Issues Surrounding Type 2 Diabetes Mellitus in the South Asian Population in London
Info: 8301 words (33 pages) Dissertation
Published: 9th Dec 2019
Tagged: HealthPublic HealthDiabetes
Summative Assignment
Introduction
Type 2 diabetes mellitus (T2DM) is a condition characterised by insulin resistance and relative insulin deficiency, and one that has associated high morbidity and mortality (Stumvoll et al., 2005). Diabetes is a major global health problem that has experienced a persistent rise in prevalence over recent decades, affecting approximately 1 in 10 adults and accounting for almost four million deaths per annum worldwide (Zheng et al., 2017; GBD, 2015). In the UK, the overall prevalence of diabetes is estimated to be 5%, with T2DM accounting for the majority of cases, with a prevalence rate of 4.5% (Holman et al., 2015). However, these prevalence figures do not account for under-diagnosis, which has been reported to be as high as 19%, which is equivalent to more than 750,000 persons or 10% of the population (Beagley et al., 2014; Pierce et al., 2009). The prevalence of T2DM in London has been increasing at rates faster than any other region within the UK, with over 500,000 Londoners that are currently living with the condition and approximately 140,000 who remain undiagnosed (Sahota et al., 2014; Public Health England, 2015a). Moreover, it is suggested that the incidence of T2DM is going to continue to rise, and will affect a further 200 million people, globally, within the next 20 years (IDF, 2017; Zheng et al., 2017). On a local scale, in London, this equates to predictions that rates of T2DM will rise by a further 200,000 cases by the year 2025 (Sahota et al., 2014). The prevalence of T2DM according to London boroughs is shown in figure 1 (appendices). Newham has a prevalence of almost 10%, which is higher than any other region and is even predicted to remain as one of the areas with the highest diabetes prevalence for the next two decades (NHS, 2015).
This work aims to evaluate the current issues surrounding T2DM in the South Asian population in the London borough of Newham, and to suggest a strategy to improve T2DM care further.
The diverse population that resides in the capital is a significant challenge to diabetes care, due to the high prevalence of obesity, vast ethnic diversity, and socioeconomic deprivation, which as a combination, is a diabetes prone demographic (NHS, 2015). There is an abundance of ethnic communities such as South Asians (figure 2, appendices), who are at increased risk of conditions that diabetes can accelerate, including cardiovascular disease and chronic kidney disease, which are the leading causes of morbidity and mortality in such patients (NHS, 2015; Zheng et al., 2017; Beckman et al., 2013). Indeed, evidence has shown that South Asian men have double the risk of death related to cardiovascular disease, even after adjustment for cardiovascular risk factors, when compared with their European counterparts (Forouhi et al., 2006). It is reported that 40% of London’s population is comprised of Black Asian and Minority Ethnic groups, and approximately half of these are of Afro-Caribbean or South Asian descent (Sahota et al., 2014). Newham has one of the most diverse ethnic communities and up to 40% of their population is of Asian descent (figure 2, appendices), of whom, 50% are overweight or obese (Sahota et al., 2014). Moreover, Newham experiences some of the greatest socioeconomic deprivation of all London boroughs (see figure 3, appendices), which can contribute to poorer health-related outcomes (NHS, 2015). Furthermore, Londoners experience some of the highest rates of diabetes-related complications such as major amputation and chronic renal failure, of which seldomly exceeds that of the national average (NHS, 2015).
Contributing Factors
Among persons of Asian descent, aside from genetic predisposition, there are a variety of factors that contribute to the observed trajectory of chronic diseases such as that of T2DM, as well as factors that influence the development, management and prognosis of chronic disease (Khunti et al., 2009). South Asian refers to people originating from the regions of India, Pakistan, Bangladesh and Sri Lanka, and there is considerable heterogeneity among these groups, in terms of religion, culture, and lifestyle that can impact on both short- and long-term diabetes care (Stevens et al., 2006).
First-line treatment of T2DM involves lifestyle interventions, including modifications to diet and exercise, which is recommended by the National Institute for Clinical Excellence guidelines (NICE, 2015). Nutritional recommendations include a diet that is high in fibre, carbohydrates of low glycaemic index, and one that is low in fat, but contains healthy unsaturated fats, and exercise recommendations include increasing physical activity and losing weight (NICE, 2015). Indeed, the typical South Asian diet is in stark contrast to these recommendations, with higher intakes of carbohydrates and unhealthy saturated fats and minimal fruit, vegetable and fibre intake, which has been shown to increase the risk of insulin resistance and metabolic syndrome (Misra et al., 2009; Lovegrove, 2007). Although evidence regarding the effect of the South Asian diet on the incidence of diabetes is limited, there is alarming evidence that it increases the risk of cardiovascular disease and cancer (Joshi et al., 2007; Dos Santos Silva et al., 2002; Dos Santos Silva et al., 2004; Radhika et al., 2008). More recently it has been demonstrated that low fruit and vegetable intake, which is markedly prevalent in these communities, is associated with low vitamin C concentrations, which demonstrates an inverse dose-response relationship with the risk of diabetes (Ness et al., 1999; Harding et al., 2008).
