Unstable Angina Diagnosis and Management
Info: 3169 words (13 pages) Dissertation
Published: 9th Dec 2019
Tagged: Medical
Coronary artery disease is a major cause of death in the United States. Coronary artery disease is defined as an established pattern of angina pectoris, a history of myocardial infarction or the presence of plaque documented by catheterization (Buttaro et al:2017). Unstable angina is a clinical syndrome that is a subset of acute coronary syndrome. The acute coronary syndrome is usually, but not always, caused by atherosclerotic coronary artery disease and is associated with a high risk of myocardial infarction and death. The acute coronary syndrome includes unstable angina, NSTEMI, and STEMI. In the spectrum of acute coronary syndrome unstable angina is defined by electrocardiographic (ECG) ST-segment depression or prominent T-wave inversion in an appropriate clinical setting (chest discomfort or angina equivalents)at the time of presentation ( 2014 Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2014). Angina equivalents include nausea, vomiting, dyspnea, diaphoresis, and dizziness. The angiographic studies show that unstable angina usually results from the disruption or erosion of an atherosclerotic plaque and the following series of pathophysiological processes that decrease the coronary blood flow. The timely diagnosis and management of these patients must start from all the information available at times of the first presentation to the clinic.
Epidemiology of Unstable Angina
The epidemiology of a disease is usually measured in terms of incidence and prevalence among the targeted population. This usually measures the disease burden in the population. At the beginning of the 20th-century heart disease was not a common cause of death in the United States. During the mid-century, the incidence of heart disease rose up considerably and reached the leading cause of death. Coronary atherosclerosis with resultant atherosclerosis was the main reason for deaths associated with heart diseases. The major risk factors for the rise in heart disease were increased in smoking, widespread consumption of unhealthy diet and sedentary lifestyle. Although the mortality rate from this condition has generally declined over the past twenty years in the US, it still continues to be a cause of about one-third of the death among people older than 35 years. The prevalence of heart disease increases with age for both men and women. The 2016 heart disease and stroke statistics update of the American heart association has recently reported that 15.5 million persons of more than or equal to twenty years of age in the united states have coronary heart disease. It has been estimated that approximately every 42 seconds, an American will suffer from myocardial infarction. Americans with two or major risk factors, the lifetime risk of developing coronary heart disease is 37.5% for men and 18.3% for women. Cardiovascular disease mortality and complications have been declining in the USA with the advancement of medical care and early detection and the implementation of preventive services in primary care. The increased awareness of the warning signs and symptoms of coronary artery disease among the people also helped to reduce the mortality rate(Sanchis-Gomar et al., 2016).
Pathophysiology of Unstable Angina
Among the one million populations who are admitted to the hospital or goes to the clinic with presentations of the acute coronary syndrome, approximately 70% do not have ST elevation as initial EKG. These patients are further classified based on the presence of elevated troponin into NSTEMI (non-ST-segment elevated MI) in which cardiac injury is sufficient enough to cause biomarker release or UNSTABLE ANGINA without elevated troponin. These both groups may or may not have other pathologic EKG changes suggestive of ischemia such ST-segment depression or onset T-wave inversion. This is primarily caused by a non-occlusive thrombus that partially interrupts perfusion. This cause a change in the supply and demand balance of coronary perfusion and myocardial oxygen consumption. The pain pattern is of increasing frequency and duration of angina episodes depending on the demand and it also occurs at rest. If left untreated, the risk of progression to acute myocardial infarction is very high. Other than atherosclerotic cause, nonobstructive causes such as anemia, sepsis, transient coronary vasospasm, and endocardial dysfunction also can lead to the same clinical presentation because of the excessive myocardial demand or reduced coronary supply (Buttaro, et al.,2017). The clinical presentation of unstable includes S3 if LV dysfunction present, S4, the transient mitral regurgitation /murmur or-or presence of a carotid arterial bruit. Others include JVD, pallor, cool and diaphoretic skin, crackles on auscultation, edema of the extremities and low-grade fever. In typical angina, it meets the three following criteria which include substernal chest discomfort of characteristic quality and duration, provoked by exertion or emotional stress and is relieved by rest and /or NTG. On the other hand, atypical angina only presents with two of the above characteristics. Whereas in non-cardiac chest pain meets one or none of the above characteristics.
