor of Folic acid:
Whilst taking folic acid has shown a slight decrease in an embryo forming a NTD – Spina Bifida it does have risks which individuals should be made aware of. One of the risks being the vitamin B12, it has been identified as a risk factor of NTD and works alongside folic acid. Vitamin B12 is a folic acid metabolism, if a woman has insufficient levels of the vitamin – this means the body will then not be able to metabolise folic acid sufficiently and effectively. Studies conducted by Professor Anne Molloy and the late Professor John Scott (founder of the Vitamin Research Unit at the Institute of Molecular Medicine, Trinity College Dublin), found that women which have a lower levels of the vitamin B12 could have three times more likely increase for an embryo forming NTD. The studies also revealed “60% of women may have low levels of B12.” (13) Vegetarians and vegans are at a higher risk of lower levels of B12 due to animal and dairy products being the only dietary sources of the vitamin. The B12 vitamin supplement is not yet officially recommended – the Professor Scott stated “…a daily supplement of at least 2.5mcg of B12, in addition to the recommended daily 400mcg supplement of folic acid could significantly further reduce the risk of NTD.” (13)Therefore, taking folic acid can reduce the risk of a foetus forming NTD however, if the woman has a low level of the vitamin B12 the folic acid is not being metabolised properly by the body. Whilst collating data a specialist within the field of Spina Bifida was emailed (See Appendix three) in which it was stated whilst researchers are continuously looking for the cause of NTD it always comes back to the body’s way of handling folate and related B12.
Family History
If a person in a family has a NTD – such as Spina Bifida this increases the chances of a baby being born with Spina Bifida. If a mother has previously had a child born with Spina Bifida, the risk of having other children with a NTD is significantly increased, “from less than 1 in 1,500 to around about 1 in 25.” (14) If there is a family history of Spina Bifida, the highest dosage of folic acid is prescribed by the GP before conceiving and the intake of folic acid must be taken for at least the first 13 weeks of the pregnancy. However, statistics have shown that babies born with NTD 95% have no family history of it. (15)
Medication
During a pregnancy and the mother is taking certain medications this could be linked to an increased risk of an embryo forming Spina Bifida and other birth defects. Mothers who are epileptic and/or suffer from the bipolar disorder and take the medications valproate (valproic acid) and carbamazepine – anti-seizure drug, could increase the risk of an embryo forming NTD. Researchers investigated the birth outcomes of almost 4 million babies born in Europe over a 10-year period which found “including almost 100,000 who had major birth defects and 2,680 whose mothers took carbamazepine during the first three months of their pregnancies.” (16) Whilst doctors try to avoid prescribing these medications if the woman is likely to get pregnant whilst taking them, sometimes if alternatives are ineffective these medications will need to be prescribed. If a pregnancy isn’t planned and the woman is taking any of these medications a reliable form of contraception is advised. The doctor may be able to lower the dosage of the medication and prescribe higher folic acid supplements to reduce the risks if the woman is contemplating trying for a baby but needs to take the medication.
Further evidence found was that women taking medication for epilepsy during pregnancy increased the risk of an embryo forming Spina Bifida. If Carbamazepine was taken during the first trimester of the pregnancy this increased the risk of an embryo forming Spina Bifida by 3.3% (17). However, it was also found valproic acid had an even higher risk. If a woman suffers epilepsy and no other medication is effective, she will be prescribed valproic acid. (18)
Health and Weight
Furthermore, even though there has been little research done within the area. It has been researched if the mother suffers from diabetes or obesity the chances of an embryo developing Spina Bifida is increased. If a woman is obese, there is an increased chance of a child being born with Spina Bifida this is because the body mass index (BMI) is 30 or more, a healthy BMI ranges from 18.5-24.9. If a woman has diabetes, the chance of a baby being born with Spina Bifida is also increased because it could be due to the excess glucose in the blood interfering with the embryos development. (14)
Conclusion
To conclude the occurrences of Neural Tube Defect to an uncomplicated gestation isunlikely to occur as it was investigated the occurrence of a neural tube defect to an uncomplicated gestation occurs 11.84%. Wales was also found to have higher rates of NTD occurrences in the most deprived areas. The factors explained this such as diet and folate intake.
Furthermore, Wales had the lowest termination rate compared to that of England and Scotland. If an abnormality is detected in the pregnancy many mothers and families opt for the option of termination, whilst Wales has a lower termination rate this could explain the higher numbers of NTD occurrences compared to the rest of the United Kingdom.