Importantly, the dietary preferences of South Asian people are often very diverse, and recipes used among Asians that are detailed by nutritional studies are varied: thus, generalisations regarding the South Asian diet cannot be made (Kassam-Khamis et al., 2000; McKeigue et al., 1985). However, evidence has shown that South Asians are likely to continue their current eating practices, even in the presence of concerns that it may adversely affect their glycaemic control (Lawton et al., 2008). It is also noted that the majority of these patients viewed their diet as a source of strength, believing that avoiding the diet would result in alienation from their ethnic community and social circle (Lawton et al., 2008).
Poor physical activity with a sedentary lifestyle has been shown to be a significant risk factor in the development of both diabetes and cardiovascular disease, and indeed, studies have shown that physical activity levels among South Asian populations are low when compared with other ethnicities (Fischbacher et al., 2004; Kolt et al., 2007). Of concern, is that low physical activity and sedentary living have also been demonstrated to be significant among South Asian children, when compared with white children (Duncan et al., 2008; Khunti et al., 2007). Reasons behind a lack of engagement in physical activity among South Asians have been reported to be related to cultural norms, social expectations, time pressures and other health problems that limit functional ability (Lawton et al., 2006). Moreover, South Asian women have reported on the cultural importance of activity that is required on a daily occurrence, but this activity is not congruent with Western exercise, which is more formal and organised (Sriskantharajah and Kai, 2007). Moreover, other evidence shows that South Asian women are reluctant to exercise voluntarily, but would be more willing if they were referred to gyms or exercise programmes from Primary Care services (Khanam and Costarelli, 2008). Thus, there is some disparity in the understanding of exercise between South Asian people and Western society, that does not appear to have been addressed by Western diabetes guidelines (NICE, 2015).
Language barriers and disease education are also problematic among different ethnic groups residing in the UK, with South Asians speaking a variety of languages – some may have little understanding of English (Khunti et al., 2009). In addition, interpreters within healthcare are not widely or readily available for time-consuming discussions regarding chronic disease education, such as concern diabetes, and furthermore, religious practices can make occurrences such as appointment organisation and conversing with the opposite sex troublesome (Hawthorne, 2001). Studies among South Asian populations have shown that important aspects of diabetes education such as management of hyperglycaemia are often lacking, and both, English, and health illiteracy, can result in failure to understand information and may even lead to poorer glycaemic control (Hawthorne and Tomlinson, 1999). Moreover, there have been numerous reported difficulties in South Asian persons’ ability to access healthcare services, including those related to cardiovascular disease (Hawthorne, 1994; Lear et al., 1994). However, it is also reported that South Asians can be less willing to engage with healthcare services due to religious and fatalistic acceptance of their illness, that is often viewed as an unmodifiable punishment from God (Choudhury et al., 2008). Finally, there are also misconceptions about Western medicine among South Asians, with reports that diabetic drugs are only for symptom relief and are otherwise ineffective, and others that report they may even be harmful (Lawton et al., 2005).
In summary, there are several barriers to effective diabetes care that exist among South Asian persons and communities, which are often due to cultural and educational factors (Sriskantharajah and Kai, 2007; Lawton et al., 2006). Indeed, the Indian Diabetes Prevention Programme have shown that positive impacts can be demonstrated, with relative risk reductions of diabetes of almost 30%, when physical activity can be increased and frequently maintained, when compared with usual care (Ramachandran et al., 2006). However, although NICE suggest that medical professionals should adopt an individualised approach to diabetes care, the guideline lacks specificity in the approach to caring for high-risk populations, such as South Asian communities (NICE, 2015). One study has reported that healthcare professionals would achieve far greater patient care by learning more about South Asian culture and religion (Fagerli et al., 2005). Other studies have taken into consideration religious constraints to effective diabetes care, such as that of Ramadan, and official bodies including the International Diabetes Federation and Diabetes and Ramadan International Alliance have even produced formal guidelines on diabetes management during the fasting period (Hassanein et al., 2017). Despite this, there currently appears to be a marked inconsistency across modern Western medicine approaches to diabetes care in meeting the needs of Black Asian and Minority Ethnic groups, which is concerning given the high burden of diabetes, and other chronic diseases, within these populations, and this is indeed an area that should be of the highest priority for healthcare services and policy makers.
Policy Initiatives and Interventions
In addition to the considerable morbidity and mortality of diabetes, which is the ninth leading cause of death and third leading cause of lost disability-adjusted life years worldwide, diabetes represents a significant economic burden to the UK, that consumes more than 10% of the National Health Service (NHS) budget (Diabetes UK, 2018; GBD Collaborators, 2015). Moreover, it is reported that the majority of T2DM cases are preventable with simple lifestyle modifications, including optimisation of body weight, and dietary and exercise habits, which represent reasonable and economic treatment options (Schellenberg et al., 2013; Hu et al., 2001). In order to tackle the burden of diabetes on both a local and national scale, a broad but robust public health approach seems the most appropriate and relevant modality. The London Health Assembly report that diabetes is an emerging crisis for the NHS and requires an approach to care that includes integrated care services and joined-up policy, in order to help improve patient outcomes (Sahota et al., 2014).