Differential diagnosis of unstable angina
GERD: Gerd is presented with a set of classical symptoms such as heartburn, regurgitation, and dysphagia. In addition to these typical symptoms, it can cause other symptoms such as coughing, chest pain, and wheezing. (Buttaro; et al., 2017)
Esophageal spasm: These are painful contractions within the esophagus. It can feel like sudden severe chest pain that lasts for a few minutes. (Buttaro et al.,2017)
Biliary colic: A person with biliary colic typically feels the pain in the middle right upper abdomen. The pain can feel like sharp, crampy or a constant dull ache. Colic usually occurs in the evening or after a heavy meal. (Buttaro et al.,2017)
Anxiety or panic attacks: People with panic attacks usually experience a racing heart, feeling dizzy, tremors, sweating, chest pains, breathing difficulties and feeling the loss of control. They usually have a history of panic attacks. (Buttaro et al., 2017)
Costochondritis: In this, the patient usually feels dull pain or sharp in the front chest wall. The reproducible tenderness one feels when we press on the rib joints is a constant feature of costochondritis. (Buttaro et al., 2017)
Braunwald Classification of unstable angina.
There are two types of classification of unstable angina based on severity and the cause of the disease. Based on the severity it is classified as class1, class 2 and class3.In class, 1there is the new onset of severe angina, but no pain at rest usually happens with exertion. In class 2 there is angina at rest within the past month but not within the past 48 hours. In class 3 there is acute angina at rest within 48 hours. Based on the precipitating factors it is classified into primary, secondary (from fever, hypoxia, and anemia) and post infarction MI (which occurs 2 weeks after myocardial infarction). (Buttaro; et al., 2017). The prognosis of the unstable angina is patient specific. Early detection and modification of the risk factors is a crucial factor in the prognosis. Current management with antiplatelet, ACE Inhibitors and Beta blockers seem to have resulted in a positive long-term outcome in patients with unstable angina.
Clinical implications
Coronary artery disease is a growing epidemic in the United States. It affects both men and women and its incidence starts as early as in the 20s in US population. Since acute coronary syndrome consists of unstable angina, non-ST-segment elevation MI and ST-segment elevation MI, the awareness of the provider in treatment decision making is critically important. Patients with chest pain account for a majority of the patients in the primary care setting. Myocardial injury and infarction are irreversible but myocardial ischemia is reversible. Since time is very critical in the intervention modalities it is very important as providers to understand the typical and atypical presentation of unstable angina and other ACS. Most of the patient who develops cardiac complications usually have one risk factor which can be picked up by the primary care visits. Because of its incidence, it is very important for the provider to know the management of unstable angina.
Diagnostic tests
CBC: Usually to identify anemia, any source of infection, inflammation and to rule out sepsis.
ESR: To rule out any inflammation
Fasting lipid profile: Including TC, LDL, HDL, and triglycerides. Hyperlipidemia is a cause of coronary artery disease. This blood test can identify the risk for atherosclerosis and can treat accordingly.
Fasting glucose: Diabetes is a major risk factor for coronary artery disease. It can go undiagnosed in many patients and it can hide the typical presentation of the acute coronary syndrome.
Thyroid function test: The prognosis of acute coronary syndromes is affected by many factors. Alteration in thyroid hormone plasma concentration, especially low triiodothyronine (T3) levels, represent a hormonal imbalance that usually occurs in patients with acute coronary syndrome. This abnormal thyroid hormonal level is related to worse prognosis.
Chest x-ray: If there are any signs and symptoms of heart failure such as orthopnea, dyspnea on exertion, elevated jugular vein distension, bilateral lower extremity edema x-ray confirmation is necessary to rule out heart failure.