Through research it was investigated NTD occurrences has decreased by more than half, the survival rates have a foetus born with a NTD has greatly increased, the number of still births had decreased by 63.73% and the neonatal deaths had decreased almost by half, all of this could be explained by the vigilant sonographers and the precise prenatal screening detecting anomalies early and ensuring the correct care and help is in place to ensure the best possible outcome.
Again, terminations are still a debated topic, many pregnancies that have a birth defect end in a termination but as the years progressed the number of terminations decreased – this could be due to the more advanced medical help and the more research within the area to ease parents worry of having a child with a NTD.
The more alert care of a sonographer performs a prenatal screening if an abnormality is detected, it can be performed as early as 15 weeks and as late as 23 weeks. Depending on the mother’s ethnic group, weight and whether she is diabetic different medians are used. The neural tube defect screening is helping detect anomalies early and the occurrences of a NTD is gradually on the decline.
Folic acid deficiency is the most spoken about hypothetical cause of Spina Bifida occurring. It has shown taking the folic acid supplement of 0.4mg daily before conceiving and the first trimester of the pregnancy can reduce the risk of an embryo developing a NTD. The fortification of cereal and bread in certain countries has seen a reduction in the number of cases of Spina Bifida. However, taking folic acid does not completely prevent the risk of Spina Bifida occurring. Especially if the woman is lacking the B12 vitamin as this vitamin metabolises folic acid in the body. Professors recommend taking a 2.5mcg supplement of B12 alongside folic acid to reduce the risk even more. Whilst researchers a continuously looking for causes of Spina Bifida it always comes back to the body’s way of handling folic acid and related B12.
Depending on the family history this could increase the risk of an embryo developing Spina Bifida. The risk is further increased greatly if the mother has previously had a child born with Spina Bifida. The GP prescribes the highest dosage of folic acid before conceiving and for the first trimester if there is a family history. However, it was found very unlikely that babies born with NTD had a family history of it.
If a mother suffers from epilepsy or bipolar the medications used to treat the disorders have shown to increase the risk of NTD developing in an embryo. The medications valproate and carbamazepine can increase the risk of NTD occurring by 3%. Doctors look for alternative medications for women who are wanting to have children or who are likely to become pregnant whilst on this medication. Therefore, the medications to help treat epilepsy and bipolar could significantly increase the risk of NTD occurring, however, the GP and midwives can put preventative methods in place to help the mother.
The health and weight of a mother is also a factor which could increase the risk of a baby being born with Spina Bifida. If the mother is diabetic the excess glucose levels in the blood could interfere with the embryos development and could increase the risk of an abnormality occurring. Also, if a woman is obese the BMI is 30 or more, much higher than that of the healthy BMI – this could increase the risk of a NTD occurring.
Finally, Neural Tube Defects are on a gradual decline whether that is due to the hypothetical causes such as folic acid deficiency or medications or the mother’s health. The main reason investigated for the decline is the attentive sonographers and professionals and very precise prenatal screening which can detect an abnormality within a pregnancy and give the mother and family the option of proceeding with the pregnancy or having a termination – the most common outcome is termination which could suggest the reasoning behind the decline in NTD occurring.
Word Count: 6,989 – including all tables, headings, contents page, bibliography, and appendix’s.
Bibliography
1. One in 50 babies has a birth defect: research. Rebecca Smith, Medical Editor for the Telegraph. London : The Telegraph, 2011.
2. What is Spina Bifida? Spina Bifida Hydrocephalus Scotland. [Online] [Cited: 28 03 2017.] https://www.sbhscotland.org.uk/content/spina-bifida-what-is/.
3. Boundless. Neurulation. [Online] 16 10 31. [Cited: 20 03 2017.] https://www.boundless.com/physiology/textbooks/boundless-anatomy-and-physiology-textbook/human-development-and-pregnancy-28/third-week-of-development-263/neurulation-1296-361/.
4. Genetics, World of. Spina bifida. [Online] 2007. [Cited: 09 03 2017.] http://ic.galegroup.com/ic/scic/ReferenceDetailsPage/ReferenceDetailsWindow?failOverType=&query=&prodId=SCIC&windowstate=normal&contentModules=&display-query=&mode=view&displayGroupName=Reference&limiter=&currPage=&disableHighlighting=false&displayGroups=.
5. Long term trends in prevalence of neural tube defects in Europe: population based study. thebmj. [Online] 24 11 2015. [Cited: 20 03 2017.] http://www.bmj.com/content/351/bmj.h5949.