Despite the existence of the discussed findings that can confound the engagement of South Asian populations with current diabetes management recommendations, there have been very few efforts made to translate this information into designing diabetes treatments and prevention programs for such ethnic groups (Khunti et al., 2009). On a more general level, the Department of Health published its National Service Framework for Diabetes (2001) in the new millennium, which set out 12 standards and important interventions that were deemed essential to improving diabetes care. These included the targeting of high-risk communities and using initiatives to help prevent diabetes, as well as improving individuals’ glycaemic control and cardiovascular risk, and screening for complications that could endanger the vision, limbs and lives of diabetic patients. Other standards included optimising the management of diabetic emergencies, and improving diabetic care among children, young people and pregnant women (Department of Health, 2001). Since its introduction, the Department of Health also established the National Diabetes Information Service and National Diabetes Audit, to help provide co-ordinated and effective diabetes information and education, and to support continuous quality improvement (Department of Health, 2010). Furthermore, the NHS Health Check programme, that was launched in 2009, is a universal initiative that was designed to assess and modify the risk of cardiovascular disease, renal disease, and diabetes, in all persons aged between 40 and 74 years (Kearney, 2017).
Furthermore, in 2008 the Department of Health launched its Healthy Weight, Healthy Lives strategy for England, which aimed to tackle the high rates of obesity and increase the ability of individuals to sustain a healthy weight, with a view to reducing the prevalence of T2DM (Department of Health, 2008). Moreover, additional initiatives included population level services such as the ‘One You’ and ‘Change4Life’ campaigns and the ‘Heart Age’ tool, which aim to encourage positive behavioural change and improve understanding of cardiovascular health. On a community level, the Department of Health recommended that integrated care is utilised to best reach high-risk and vulnerable communities, such as Black, Asian and other ethnic minority groups (Public Health England, 2018).
Outcomes
The Health and Social Care Act 2012 ensures that there is a legal obligation on service providers to offer the NHS Health Check to all eligible persons every five years (Public Health England, 2018). It is reported that were 15.5 million persons eligible for the NHS Health Check between 2013 and 2017, of which 78% were offered a check while 49% participated: that is equivalent to 5.9 million persons (Public Health England, 2018). The percentage of people accepting invitations to the NHS Health Check has demonstrated an increasing trend, which is currently reported to be 51.1%. In Newham, the statistics show a similar trend, but one that has a higher participation rate of 64.2%, which is far above the national average (NHS, 2018). Moreover, the Expert Scientific and Clinical Advisory Panel report that NHS Health Check coverage has been able to reach the highest-risk groups, including South Asian communities (Thompson et al., 2017). In a study evaluating the coverage impact of the programme within London, Robson et al. (2017) showed that coverage between 2009 to 2013 among persons in Newham increased from 34% to 42%, and by 15.7% to 25.1% in South Asian communities, but these uptake rates were lower than any other ethnicity. The results also showed that statin prescription rates increased by more than 3% as a result of health check attendance, and more comorbidities were identified and diagnosed, including diabetes, hypertension and chronic kidney disease. In Newham, the likelihood of being newly diagnosed with diabetes was significantly higher (odds ratio 1.145; 95% CI 1.037, 1.263, p=0.007), but again, it was one of the lowest among London boroughs. The authors concluded that the NHS Health Check programme shows no evidence of inequity of care provision, yet there is still limited impact upon high-risk groups such as South Asian communities (Robson et al., 2017; Robson et al., 2015). In a prior study, Robson et al. (2016) concluded that the increase in statin treatment in high cardiovascular risk groups is likely to yield important reductions in the number of cardiovascular events, but there has yet to be any meaningful outcome data.
High-quality trial data has shown meaningful and promising results for the effectiveness of diabetes prevention programs in improving outcomes, which have been evaluated in a recent systematic review (Public Health England, 2015b). The incidence of T2DM was found to be 26% (95% CI 7%, 42%) lower in the patients who attended the Diabetes Prevention Program, than in those who received normal care. In addition, the programme has been shown to improve weight, with 2.46 kg total weight loss over the 12- to 18-month follow-up period, while mean weight loss was 1.57 kg higher than non-intervention groups, but this did not reach statistical significance (p=0.64). The results regarding glycaemic control have shown little improvement from patient’s baseline. Among randomised controlled trials, fasting glucose concentrations were found to be 0.09 mmol/L lower, which was 0.06 mmol/L more than usual care, but this difference was not statistically significant. There were also no significant differences between groups for 2-hour glucose tolerance testing (p=0.52). Similarly, there were no differences between groups for glycated haemoglobin (HbA1C) concentrations, with a reduction of 0.04% (95% CI -0.07, -0.01) in the prevention group. The results also demonstrated that there were no ethnic disparities for the reported outcomes, including T2DM incidence, weight, and glycaemic parameters, but there are only a limited number of trials evaluating the impact of programs upon specific ethnic groups such as South Asians (Public Health England, 2015b).
Strategy for Further Improvement
On a local scale and individual level, nurses can adopt various strategies to help improve patients experience and diabetes care. Given that the evidence has highlighted that a proportion of South Asians are health illiterate and that disease education is fundamental to outcomes (Adams, 2010), a nursing strategy using tailored individual counselling with education seems an appropriate and realistic modality to improving care. This approach would allow nurses the time to explore the holistic and patient-centred needs of individuals such as barriers to physical exercise or medication adherence problems, can be addressed in a therapeutic way. This may help patients to better understand their illness and its management, as well as the implications of their decisions, such that individuals are better informed about their health, which may act as a catalyst to adopting more self-responsibility and healthy behaviours, that may ultimately lead to positive change and better outcomes. This may prove an effective approach for vulnerable individuals, including South Asians, who may be less likely to engage with Western medicine. Indeed, the use of tailored counselling and education has been found to improve the management and knowledge of patients with a variety of chronic diseases, as well as enhancing satisfaction levels and individual’s self-confidence and self-efficacy in managing their conditions (Bosworth et al., 2005; Murray et al., 2007; Lee et al., 2012).
In order to target high-risk populations such as South Asians on a larger scale, it appears that an alternative but complementary approach is required to improve their engagement with health services, which thus has potential to improve their health outcomes. Indeed, the London Health Assembly report that an integrated approach to care can lead to improved patient outcomes, and its effectiveness can be optimised by utilising the principles of holistic care (Sahota et al., 2014). Moreover, joining-up policy at a local level by increasing the collaboration between health and planning departments may help to tackle rates of obesity by speculating on examples such as restricting the building of fast food outlets within the proximity of schools (Sahota et al., 2014). However, in order for professionals including doctors and nurses to positively impact on patient experiences, it is important that this involves the incorporation of holism and individualised care.
Holistic and patient-centred care are approaches that aim to individualise medical care by acknowledging and addressing the patients most valued needs, whether they are medical, emotional, psychological, spiritual or religious (Gluyas, 2015). Patient-centred approaches to care offer opportunities for care providers to develop therapeutic relationships with patients, of which, help to better empower and engage individuals in developing a proactive attitude towards their health and gaining stronger self-efficacy, than compared with more conventional approaches (McMillan et al., 2013). It is reported that patient-centred care is essential to proving high-quality care in modern health systems and has been shown to improve various important outcomes, including improvements in satisfaction with care, as well as reducing hospital readmission rates and length of stay, improving management of long-term disease, reducing cost, and improving survival rates (Charmel and Frampton, 2009).
Conclusion
In summary, diabetes represents a significant public health problem and is an emerging, if not, an already present crisis of epidemic proportion. Diabetes is associated with high morbidity and mortality, which can profoundly impact on individual’s daily lives, and also has wider societal and national implications, such as reduced productivity with excess life-years lost due to health-related disability or premature death. Controlling the diabetes epidemic is a major challenge and although various government led initiatives have been introduced, the data on outcomes has found few meaningful improvements in diabetes outcomes. However, diabetes prevention programs can reduce the incidence of diabetes, and have some impact on weight and HbA1C reduction, which represent small initial steps to potential greater future improvements. In regard to high-risk communities such as those of South Asian ethnicity and the socioeconomically deprived in Newham, there is insufficient data to draw conclusions at this current time. However, in the interim and into the future, it is imperative that care providers adopt approaches to care that can engage difficult-to-access communities, in order to reduce the burden of diabetes upon such persons. This approach will rely on utilising and optimising the principles of patient-centred and holistic care during every opportunity of patient contact, which has the potential to improve morbidity and mortality not only on an individual level, but on a much larger population-level scale.
References
Adams, R. J. (2010) Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy, 3 61-72. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3270921/ [accessed 02/06/2018].
Beagley, J., Guariguata, L., Weil, C. and Motala, A. A. (2014) Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin Pract, 103 (2), 150-160. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24300018 [accessed 08/05/2018].
Beckman, J. A., Paneni, F., Cosentino, F. and Creager, M. A. (2013) Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Eur Heart J, 34 (31), 2444-2452. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23625211?dopt=Abstract&holding=npg [accessed 27/05/2018].
Bosworth, H. B., Olsen, M. K., Gentry, P., Orr, M., Dudley, T., McCant, F. and Oddone, E. Z. (2005) Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Education and Counseling, 57 (1), 5-14. Available from: http://dx.doi.org/10.1016/j.pec.2004.03.011 [accessed 02/06/2018].
Charmel, P. A. and Frampton, S. B. (2009) Putting Patients First: Best Practices in Patient-Centred Care. 2nd edition. San Francisco, CA, Planetree.
Choudhury, S. M., Brophy, S., Fareedi, M. A., Zaman, B., Ahmed, P. and Williams, D. R. R. (2008) Intervention, recruitment and evaluation challenges in the Bangladeshi community: Experience from a peer lead educational course. BMC Medical Research Methodology, 8 64-64. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2571097/ [accessed 30/05/2018].
Department of Health. (2001). National Service Framework for Diabetes: Standards [online]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198836/National_Service_Framework_for_Diabetes.pdf [accessed 29/05/2018].
Department of Health. (2008). Healthy Weight, Healthy Lives: A Cross-Government Strategy for England [online]. Available from: https://extranet.who.int/nutrition/gina/sites/default/files/GBR%202008%20Healthy%20Weight%2C%20Healthy%20Lives-%20A%20Cross-Government%20Strategy%20for%20England.pdf [accessed 29/05/2018].
Department of Health. (2010). Six Years On: Delivering the Diabetes National Service Framework [online]. Available from: http://webarchive.nationalarchives.gov.uk/20130123201230/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_112509 [accessed 29/05/2018].
Diabetes UK. (2018). Cost of diabetes [online]. Available from: https://www.diabetes.co.uk/cost-of-diabetes.html [accessed 08/05/2018].