Electrolytes: Electrolytes such as calcium, magnesium, and potassium play a major role in cardiac muscle function. Electrolyte imbalance is maximally seen in calcium. Hypocalcemia, hypokalemia, and hyponatremia are usually present in patients with acute coronary syndrome
12 lead EKG: Usually no ST elevation is seen in unstable angina. Unstable angina is considered to be present in patients with ischemic symptoms suggestive of an ACS with or without EKG changes. The EKG changes usually if present are ST-segment depression or transient elevation or new T wave inversion.
Echocardiogram: This can be performed as an outpatient if the patient is stable enough.
Cardiac catheterization with angiography is performed in patients with a TIMI score of 0-3. This is done in inpatient settings.
Myoglobin: It is the earliest serum marker available but false elevations are possible.
Troponin I and T: It is highly sensitive and specific. Begins to rise 3-4 hours after the onset of pain and peaks up to 18-36 hours. False elevations are also possible.
Creatinine Kinase (CK): CK MB is highly suggestive of myocardial injury. It is released from the injured heart muscles. Calculate the ratio of CK and CK MB
Treatment of unstable angina.
A vigilant effort must be made to differentiate other causes of increased myocardial oxygen demand such as thyrotoxicosis, tachyarrhythmia, exacerbation of preexisting heart failure and anemia. Timely treatment of these conditions may reduce the pain at rest. Any coexisting stress from life events also collected from the patients. Because in some situations mild sedation or removal from an emotionally disturbing situation must be needed. The confidence of the practitioner in her ability to cope with the uncertainty of the nature and course of the unstable angina is of very important. A number of drugs have seemed to be effective in the treatment of unstable angina. It is up to the provider to decide which is the best option for his patient based on the best evidence practice guidelines.
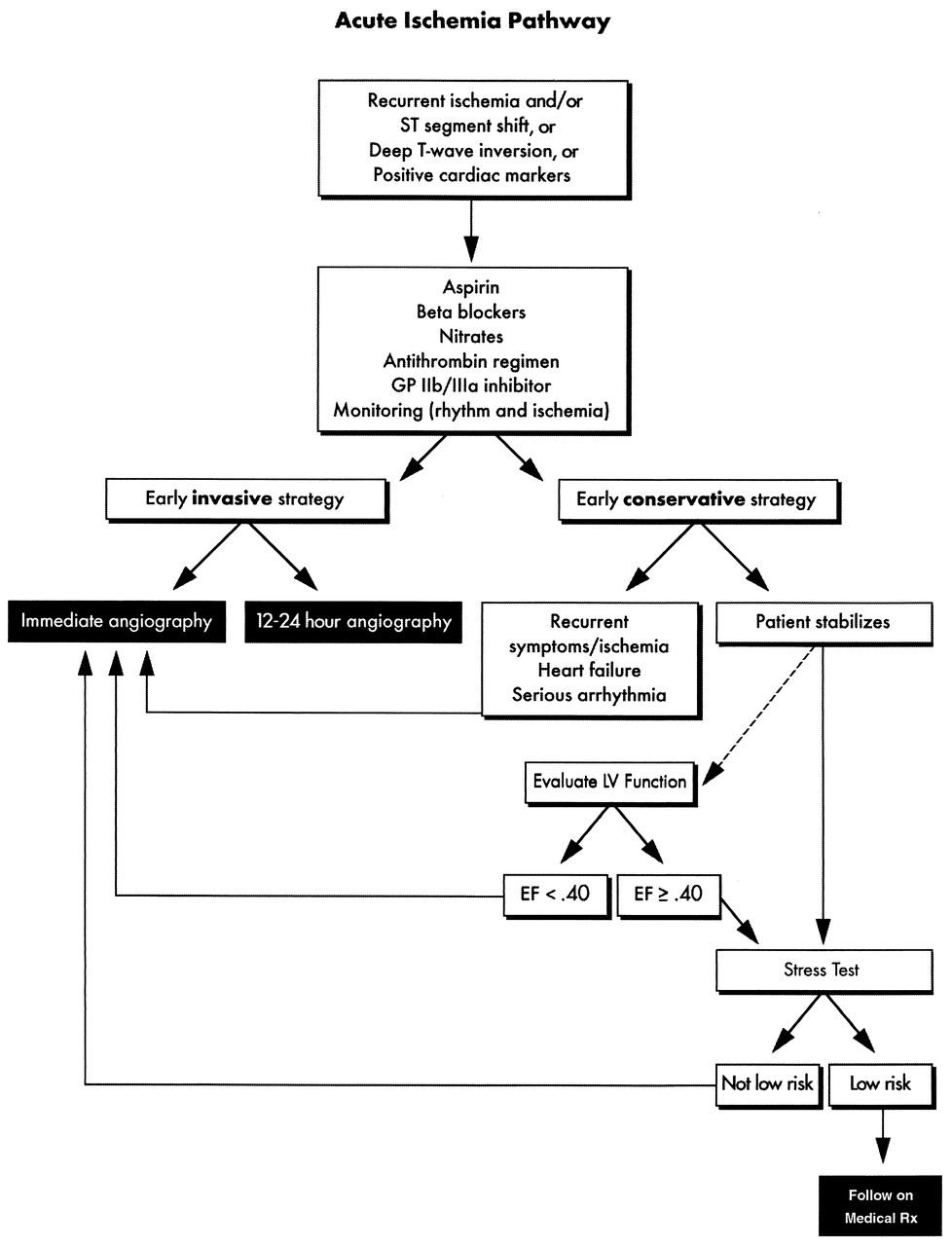
Drug Treatment:
The major drug class in the management of unstable angina includes nitrates, antihypertensive agents, antihyperlipidemic agents, and antiplatelet agents. Patients with oxygen saturation of less than 90% or at risk of developing hypoxemia should be treated with supplemental oxygen. The first drug of choice in ischemia is nitrates. Nitrates lead to coronary vasodilation and also cause peripheral vasodilation. It reduces the myocardial oxygen consumption by decreasing the preload and end diastolic volume. These can cause a headache and postural hypotension which can be managed with the adjustment of doses. This should be contraindicated in hypotension, right ventricular infarction and recent use of phosphodiesterase inhibitors. The next class of drug includes antiplatelet drugs. Chewable aspirin usually gives the rapid effect If the pain still persists after use of nitrates, morphine may be used. The vasodilation effect of morphine can reduce pain, blood pressure and congestive symptoms. This can also reduce the anxiety of the patients. Nitrates can be used as oral long-acting agents, sublingual tablets and also ointment. The next group of drugs that are used in the management of unstable angina is beta blockers. This reduces the myocardial oxygen consumption.It is contraindicated in active bronchospasm, hemodynamic instability, severe bradycardia, cocaine abuse, heart blocks greater than a first degree and decompensated heart failure. Cardio-selective beta –blockers (metoprolol and atenolol) are preferable because they act mainly on the beta -1 receptors and causes less bronchospasm than others. ACE inhibitors also can be used to significantly reduce morbidity and mortality. All the patients should receive high-intensity statins regardless of their LDL levels. The usual drug of choice is Atorvastatin 8o mg. (Button; et al., 2017).
Nonpharmacologic interventions.
Screening is one of the most important keys to preventing the occurrence of unstable angina and its progression to acute myocardial infarction. Usually, most of the patients who develop CAD one have at least risk factor. The risk modification strategy includes tobacco cessation, bringing down the body mass index to 18.5 -24.9, moderate intensity activity for 30-60 mins seven days per week, alcohol consumption in moderation (no more than 2 drinks for men and no more than one drink for women per day, low sodium diet (less than 1500gms/day and no addition at the table), 2-3 servings of fruits and vegetables per day and saturated fat less than 10% of daily calories.
