Types of Stroke and Risk-Factors
Info: 3459 words (14 pages) Dissertation
Published: 10th Dec 2019
- Stroke is a leading cause of adult disability. Describe the pathological sub-types of stroke, including relevant risk factors, and differences in their outcomes. (50%)
Based on their main pathological background, strokes can be classified into the ischemic and haemorrhagic stroke.
Ischaemic strokes (infarction) are caused by the occlusion of arteries that perfuse the brain either by thrombosis or emboli. The occlusion then results in ischemia of all areas that supplied by the occluded arteries. The blockage can be at the main atherosclerotic vessels or to distal areas where the emboli travel to.
Haemorrhagic strokes are caused by a spontaneous bleed in the brain which results in haematoma, oedema, and compression of the brain contents. Most of the cases are due to arteriolar hypertensive, advanced age, coagulation disorders or diet (excessive alcohol consumption). In elderly, cortical amyloid angiopathy (the result of high blood pressure) is one of the pathological causes of stroke occurring in elderly. The rate of the disorder increased as the population become older. In more severe cases, due to the compression of the brain substances by oedema, coma or even death may occur. (1)
There are several ways to categorize Ischaemic stroke, such as categorization based on pathological mechanism of stroke; aetiological, location and size of the stroke; and the sign and symptoms. None of the stroke classification is perfect whatsoever. The categorization based on pathological mechanism such as the International Classification of Diseases of World Health Organization and Trial of ORG 10172 in acute stroke treatment (TOAST) can be expensive and time consuming because it requires an extensive investigation before deciding the type of stroke. (2) Therefore, this essay will focus on the ischaemic stroke sub-categories defined by Oxfordshire Community Stroke Project (OCSP) study, classification based on initial clinical manifestation which offers a simplicity, speed and does not require extensive diagnosis. However, it should be noted that some of the limitations by using OCSP are including: (1) information disease aetiology and pathophysiology which is crucial when determining appropriate treatment and management to the patient is lacking (2, 3), (2) may fail to distinguish small cortical infarction and lacunar infarction stroke(4)
The Ischaemic stroke can be divided into 4 sub-categories based on OSCP scheme, which are: Lacunar infarcts (LACI), Total anterior circulation infarcts (TACI), Partial anterior circulation infarcts (PACI) and Posterior circulation infarcts (POCI).(5) Although the classification is based on presenting signs and symptoms, each sub-category is labelled anatomically, indicating the relation between anatomical location of cerebral infarction and presenting signs and symptoms.(6)
- LACI
Patients show a pure motor stroke, sensory-motor stroke, or ataxic hemiparesis. Patients with faciobrachial involvement are included in this classification. (5)However, those with restricted deficit are excluded. Due to their small size and location, LACI usually do not affect cortical function. (1)Lacunar stroke is caused by a small lacunar infarct within basal ganglia or pons. In cases that lacunar syndrome was not accompanied with lacunar infarct, it is suggested that the syndrome may arise from a lesion involving right hemisphere. Disorder affecting basal perforating artery such as arteriolar lipohyalinosis or by microatheroma are thought to be the underlying cause of lacunar infarcts. Several proposed causes of lacunar infarcts are: embolism, hypertension, small-vessel occlusive disease, hematologic disorder, small intracerebral haemorrhages and vasospasm. (5)
- TACI
Signs and symptoms accompanied this category are higher cerebral dysfunction (i.e. dysphasia, dyscalculia, visuospatial disorder); homonymous visual defect; and ipsilateral motor and/or sensory deficit of at least two areas of the face, arm, and leg. If the patient executive function cannot be assessed due to impaired consciousness, a deficit can be assumed. TACIs are associated with ischemia in deep and superficial areas supplied by middle cerebral artery (MCA). In TACI, patients showed a more complete clinical syndrome than those with more restricted disorders (i.e. LACI or PACI). Using radiologic imaging, occlusion of MCA is mostly due to either embolism or thrombus with ratio of 2 to 1. Thrombus usually derive from a more proximal vessel, specifically in the internal carotid artery (ICA). Most TACI patients have high mortality rate (5)