Dos Santos Silva, I., Mangtani, P., McCormack, V., Bhakta, D., McMichael, A. J. and Sevak, L. (2004) Phyto-oestrogen Intake and Breast Cancer Risk in South Asian Women in England: Findings from a Population-based Case-Control Study. Cancer Causes & Control, 15 (8), 805-818. Available from: https://doi.org/10.1023/B:CACO.0000043431.85706.d8 [accessed 29/05/2018].
Dos Santos Silva, I., Mangtani, P., McCormack, V., Bhakta, D., Sevak, L. and McMichael, A. J. (2002) Lifelong vegetarianism and risk of breast cancer: a population-based case-control study among South Asian migrant women living in England. Int J Cancer, 99 (2), 238-244. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11979439 [accessed 28/05/2018].
Duncan, M. J., Woodfield, L., Al-Nakeeb, Y. and Nevill, A. M. (2008) Differences in physical activity levels between white and South Asian children in the United Kingdom. Pediatr Exerc Sci, 20 (3), 285-291. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18714118 [accessed 29/05/2018].
Fagerli, R. A., Lien, M. E. and Wandel, M. (2005) Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite, 45 (3), 295-304. Available from: http://www.sciencedirect.com/science/article/pii/S0195666305000814 [accessed 29/05/2018].
Fischbacher, C. M., Hunt, S. and Alexander, L. (2004) How physically active are South Asians in the United Kingdom? A literature review. Journal of Public Health, 26 (3), 250-258. Available from: http://dx.doi.org/10.1093/pubmed/fdh158 [accessed 29/05/2018].
Forouhi, N. G., Sattar, N., Tillin, T., McKeigue, P. M. and Chaturvedi, N. (2006) Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia, 49 (11), 2580-2588. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16972045?dopt=Abstract&holding=npg [accessed 26/05/2018].
GBD (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet, 385 (9963), 117-171. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4340604/ [accessed 27/05/2018].
GBD Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386 (9995), 743-800. Available from: http://dx.doi.org/10.1016/S0140-6736(15)60692-4 [accessed 08/05/2018].
Gluyas, H. (2015) Patient-centred care: improving healthcare outcomes. Nurs Stand, 30 (4), 50-57. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26394978 [accessed 19/04/2018].
Harding, A., Wareham, N. J. and Bingham, S. A. (2008) Plasma vitamin c level, fruit and vegetable consumption, and the risk of new-onset type 2 diabetes mellitus: The european prospective investigation of cancer–norfolk prospective study. Archives of Internal Medicine, 168 (14), 1493-1499. Available from: http://dx.doi.org/10.1001/archinte.168.14.1493 [accessed 29/05/2018].
Hassanein, M., Al-Arouj, M., Hamdy, O., Bebakar, W. M. W., Jabbar, A., Al-Madani, A., Hanif, W., Lessan, N., Basit, A., Tayeb, K., Omar, M. A. K., Abdallah, K., Al Twaim, A., Buyukbese, M. A., El-Sayed, A. A. and Ben-Nakhi, A. (2017) Diabetes and Ramadan: Practical guidelines. Diabetes Research and Clinical Practice, 126 303-316. Available from: http://www.sciencedirect.com/science/article/pii/S0168822717303388 [accessed 30/05/2018].
Hawthorne, K. (1994) Accessibility and Use of Health Care Services in the British Asian Community. Family Practice, 11 (4), 453-459. Available from: http://dx.doi.org/10.1093/fampra/11.4.453 [accessed 29/05/2018].
Hawthorne, K. (2001) Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Educ Res, 16 (3), 373-381. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11497119 [accessed 29/05/2018].
Hawthorne, K. and Tomlinson, S. (1999) Pakistani moslems with Type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control. Diabet Med, 16 (7), 591-597. Available from: https://www.ncbi.nlm.nih.gov/pubmed/10445836 [accessed 29/05/2018].
Holman, N., Young, B. and Gadsby, R. (2015) Current prevalence of Type 1 and Type 2 diabetes in adults and children in the UK. Diabet Med, 32 (9), 1119-1120. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25962518 [accessed 08/05/2018].
Hu, F. B., Manson, J. E., Stampfer, M. J., Colditz, G., Liu, S., Solomon, C. G. and Willett, W. C. (2001) Diet, Lifestyle, and the Risk of Type 2 Diabetes Mellitus in Women. New England Journal of Medicine, 345 (11), 790-797. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa010492 [accessed 08/05/2018].
IDF. (2017). Diabetes Atlas – 8th Edition [online]. Available from: http://www.diabetesatlas.org [accessed 08/05/2018].
Joshi, P., Islam, S., Pais, P., Reddy, S., Dorairaj, P., Kazmi, K., Pandey, M. R., Haque, S., Mendis, S., Rangarajan, S. and Yusuf, S. (2007) Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. Jama, 297 (3), 286-294. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17227980 [accessed 28/05/2018].
Kassam-Khamis, T., Judd, P. A. and Thomas, J. E. (2000) Frequency of consumption and nutrient composition of composite dishes commonly consumed in the UK by South Asian Muslims originating from Bangladesh, Pakistan and East Africa (Ismailis). J Hum Nutr Diet, 13 (3), 185-196. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12383125 [accessed 29/05/2018].