Conclusions and Limitations
One of the studies I selected was on the diagnostic potential of plasmatic micro RNA in stable and unstable angina. This work showed that specific plasmatic microRNA has the potential to correctly identify patients with angiographically documented CAD. But the limitation was they failed to identify a plasmatic microRNA expression pattern that is able to differentiate stable and unstable angina. (D’Alessandro et al., 2013). The second study selected was the gender disparity, presentation and outcome management of patients with the acute coronary syndrome. The difference in this largely related to differences in prognostic variables and management pattern. The limitation is that the difference in the management pattern needs further study(Shahab et al., 2013). The next study was done on the predictive value of NLR (neutrophil to lymphocyte ratio) on the clinical outcome of patients with NSTEMI and unstable angina. The study showed that NLR is a strong independent predictor of 3-year mortality in patients with unstable angina. The limitation includes it was a single center and each patient is treated differently. Other inflammatory markers were not analyzed as it is very expensive. (Gul et al., 2014). Another study selected was direct intra-myocardial mesenchymal stromal injections in patients with refractory angina. The study showed an improvement in clinical symptoms and exercise tolerance. This study was not a dose titration study. (Haack-Sørensen et al., 2013).The last study selected was Effects of statin on circulating microRNAome and predicted function regulatory network in patients with unstable angina. This study showed that statins induce microRNA expression in unstable angina patient which plays an important role in signal pathways in the pathogenesis of unstable angina.No limitation was documented in the study. (“Effects of statin on circulating microRNAome and predicted function regulatory network in patients with unstable angina | BMC Medical Genomics | Full Text,” 2018.)
References
- 2014 ACC/AHA/AATS/PCNA/SCAI/STS Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease | JACC: Journal of the American College of Cardiology. (2014). Retrieved November 19, 2018, from http://www.onlinejacc.org/content/64/18/1929
- Buttaro TM, Trybulski J, Bailey PP, Sandberg-Cook J. Primary Care: A Collaborative Practice. 5th ed. St Louis, MO: Elsevier Mosby; 2017.
- D’Alessandra, Y., Carena, M. C., Spazzafumo, L., Martinelli, F., Bassetti, B., Devanna, P., … Pompilio, G. (2013). Diagnostic Potential of Plasmatic MicroRNA Signatures in Stable and Unstable Angina. PLOS ONE, 8(11), e80345. https://doi.org/10.1371/journal.pone.0080345
- Effects of statin on circulating microRNAome and predicted function regulatory network in patients with unstable angina | BMC Medical Genomics | Full Text. (2018). Retrieved November 10, 2018, from https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-015-0082-4
- Gul, M., Uyarel, H., Ergelen, M., Ugur, M., Isık, T., Ayhan, E., … Uslu, N. (2014). Predictive Value of Neutrophil to Lymphocyte Ratio in Clinical Outcomes of Non-ST Elevation Myocardial Infarction and Unstable Angina Pectoris: A 3-Year Follow-Up. Clinical and Applied Thrombosis/Hemostasis, 20(4), 378–384. https://doi.org/10.1177/1076029612465669
- Haack-Sørensen, M., Friis, T., Mathiasen, A. B., Jørgensen, E., Hansen, L., Dickmeiss, E., … Kastrup, J. (2013). Direct Intramyocardial Mesenchymal Stromal Cell Injections in Patients with Severe Refractory Angina: One-Year Follow-Up. Cell Transplantation, 22(3), 521–528. https://doi.org/10.3727/096368912X636830
- Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of coronary heart disease and acute coronary syndrome. Annals of Translational Medicine, 4(13). https://doi.org/10.21037/atm.2016.06.33
- Shehab, A., Al-Dabbagh, B., AlHabib, K. F., Alsheikh-Ali, A. A., Almahmeed, W., Sulaiman, K., … Amin, H. (2013). Gender Disparities in the Presentation, Management and Outcomes of Acute Coronary Syndrome Patients: Data from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2). PLOS ONE, 8(2), e55508. https://doi.org/10.1371/journal.pone.0055508
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Medical"
The word Medical refers to preventing or treating injuries or illnesses, relating to the study or practice of medicine. Medical care involves caring for a patient and helping them through their journey to recovery.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