- PACI
Patients show two of the three components of TACIs syndrome, which either the impairment of higher cerebral function alone or a more restricted sensory/motor defect (i.e disorder only affect one of the limb, face, or hand and not the whole arm). The underlying cause of PACI is the cortical infarct because of blockage within the upper (no visual involvement) or lower (no motor/sensory deficit) area supplied by MCA. This sub-type of stroke also include infarct within areas vascularized by ACA as well as the striatocapsular infarctions, which may result from blockage in the MCA stem which supply smaller penetrating branches of lenticulostriate arteries by a thrombus. Most infarctions that happen in distal branch of artery are caused by caused either by a cardiogenic emboli or arterial embolic spread. The occurrence of infarct within frontoparietal border zone is thought to be caused by the occlusion of more proximal vessels in which supplying the deep perforating vessels.(5)
- POCI
POCI patients presented any signs of ipsilateral cranial nerve palsy, bilateral motor and/or sensory deficit, conjugate gaze palsy, and homonymous visual field defect. The cause of this disorder is due to any blockage by thrombus or emboli on blood vessels supplying the brainstem, cerebellum, and occipital lobes. Embolism is proposed to be the main cause of pure occipital lobe syndrome, while non-embolic infarction is due to atheroma in the main vessel which give branch to circumferential artery or failure of collateral vessels to perfuse due to more proximal blockage. (5)
Haemorrhagic stroke types:
- Aneurysmal Subarachnoid Haemorrhage
This type of haemorrhagic stroke is caused by the rupture of cerebral aneurysm which consequently fills the subarachnoid space with blood. Subarachnoid space is the location where the cerebrospinal fluid and trabeculae are normally found. The bleeding may extend to other areas such as basal cistern, ventricles, and spinal subarachnoid space. An aneurysm is a bulge at the site of weakness within the blood vessel walls. Most cerebral aneurysm are berry aneurysm and mainly located in the anterior circulation specifically at the anterior bifurcations and junctions of blood vessels such as in the circle of Willis. The aneurysm is thought to arise from a congenital defect in the muscular wall of the affected vessels. The disorder is higher in people with certain diseases. E.g. Polycystic kidney disease, fibromuscular dysplasia, and arteriovenous malformation of the brain. Mortality and morbidity of subarachnoid haemorrhage are high, with only one-third of people survive after the haemorrhage.(1)
- Arteriovenous Malformations
Is a disorder in which the arteries and veins are abnormal and linked by one or more fistula. The vascular networks lack of capillary bed and the small arteries do not have muscular layer. It is suggested that the problem may be due to failure in the development of cerebral capillary network during embryonic development. As the child’s brain grow, the thin-walled vessels enlarged to meet the demand of blood supply in the brain. The vessels tangled and shunt the blood from the high-pressure arterial circulation to the low-pressure venous system. Thus, the draining venous circulation that responsible only as draining system receive high-pressure blood, prone to rupture and causing haemorrhage. (1)
Generally, the risk factors of stroke can be classified into modifiable and non-modifiable factors.
The non-modifiable factors are age, sex, race, prior stroke history, and family history. The incidence of stroke increases with age. Although men have an increased risk to get a stroke at a younger age, more women die from stroke each year because women tend to live longer than men. Increased risk of stroke and mortality rates are also found in the Blacks, Hispanic/Latino American than in whites. Prior heart disease especially atrial fibrillation and other disorders that predispose to clot formation on cardiac wall, increasing cardioembolic stroke risk. Polycythemia, sickle cells disease and blood diseases can form a clot and cause blockage in cerebral vessels.