Kearney, M. (2017). How effective is the NHS Health Check? [online]. Available from: https://www.england.nhs.uk/blog/matt-kearney-8/ [accessed 29/05/2018].
Khanam, S. and Costarelli, V. (2008) Attitudes towards health and exercise of overweight women. Journal of the Royal Society for the Promotion of Health, 128 (1), 26-30. Available from: https://doi.org/10.1177/1466424007085225 [accessed 30/05/2018].
Khunti, K., Kumar, S. and Brodie, J. (2009). Diabetes UK and South Asian Health Foundation recommendations on diabetes research priorities for British South Asians [online]. Available from: https://www.diabetes.org.uk/resources-s3/2017-11/south_asian_report.pdf [accessed 28/05/2018].
Khunti, K., Stone, M. A., Bankart, J., Sinfield, P. K., Talbot, D., Farooqi, A. and Davies, M. J. (2007) Physical activity and sedentary behaviours of South Asian and white European children in inner city secondary schools in the UK. Family Practice, 24 (3), 237-244. Available from: http://dx.doi.org/10.1093/fampra/cmm013 [accessed 30/05/2018].
Kolt, G. S., Schofield, G. M., Rush, E. C., Oliver, M. and Chadha, N. K. (2007) Body fatness, physical activity, and nutritional behaviours in Asian Indian immigrants to New Zealand. Asia Pac J Clin Nutr, 16 (4), 663-670. Available from: http://apjcn.nhri.org.tw/server/APJCN/16/4/663.pdf [accessed 29/05/2018].
Lawton, J., Ahmad, N., Hallowell, N., Hanna, L. and Douglas, M. (2005) Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. BMJ, 330 (7502), 1247-1251. Available from: https://www.bmj.com/content/bmj/330/7502/1247.full.pdf [accessed 30/05/2018].
Lawton, J., Ahmad, N., Hanna, L., Douglas, M., Bains, H. and Hallowell, N. (2008) ‘We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethnicity & Health, 13 (4), 305-319. Available from: https://doi.org/10.1080/13557850701882910 [accessed 29/05/2018].
Lawton, J., Ahmad, N., Hanna, L., Douglas, M. and Hallowell, N. (2006) ‘I can’t do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Education Research, 21 (1), 43-54. Available from: http://dx.doi.org/10.1093/her/cyh042 [accessed 29/05/2018].
Lear, J. T., Lawrence, I. G., Burden, A. C. and Pohl, J. E. (1994) A comparison of stress test referral rates and outcome between Asians and Europeans. Journal of the Royal Society of Medicine, 87 (11), 661-662. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1294930/ [accessed 29/05/2018].
Lee, T. W., Lee, S. H., Kim, H. H. and Kang, S. J. (2012) Effective Intervention Strategies to Improve Health Outcomes for Cardiovascular Disease Patients with Low Health Literacy Skills: A Systematic Review. Asian Nursing Research, 6 (4), 128-136. Available from: http://www.sciencedirect.com/science/article/pii/S197613171200062X [accessed 03/06/2018].
Lovegrove, J. A. (2007) CVD risk in South Asians: the importance of defining adiposity and influence of dietary polyunsaturated fat. Proc Nutr Soc, 66 (2), 286-298. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17466109 [accessed 28/05/2018].
McKeigue, P. M., Adelstein, A. M., Shipley, M. J., Riemersma, R. A., Marmot, M. G., Hunt, S. P., Butler, S. M. and Turner, P. R. (1985) Diet and risk factors for coronary heart disease in asians in Northwest London. The Lancet, 326 (8464), 1086-1090. Available from: http://dx.doi.org/10.1016/S0140-6736(85)90684-1 [accessed 20/05/2018].
McMillan, S. S., Kendall, E., Sav, A., King, M. A., Whitty, J. A., Kelly, F. and Wheeler, A. J. (2013) Patient-Centered Approaches to Health Care: A Systematic Review of Randomized Controlled Trials. Medical Care Research and Review, 70 (6), 567-596. Available from: https://doi.org/10.1177/1077558713496318 [accessed 19/04/2018].
Misra, A., Khurana, L., Isharwal, S. and Bhardwaj, S. (2009) South Asian diets and insulin resistance. Br J Nutr, 101 (4), 465-473. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18842159 [accessed 28/05/2018].
Murray, M. D., Young, J., Hoke, S., Tu, W., Weiner, M., Morrow, D., Stroupe, K. T., Wu, J., Clark, D., Smith, F., Gradus-Pizlo, I., Weinberger, M. and Brater, D. C. (2007) Pharmacist intervention to improve medication adherence in heart failure: A randomized trial. Annals of Internal Medicine, 146 (10), 714-725. Available from: http://dx.doi.org/10.7326/0003-4819-146-10-200705150-00005 [accessed 02/06/2018].
Ness, A. R., Cappuccio, F. P., Atkinson, R. W., Khaw, K. T. and Cook, D. G. (1999) Plasma vitamin C levels in men and women from different ethnic backgrounds living in England. Int J Epidemiol, 28 (3), 450-455. Available from: https://www.ncbi.nlm.nih.gov/pubmed/10405847 [accessed 29/05/2018].
NHS. (2015). Understanding diabetes in London [online]. Available from: http://www.londonscn.nhs.uk/wp-content/uploads/2015/02/dia-understanding-ldn-challenges-022015.pdf [accessed 08/05/2018].
NHS. (2018). Explore NHS Health Check Data [online]. Available from: https://www.healthcheck.nhs.uk/commissioners_and_providers/data/ [accessed 29/05/2018].
NICE. (2015). Type 2 diabetes in adults: management [online]. Available from: https://www.nice.org.uk/guidance/ng28 [accessed 08/05/2018].
Pierce, M. B., Zaninotto, P., Steel, N. and Mindell, J. (2009) Undiagnosed diabetes-data from the English longitudinal study of ageing. Diabet Med, 26 (7), 679-685. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19573116 [accessed 08/05/2018].
Public Health England. (2015a). Diabetes prevalence estimates for local populations [online]. Available from: https://www.gov.uk/government/publications/diabetes-prevalence-estimates-for-local-populations [accessed 08/05/2018].
Public Health England. (2015b). A systematic review and meta- analysis assessing the effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes mellitus in routine practice [online]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/456147/PHE_Evidence_Review_of_diabetes_prevention_programmes-_FINAL.pdf [accessed 30/05/2018].
Public Health England. (2018). NHS Health Checks: applying All Our Health [online]. Available from: https://www.gov.uk/government/publications/nhs-health-checks-applying-all-our-health/nhs-health-checks-applying-all-our-health [accessed 29/05/2018].
Radhika, G., Sudha, V., Mohan Sathya, R., Ganesan, A. and Mohan, V. (2008) Association of fruit and vegetable intake with cardiovascular risk factors in urban south Indians. Br J Nutr, 99 (2), 398-405. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17678569 [accessed 29/05/2018].
Ramachandran, A., Snehalatha, C., Mary, S., Mukesh, B., Bhaskar, A. D. and Vijay, V. (2006) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia, 49 (2), 289-297. Available from: https://doi.org/10.1007/s00125-005-0097-z [accessed 29/05/2018].
Robson, J., Dostal, I., Madurasinghe, V., Sheikh, A., Hull, S., Boomla, K., Griffiths, C. and Eldridge, S. (2017) NHS Health Check comorbidity and management: an observational matched study in primary care. The British Journal of General Practice, 67 (655), 86-93. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5308122/ [accessed 30/05/2018].
Robson, J., Dostal, I., Madurasinghe, V., Sheikh, A., Hull, S., Boomla, K., Page, H., Griffiths, C. and Eldridge, S. (2015) The NHS Health Check programme: implementation in east London 2009–2011. BMJ Open, 5 (4), e007578. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4401839/ [accessed 30/05/2018].
Robson, J., Dostal, I., Sheikh, A., Eldridge, S., Madurasinghe, V., Griffiths, C., Coupland, C. and Hippisley-Cox, J. (2016) The NHS Health Check in England: an evaluation of the first 4 years. BMJ Open, 6 (1), e008840. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4735215/ [accessed 30/05/2018].
Sahota, O., Boff, A., Dismore, A., Malthouse, K. and Twycross, F. (2014). Blood Sugar Rush: Diabetes time bomb in London [online]. Available from: https://www.london.gov.uk/sites/default/files/gla_migrate_files_destination/Diabetes%20report_0.pdf [accessed 08/05/2018].
Schellenberg, E. S., Dryden, D. M., Vandermeer, B., Ha, C. and Korownyk, C. (2013) Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med, 159 (8), 543-551. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24126648 [accessed 08/05/2018].
Sriskantharajah, J. and Kai, J. (2007) Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Family Practice, 24 (1), 71-76. Available from: http://dx.doi.org/10.1093/fampra/cml066 [accessed 30/05/2018].
Stevens, A., Raftery, J., Mant, J. and Simpson, S. (2006) Health Care Needs Assessment: The Epidemiologically Based Needs Assessment Reviews. 1st edition. Abingdon, UK, CRC Press.
Stumvoll, M., Goldstein, B. J. and van Haeften, T. W. (2005) Type 2 diabetes: principles of pathogenesis and therapy. Lancet, 365 (9467), 1333-1346. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15823385?dopt=Abstract&holding=npg [accessed 27/05/2018].
Thompson, K., Kearney, M., Deanfield, J., Iqbal, Z., Newton, J. and Greaves, F. (2017). Emerging evidence on the NHS Health Check: findings and recommendations [online]. Available from: https://www.healthcheck.nhs.uk/document.php?o=1293 [accessed 30/05/2018].
Zheng, Y., Ley, S. H. and Hu, F. B. (2017) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nature Reviews Endocrinology, 14 88-98. Available from: http://dx.doi.org/10.1038/nrendo.2017.151 [accessed 08/05/2018].