6. Neural Tube Defects (NTDs). Congenital Anomaly Register and Information Service. [Online] [Cited: 27 03 2017.] http://www.caris.wales.nhs.uk/central-nervous-system/.
7. Abortion statistics, England and Wales: 2015. [Online] 2015. [Cited: 28 03 2017.] https://www.gov.uk/government/statistical-data-sets/abortion-statistics-england-and-wales-2015.
8. Trends in Neural Tube Defects. Office for National Statistics. [Online] [Cited: 20 03 2017.] file:///C:/Users/geral/AppData/Local/Microsoft/Windows/INetCache/IE/3P8PU9ZH/trends-in-neural-tube-defects.pdf.
9. Bread and Flour Regulations (Folic Acid) Bill [HL] . www.parliament.uk . [Online] 08 07 2016. [Cited: 2017 03 24.] https://hansard.parliament.uk/lords/2016-07-08/debates/16070837000492/BreadAndFlourRegulations(FolicAcid)Bill(HL).
10. PREGNANCY CARE FOR WOMEN WITH DIABETES 2015. NPID. [Online] 2015. [Cited: 14 04 2017.] file:///C:/Users/geral/AppData/Local/Microsoft/Windows/INetCache/IE/EWHGQUML/Pregnancy-Care-For-Women-With-Diabetes-Summary-Report-FINAL.pdf.
11. Prenatal Screening and Diagnosis of Neural Tube Defects, Down Syndrome,and Trisomy 18. Quest Diagnostics . [Online] 01 2015. [Cited: 21 03 2017.] http://www.questdiagnostics.com/testcenter/testguide.action?dc=CF_PrenatScreen.
12. Prevention of neural tube defects in the UK: a missed opportunity. JK Morris, 1 J Rankin,2 ES Draper,3 JJ Kurinczuk,4,5 A Springett,1,5 D Tucker,6 D Wellesley,7 B Wreyford,5,8 NJ Wald1. s.l. : group.bmj.com, 2015.
13. More recent developments in NTD prevention . International Federation for Spina Bifida and Hydrocephalus. [Online] [Cited: 24 03 2017.] https://www.ifglobal.org/en/what-we-do/global-prevention/more-recent-developments-in-ntd-prevention.
14. Spina Bifida – Causes. NHS Choices. [Online] 26 02 2015. [Cited: 27 03 2017.] http://www.nhs.uk/Conditions/Spina-bifida/Pages/Causes.aspx.
15. What Causes Spina Bifida? My Child Without Limits.org. [Online] [Cited: 27 03 2017.] http://www.mychildwithoutlimits.org/understand/spina-bifida/what-causes-spina-bifida/.
16. Epilepsy Drug in Pregnancy Raises Spina Bifida Risk. WebMD. [Online] 02 12 2010. [Cited: 27 03 2017.] http://www.webmd.com/epilepsy/news/20101202/epilepsy-drug-in-pregnancy-raises-spina-bifida-risk#1.
17. Carbamazepine Linked to Increased Risk for Spina Bifida. baby Med. [Online] 27 08 2010. [Cited: 27 03 2017.] http://www.babymed.com/news/carbamazepine-linked-increased-risk-spina-bifida.
18. Valproic Acid Monotherapy in Pregnancy and Major Congenital Malformations. Jentink, J., et al. NEW ENGLAND JOURNAL OF MEDICINE : Jentink, J., Loane, M. A., Dolk, H., Barisic, I., Garne, E., de Jong-van den Berg, L. T. W., & Morris, J. K. (2010). Valproic Acid Monotherapy in Pregnancy and Major Congenital Malformations. NEW ENGLAND JOURNAL OF MEDICINE, 362(23), 2185-2193., 2010.
19. Data & Statistics. Centers for Disease Control and Prevention. [Online] 11 10 2016. [Cited: 19 03 2017.] https://www.cdc.gov/ncbddd/birthdefects/data.html.
Appendix one:
Raw Data: Analysis of Survey Results
| Are you male or female? | ||
| Male | Female | |
| Numbers | 13 | 48 |
| Percentages | 21.30% | 78.70% |
| What is your age range? | |||||
| 18>24 | 24>30 | 30>45 | 45> | OTHER | |
| Numbers | 27 | 3 | 14 | 14 | 3 |
| Percentages | 44.26% | 4.92% | 22.95% | 22.95% | 4.92% |
| Have you heard of Spina Bifida before? | |||
| Yes | No | N/A | |
| Numbers | 50 | 10 | 1 |
| Percentages | 81.96% | 16.39% | 1.64% |
| Did you know there was 4 levels of severity? | ||
| Yes | No | |
| Numbers | 9 | 52 |
| Percentages | 16.40% | 83.60% |
| Are you aware of the possible causes? | ||
| Yes | No | |
| Numbers | 51 | 10 |
| Percentages | 83.60% | 16.40% |
| What possible causes are you aware of? | ||||
| Low levels of folic acid | Genetics | Paralysis | N/A | |
| Numbers | 8 | 1 | 1 | 51 |
| Percentages | 13.11% | 1.64% | 1.64% | 83.60% |
| Would you encourage someone/would you take the recommended folic acid intake? | |||
| Yes | No | N/A | |
| Numbers | 59 | 1 | 1 |
| Percentages | 96.72% | 1.64% | 1.64% |
| Do you agree with a mother being offered a termination if an abnormality is detected? | |||
| Yes | No | N/A | |
| Numbers | 42 | 18 | 1 |
| Percentages | 68.85% | 29.51% | 1.64% |
Appendix two:
Thank you very much for your response and your information provided. I very much appreciate you taking time to respond and giving me a very in-depth response. I will be sure to let you know.
Thank you again.
Best wishes,
Dear
Thank you for your enquiry about your research. It is a fascinating area of study and full of complexities too with regards to sourcing accurate data on incidences of neural tube defects, the myriad potential causes, and the true impact of preventative measures, as I am sure you will be aware, hence it being a good choice as the need for further research is very evident!
I am not a scientist or a medic so my comments are from the perspective of a support practitioner (originally, I was an OT) rather than a medical perspective. I attended the conference of the International Federation of Spina Bifida and Hydrocephalus last year and heard several eminent research scientists debating the complexities re understanding the cause/s of Spina Bifida. The discussions understandably focussed around folate levels and the links with low folate and neural tube defects. However, there was clear debate about whether there were causes affecting absorption of folate in the first place ie. whether other biological/genetic/environmental factors may affect individual’s folate levels and their capacity to absorb folic acid + other nutrients or whether folate levels were insufficient within regular diets etc. There has certainly been a reduction in incidence of Spina Bifida since there have been direct campaigns to increase uptake periconceptually and there is evidence of reduced incidence in countries where compulsory fortification has been introduced. However, research also shows geographical clusters eg. around open coal mines in China and other areas which have prompted more research.
It is tricky to measure and establish the full impact of antenatal screening and there is thought to be a high incidence of termination in many countries including Scotland. There are variations in what information is or isn’t provided during the screening process and it is so complex due to the significant variance in Spina Bifida and the degree to which it affects people. There are some hypotheses around the impact of medical advice given at this stage as well as social/contextual influence on continuation v. termination. I am sorry that I am not entirely sure re access to records re terminations and whether neural tube defects would routinely be recorded in all cases or not. My understanding is that this may depend on what the primary diagnosis is though I would suggest that the Foetal medicine service could give more accurate information about this if you need that for your research.
From a support perspective, we reiterate to parents that although there is sound evidence that taking folic acid periconceptually can reduce the risk of Spina Bifida occurring, it is NOT the sole cause and we are very aware of many parents who have indeed taken the recommended doses but have still had a baby diagnosed with neural tube defect. It can understandably be difficult for parents to think that anything they did/didn’t do caused their child to have Spina Bifida and we reassure them that it is a much more complex picture. A challenge for preventative measures is that the protective benefits of folic acid are most effective if it is taken before conception or in the first 4-6 weeks of pregnancy when the neural tube forms. As most would be unaware of pregnancy at this stage they may often only be advised to begin taking folic acid once their pregnancy is confirmed, often after the crucial point, hence campaigns have begun to target individuals and couples of children bearing age to be aware before conceiving eg. https://www.sbhscotland.org.uk/content/are-you-getting-enough/
I hope that is of some help, and please don’t hesitate to get in touch if you want to discuss further. Also, if you would like more expert knowledge our president Margo Whiteford is also the chair of the International Federation for SBH and there may be useful information for you through them too https://www.ifglobal.org/en/who-we-are
Spina Bifida Hydrocephalus Scotland
The second email was sent to the charity SBH Scotland
Dear;
Thank you for your e-mail, which I have copied below so that I can try my best to address your questions.
We no longer have a dedicated worker in our folic acid promotion campaign, but the International Federation for Spina Bifida & Hydrocephalus may be able to provide some more informed answers to these questions (https://www.facebook.com/ifsbh/ ; https://www.facebook.com/profile.php?id=100010844671073 (Martine Austin, who used to run the Go Folic! campaign here); https://www.ifglobal.org/en/ ) and they remain very active in the area.
“Dear who it may concern,
I would greatly appreciate if someone could answer or give an opinion into some of the questions. One subject I have researched into is the causes, as there is not a proven cause folic acid deficiency is the main spoken about cause; is there any other causes that could increase the risk of an embryo forming Spina Bifida?
Also, do you think the preventative methods used in practice working are reducing the number of cases of Spina Bifida?
Finally, how much have the Spina Bifida profiles changed over the years? What support do they receive now to help them?
If you know of any published papers which could help with my research that would be greatly appreciated.
Any information would be greatly appreciated.
Researchers continue to explore possible alternative causes of neural tube defects, but everything comes back to the body’s handling of folate, whether that be focussed around MTFHR gene, risks posed by anti-folate drugs (some anti-epileptics, like valproate), or related B-vitamins (B12 and inositol). Have a look at his link: https://www.ifglobal.org/en/what-we-do/global-prevention/more-recent-developments-in-ntd-prevention There are recognised high-risk groups: https://www.ifglobal.org/en/what-we-do/global-prevention/high-risk-women
It is remarkably difficult to know whether preventative methods have made a difference to numbers of pregnancies affected by neural tube defects. Datasets are not very complete. BINOCAR /EUROCAT are the best datasets available for Europe, I think: http://www.binocar.org/eurocat There is, in the UK, a general downward trend (which may be reversing slightly) of births of children with spina bifida. However, there is also a high pregnancy termination rate – around 80% – when spina bifida myelomeningocele is identified on 20-week antenatal scans.
Whilst we as SHINE support fortification of white flour with folic acid, it is unclear whether this would provide the levels required to have a major effect on affected pregnancy figures. Indications from countries like Canada and the USA have suggested that fortification can help, though (Berry R.J., Mulinare J., Hamner H.C. Folic acid fortification: neural tube defect risk reduction—a global perspective. In: Bailey L.B., editor. Folate in Health and Disease. 2nd. CRC Press; Boca Raton, FL, USA: 2010. pp. 179–204.) Although folic acid was promoted in the early 1990s in the UK (its primary use is as a preconception supplement – its value after a few weeks of pregnancy and in unplanned pregnancies is thus very limited, in terms of neural tube defects), women now must actively ‘seek’ the information, except those who become aware of SHINE’s Go Folic! campaign or similar work.
Does this help at all? Like I say – Int’l Fed could also be a great source of information;
Appendix three:
Survey Questions:
Awareness of Spina Bifida |
Spina Bifida
My chosen subject for my graded unit is Spina Bifida. I am required to collate my own data for analysis so I have made a survey on surveymonkey.com. I am specifically looking into the awareness the public are of Spina Bifida and their opinion of the preventative methods.
Spina Bifida is a form of neural tube defects that forms abnormalities of the brain, spine and spinal cord that occurs in the early stages of a developing embryo. When the neural tube defects occur, the neural tube does not close properly forming a gap in the spinal column. Spina Bifida has 4 levels of severity, the severest causes paralysis and urine and bowel dysfunction.
Top of Form
* 1. Are you male or female?
Male
Female
Other
* 2. What is your age range?
18>24
24>30
30>45
45>
Other
* 3. Have you heard of Spina Bifida before?
Yes
No
* 4. Did you know there was 4 levels of severity?
Yes
No
* 5. There is not a defined cause of Spina Bifida but there are suggestions on what could possibly increase the chances of an embryo forming Spina Bifida, are you aware of any of the possible causes of Spina Bifida?
Yes
No
* 6. If answered yes, what possible causes do you think increases the chance of an embryo forming Spina Bifida?

* 7. Folic acid is advised to pregnant women in their first trimester of pregnancies, this is a preventative method. Would you encourage someone/or would you take the recommended folic acid intake to prevent any defects occurring during the pregnancy?
Yes
No
* 8. An abnormality can be detected antenatally (before birth) and some mothers are offered a termination, do you agree with this method?
Yes
No
* 9. Why do you agree/disagree with this method?

* 10. Do you think the public/expectant parents should be made more aware of Spina Bifida?
Yes
No
Bottom of Form
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Children"
Dissertations looking at all aspects of children, their health and wellbeing, the impact of advances in technology on childhood and more.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