Modifiable risk factors include obesity, sedentary behaviour, excessive alcohol intake, illicit substance abused and oral contraceptive use. Although the excessive alcohol intake may increase the risk of stroke, light to moderate intake of alcohol reduces the risk. Several drugs abuse such as cocaine, amphetamines, and heroin are associated with cerebral haemorrhages(1). Furthermore, there is a strong correlation between genetic abnormality and stroke, such as in patients with Fabry disease. Fabry disease is a lysosomal storage disorder that can be inherited following X-link pattern. Such disorder is caused by a mutation in a gene encoded for lysosomal hydrolase α-galactosidase A (GLA) and result in accumulation of glycosphingolipids within vascular endothelium, smooth muscle cells, autonomic and dorsal root ganglia. It is thought that the lipid deposits may contribute to vessel occlusion and tissue infarction. Nevertheless, stroke risk factors such as hypertension, hypercholesterolemia, diabetes mellitus, hypercoagulopathy and cardiac disease may be eliminated through changing of lifestyle in conjunction with medical treatment.(7)
The outcomes showed by stroke patients are vary according to the stroke sub-category they belong to. In TACI patients, the possibility to have good functional outcome is low and high mortality. The mortality is due to the direct neurological injury caused by stroke on anterior circulation (i.e. transtentorial herniation). In contrast, PACI patients have lowest chance fatality, but they are more likely to develop an early recurrent stroke than the patients classified in other groups. LACI is shown to have mildest severity but many of the patients are handicapped if not treated correctly. POCI may cause death in stroke patients by damaging the vital structure of brainstem(5). Nevertheless, strokes outcome can also be predicted based on the speed of recovery. A study showed that although TACI is considered to have the most severe outcome, the patients may have significant recover if there is early recovery (after fourdays of treatment), indicating the importance of clinical classification and assessment of severity/impairment to predict prognosis and outcome (8)
Table 1. Outcomes by OCSP subtypes(2)
| TACI | PACI | LACI | POCI | |
| Mortality | ||||
| 30 days | 39% | 4% | 2% | 7% |
| 1 year | 60% | 16% | 11% | 19% |
| Dependence | ||||
| 30 days | 56% | 39% | 36% | 31% |
| 1 year | 36% | 29% | 28% | 19% |
| Recurrence | ||||
| 1 year | 6% | 17% | 9% | 20% |
- What types of specialised care do acute stroke units provide and is there evidence of benefit? (50%)
Stroke Unit is a specialised ward area where a multidisciplinary stroke team which consists of doctors, nurses, physiotherapists, occupational therapists, speech and language therapists, clinical/neuropsychologists, dieticians and social workers. The team may also receive input given by pharmacists, orthotics, orthoptists, and chiropodists. The stroke unit is linked closely to the department of radiology, neurosurgery, vascular surgery, neurology, geriatric medicine and cardiology. (9). The team is responsible to do a rapid specialist assessment (i.e. blood pressure, pulse, breathing rate, oxygen levels, conscious level and temperature), diagnosis (type of stroke, cause of the stroke), acute stroke treatment (i.e. thrombolysis), physiological and neurological monitoring and rehabilitation. The multidisciplinary team will work together with patients and their family to create a personalised holistic care. The team usually have a regular meeting where they would talk about patients’ update and treatment plan(9).
The major elements that comprised ward characteristics are: hospital setting (academic hospital or based at the same location as intensive care, neurosurgery, vascular surgery, and rehabilitation), unit setting (neurological beds equipped with at least two or more continuous electrocardiography monitor per ten beds), staffing per unit ward (full time physicians, nurses, and therapists), diagnostic tools ( availability of cranial CT scan, brain MRI scan, echocardiography, duplex ultrasound, and cerebral catheter angiography, for 24 hour, everyday), process of care (regular team meetings and early mobilization)(10)
Treatment of stroke by aetiology:
- The main treatment during ischaemic stroke is the administration of alteplase, a fibrinolytic drug. Administration of the drug is done by staff who have been trained and have good knowledge regarding stroke thrombolysis, contraindication of the drug and management of complication. Alteplase is critical to be given soon after the onset of stroke. Patients with acute ischaemic stroke should be considered to receive a combination of intravenous thrombolysis and thrombectomy, especially if they have a proximal intracranial artery occlusion which causing neurological decline(11). A meta-analysis has clearly shown the beneficial of endovascular thrombectomy to treat patients with anterior circulation ischaemic stroke is beneficial irrespective of patient characteristic such as elderly, alteplase ineligible patients, and patient who present later than 300 minutes after stroke onset. Also, the stroke patients who are diverse in geographical location has consistently showed reduced disability on the modified Ranking Scale (mRS) at 90 days(12). In cases when the ischaemic patients fulfil national clinical guidelines such as having a poor level of consciousness, suspected of middle artery infarction, and CT shown infarct of at 50% of MCA areas, then the decompressive hemicraniectomy may be performed.(11)
- Patients with intracerebral haemorrhage deteriorate quickly and should be sent to specialized stroke unit immediately. Patients with intracerebral haemorrhages who are taking vitamin K antagonist medication or anticoagulant drugs should urgently be administered a medication that reverses the anticoagulant effect in conjunction with prothrombin complex and/or intravenous vitamin K. Patients with intracerebral haemorrhage who present with high blood pressure may also be treated with blood pressure lowering medication. If the patients develop hydrocephalus, surgical intervention may be considered.(11)
- Acute stroke patients are often present acute neurological deficits and significant disturbance of pyrexia, hyperglycaemia, and hypoxia. A week after the onset of stroke, patients usually develop urinary sepsis and respiratory tract infection that required antibiotic treatment. Hence, patients with acute stroke should be admitted directly to hyperacute stroke unit to achieve and maintain normal physiological status and be assessed for such risk factors. (11)Stroke patients have a high risk to get affected by urinary incontinence and constipation. To prevent incontinence, patients should be trained for regular toileting. Whereas in constipation they may be given a laxative. Several things that will also be monitored carefully are the level of consciousness, hydration, nutrition, cardiac rhythm and rate. Swallowing difficulties are common in stroke patients and should be assessed. Those with swallowing difficulties will receive medication, food, and fluid in ways that will not cause aspiration (i.e. IV fluid/drug, nasogastric tube feeding)(9).