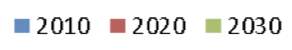
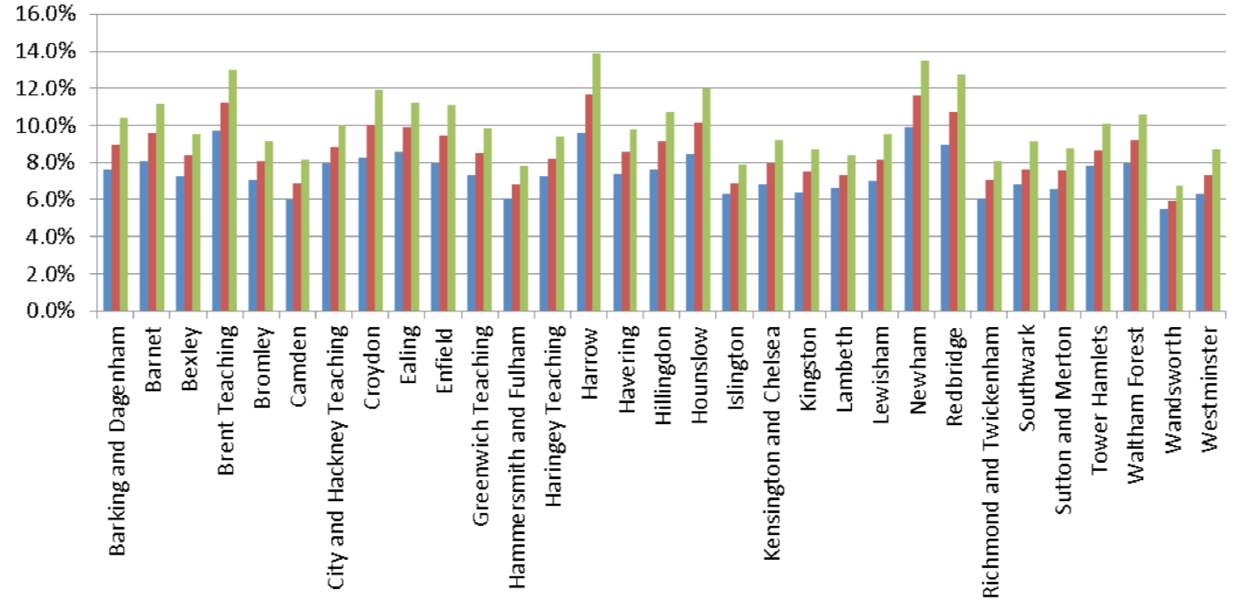
Figure 1. Diabetes prevalence by areas of London for 2010, and predictions for 2020 and 2030 (NHS, 2015).
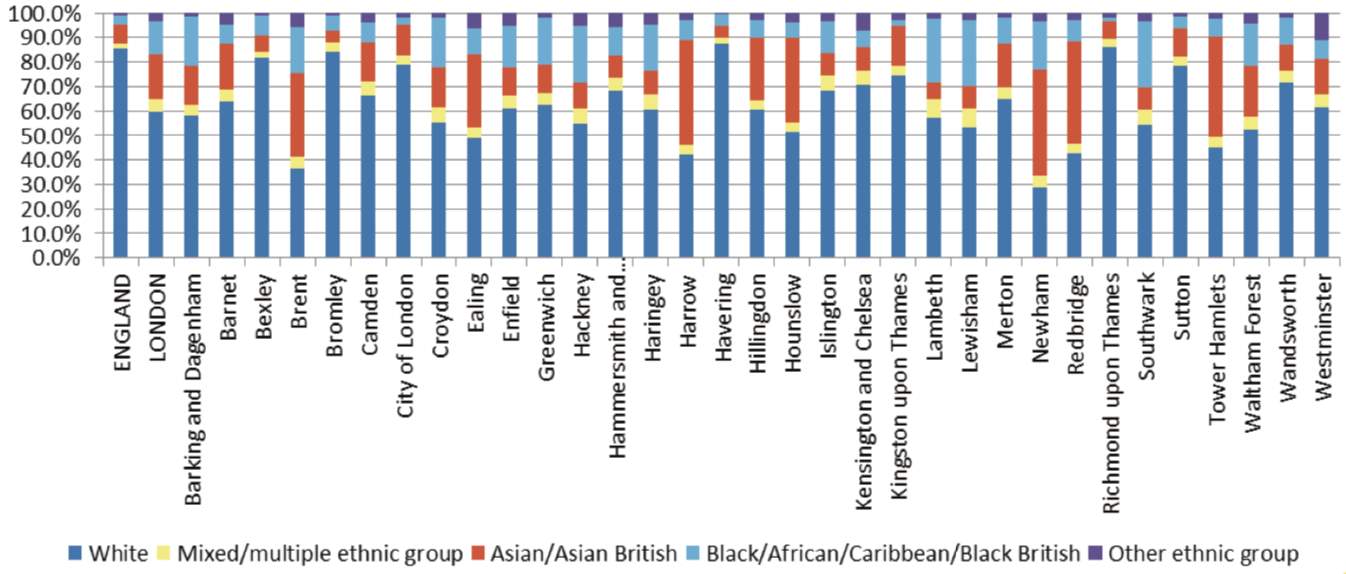
Figure 2. Ethic diversity of London by borough (NHS, 2015).
Figure 3. Socioeconomic deprivation in London by levels of deprivation indices (NHS, 2015).
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Diabetes"
Diabetes is a metabolic disorder that results in an abnormally high blood glucose level. Blood glucose levels are controlled by insulin produced by the pancreas. In diabetics, the pancreas either doesn’t produce enough (or any) insulin, or the body does not respond sufficiently to the insulin that the pancreas produces.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