In the rehabilitation unit, early goal for management and therapy usually related with feeding, sitting balance and mobility. The main purpose of rehabilitation is to improve the overall quality of life. This is done by addressing problems such specific impairments, activity limitation and restriction in social participation and involving the family.(13)
According to meta-analysis review, the stroke patients who receive treatment in stroke unit have better prognosis by showing a likelihood to be alive, independent to return home after stroke than those who only receive treatment at the less-organised unit(14). When compared to the conventional ward, the stroke patients who treated in the stroke care unit have significantly higher survival rate than those in the conventional ward (figure 1). (10)
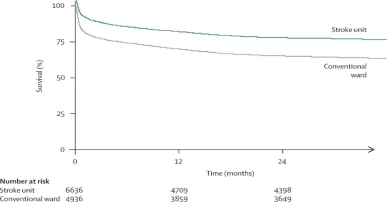
Figure 1. Survival rate of stroke patients who treated in stroke unit and conventional unit(10)
References:
1. Grossman SC, Porth CM. Porth’s Pathophysiology: Lippincott Williams and Wilkins; 2013. 1648 p.
2. Sims J, Koroshets WJ. Handbook of Stroke Prevention in Clinical Practice. Furie KL, Kelly PJ, editors: Humana Press; 2004.
3. Adams HP, Jr., Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke.24(1):35-41.
4. Asdaghi N, Jeerakathil T, Hameed B, Saini M, McCombe JA, Shuaib A, et al. Oxfordshire community stroke project classification poorly differentiates small cortical and subcortical infarcts. Stroke.42(8):2143-8.
5. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet.337(8756):1521-6.
6. Stevens A, Raftery J, Mant J, Simpson S. Health Care Needs Assessment: The Epidemiologically Based Needs Assessment 1ed: CRC Press; 2006 1 May 2006. 960 p.
7. Barrett KM, Meschia JF. Genetic stroke syndromes. CONTINUUM: Lifelong Learning in Neurology.20(2 Cerebrovascular Disease):399-411.
8. Sprigg N, Gray LJ, Bath PM, Lindenstrom E, Boysen G, De Deyn PP, et al. Stroke severity, early recovery and outcome are each related with clinical classification of stroke: data from the ‘Tinzaparin in Acute Ischaemic Stroke Trial’ (TAIST). Journal of the Neurological Sciences.254(1-2):54-9.
9. Rodgers H, Price C. Stroke unit care, inpatient rehabilitation and early supported discharge. Clinical Medicine, Journal of the Royal College of Physicians of London. 2017;17(2):173-7.
10. Candelise L, Gattinoni M, Bersano A, Micieli G, Sterzi R, Morabito A, et al. Stroke-unit care for acute stroke patients: an observational follow-up study. Lancet.369(9558):299-305.
11. National Clinical Guideline for Stroke, (2016).
12. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet.387(10029):1723-31.
13. Acute Stroke Unit: NHS North Bristol; [cited 2017 11 November]. Available from: https://www.nbt.nhs.uk/our-services/a-z-services/stroke-tia-services/acute-stroke-unit.
14. Stroke Unit Trialists C. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013(9):CD000197.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allRelated Content
All TagsContent relating to: "Neurology"
Neurology is the specialist branch of medicine that deals with the treatment of disorders of the nervous system. This means that neurologists concern themselves with issues affecting the brain, the nerves, and the spinal cord.
Related Articles
DMCA / Removal Request
If you are the original writer of this dissertation and no longer wish to have your work published on the UKDiss.com website then please:




